LW4: COMPOSITE "IN SITU" LYMPHOMAS – COEXISTENCE OF
advertisement

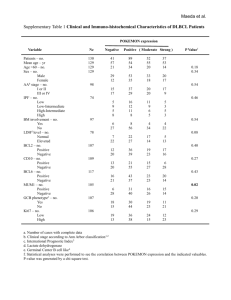
LW4: COMPOSITE "IN SITU" LYMPHOMAS – COEXISTENCE OF BOTH FOLLICULAR AND MANTLE CELL LYMPHOMA “IN SITU” Michele R Roullet1 and Adam Bagg2 1.Pathology 2.Hospital Sciences Medical Group/Eastern Virginia Medical School, Department of Pathology, Norfolk, VA, USA of the University of Pennsylvania, Department of Pathology and Laboratory Medicine, Philadelphia, PA, USA mrroullet33@gmail.com Clinical history: An 84-year-old woman with recurrent rectal carcinoma underwent splenectomy for multiple radiologically-detected splenic masses, presumed to represent metastatic carcinoma. The CBC was normal, apart from a mild lymphopenia. Details of biopsy & Histopathology: Spleen, 110 grams. The specimen was processed with standard formalin fixation. H&E histologic sections of the grossly appreciated nodules in the spleen revealed features consistent with grade 1-2 follicular lymphoma. Both the red and white pulp in the uninvolved (non-nodular) portions of the spleen were histologically unremarkable. Immunohistochemistry/immunophenotype: Immunohistochemical stains revealed that the nodules of histologically-evident follicular lymphoma contained CD20+ CD79a+ B-cells that were positive for CD10, CD23 and BCL6, but negative for BCL2, CD5, and CD43. The mantle zone lymphocytes, both those surrounding the follicles of follicular lymphoma, and in the histologically uninvolved white pulp of the spleen were cyclin D1positive. These cyclin D1-positive cells were confined to the mantle zones. The cyclin D1-positive cells did not coexpress CD5. While most of the CD10+ BCL6+ germinal centers in the uninvolved areas were BCL2-negative, a subset contained variable numbers of brightly BCL2-positive cells. Genetic/molecular analysis: FISH (on whole, non-microdissected tissue) using fusion probes was positive for a t(11;14)/CCND1/IGH@ fusion, but negative for t(14;18)/BCL2/IGH@. This tissue was also negative for a BCL6 translocation, using a break-apart probe. ImmunoFISH analysis, using break-apart probes for BCL2 and CCND1, was positive for split signals with BCL2 probes in CD10-positive cells and with the CCND1 probes in CD10-negative cells. No BCL2 break apart was evident in the CD10-negative cells, and no CCND1 break apart was present in the CD10-positive cells. The positive (split signal) BCL2 result was present in both the BCL2-negative follicular lymphoma and the brightly BCL2-positive germinal center cells in the histologically uninvolved spleen. IGL@ break-apart probes also showed a split signal in both the follicular lymphoma nodules and the BCL2-positive germinal center cells in the uninvolved spleen and dual FISH using IGL@ and BCL2 probe was positive for IGL@/BCL2 fusion. PCR analysis was performed on laser capture microdissected tissue using BIOMED-2 IG primers. IGH@ PCR revealed identical monoclonal peaks using V-FR2 primers, as well as with the DH1-6 primers in two regions: tissues dissected from the mantle zones within the nodules of follicular lymphoma and in the mantle zones of the uninvolved white pulp; these peaks were not detected in three other regions: the BCL2-negative follicular lymphoma; the normal, BCL2-negative germinal centers in the uninvolved white pulp; or in the histologically normal but BCL2-positive germinal centers in the white pulp. IGK@ PCR (VK-Kde) revealed the same monoclonal rearrangement in all 5 regions. Proposed diagnosis Composite lymphoma, follicular lymphoma (grade 1-2/3) and mantle cell lymphoma, with "in situ" components. Interesting feature(s) of the submitted case This case demonstrates two coexisting "in situ" lymphomas within an uncommon composite lymphoma (follicular lymphoma and mantle cell lymphoma). The follicular lymphoma within the nodules is BCL2-negative while the follicular lymphoma "in situ" is BCL2positive and both harbor a t(18;22)(q21;q11).