By
Dr Fadhl Ali Almohtady
Consultant Surgeon
UST-Hospital
30--31 /5/2o12
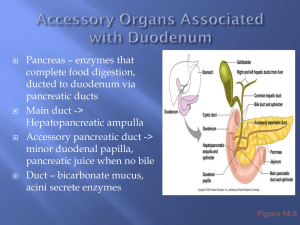
INTRODUCTION
Open cholecystectomy was the standard practıce
for treartment of symptomatıc gallbladder
dısease untıl later 1980
At present more than 90% of cholecystectomıes
are performed by laparoscopy whıch become one
of the commonest surgıcal procedure ın the world.
Unfortunately the wıdespread used of laparoscopy
has lead to a concurrence rıse ın the ıncıdence of
major bıle duct ınjury(BDI)
Complications of Laparoscopic Cholecystectomy :
A National Survey of 4,292 Hospitals and an Analysis of 77,604 Cases
Deziel D J et al Chicago Illinois - Am J of Surg 165 January 1993
1.750 respondents
1.2% laparotomy for treatment of complications
0.6% mean rate of bile duct injury (exclusive of cystic
duct), that will be lowered after performing > 100 LC
50% of bile duct injury was recognized postoperatively,
required anastomotic repair
33 pts died, 18 of them due to operative injury
0.14% bowel injuries
0.25% vascular injuries
Most lethal complications
Bılıary ınjury durıng
cholecystectomy
OC
:has been associated wıth 0.2%-0.4% risk of
BDI.
ON THE OTHER HAND (LC): has been associated with
2.5 fold to 4 folds increase in the incidence of post
operative BDI.
in 1990 high rate of BDI ıs due to in part to learnıng
curve effect .
A surgeon had ı.7% chance of BDI ın the first case a
0.17% chance of BDI after the 50th case.
However,most surgeon passed through the learning
curve (steady state)
BILE DUCT INJURY (I)
Any injury to the bile duct during
cholecystectomy is a dreaded complication.
Major bile duct injuries may require biliary-
enteric reconstruction
Many patients, their consultants, and their
lawyers believe these treatments result in a
lifetime of disability
(Maraca R.J et al : Arch Surge 2003, 137:889-894)
BILE DUCT INJURY (2)
The occurrence of an accidental bile duct injury
strikes the patient and surgeons with great force,
as neither is prepared for this complication
Often the surgeons is not immediately aware of
disaster, and a delayed diagnosis adds further
difficulty to the potentially disturbed relationship
between doctor and patient.
(Gouma DJ and Obertrop H : BJS 2002,89,385-386)
The Problem
LC has been associated with a higher incidence of
IA bile duct injuries
LC—0.4 to 0.8%
Traditional OC—0.2-0.4%
Association:
Increased mortality and morbidity
Reduced long-term survival
Reduced quality of life
Between 34% and 49% of surgeons are expected to
cause such an injury during their career.
Awareness and preventative methods are of
clinical importance to surgeons.
Risk Factors and Mechanism
Risk Factors
◦
Surgeon related rısk factors
◦
Lack of experıence
Mısıdentıfıcatıon of bılıary anatomy
Intraoperatıve bleedıng
Over confıdant surgeon
Improper ıterpretatıon of ıoc
Improper lateral retractıon
◦
◦
◦
◦
◦
◦
(insufficient or excess
Lack of conversıon ınto OC ın
dıffıcult cases
Risk Factors…….cont
Patıent related rısk factors:
◦ Age & sex
◦
◦
◦
◦
◦
Anatomical variations (biliary and
vasculature)
Severıty of dısease : Acute ,chronıc
cholecystıtıs,empyema and mırızzı
syndrome,…..
prevıous surgery wıth adhesıons.
Obesıty
Common Variant's of bile
duct anatomy
Lacey Clinic, Burlington, MA.1994
MANNER OF CONFLUENCE RIGHT
SECTORAL DUCTS
Blumgart LH. Surg Clin N Am. 1994.74.4
Risk Factors…….cont
Rısk factors ınherent to laparoscopıc
approach;
2-dimensional video monitor view,
fixed view point, etc
.loss of depth perceptıon
Lack of manual palpatıon
Surgeon dependant to equıpment
Blınd manıpulatıon the ınstruments
Mechanism of injury
Initially…Surgeon’s Learning Curve –Steady
Anatomical Misidentification: excision, incision, or
transection of biliary anatomy
◦
◦
Injuries: common bile duct, common hepatic
duct, right and left hepatic ducts, right hepatic
artery, ducts draining hepatic segments
Anatomical variations (biliary and vasculature)
Electro cautery, thermal injury: stricture of CBD or
hepatic ducts, bile leak
Mechanical trauma: stricture of the biliary ducts,
bile leaks
Improper surgical approach
Misidentification injuries 2 main
types ;
1-CBD is mistaken for cystic duct so is
clipped and divided.
2-The segment of an aberrant right
hepatic duct at the junction of cystic
duct and CHD is mistaken for cystic
duct
Classic Laparoscopic Injury
--Mistaking the common bile duct for the cystic duct
Thermal Injuries
Inappropriate
use of electro
cautery near
biliary ducts
May lead to
stricture and/or
bile leaks
Mechanical
trauma can have
similar effects
Lahey Clinic, Burlington, MA.1994
CHD DRAINS FREELY IN TO THE PERITONEAL
CAVITY
Lacey Clinic, Burlington, MA 1994
CLASSIFICATION OF BDI
There are many classıfıcatıon
systems,
Bismuth ,McMahon, Strasberg,
Amesterdam academic medical
center;s classificatıon, Stewart and
so and so……..
CLASSIFICATION OF BDI…..cont
PURPOSE to know the severıty of
the ınjury.
Communıcatıon purposes between
doctors and centers
Treatment purposes –modalıty of
treatment
Bismuth's classification (1982)[
Type
Criteria
1 Low CHD stricture, with a length of the common
hepatic
duct stump of >2 cm
2 Proximal CHD stricture-hepatic duct stump <2 cm
3 Hilar stricture, no residual CHD, but the hepatic
ductal
confluence is preserved
4 Hilar stricture, with involvement of confluence and
loss of communication between right and left hepatic
duct
5 Involvement of aberrant right sectorial hepatic duct
alone or with concomitant stricture of the CHD.
Bile
Duct
Injuries
Bismuth classification of bile duct
strictures
Lacey Clinic, Burlington, MA.1994
McMAHON classıfıcatıon
TYPE OF INJURY
1-MAJOR BDI
2-MINOR BDI
CRITERIA
1-Laceratıon > 25% of bıle
duct dıameter.
2-Trasectıon of CHDor
CBD.
3-Development of postoperatıve stıcture.
1-Laceratıon of<25% of
BD dıameter.
2-Laceratıon of cystıcCBD junctıon(buttonhole
tear)
Strasberg Classification
Type A Cystic duct leaks or
leaks from small ducts in
the liver bed
Type B Occlusion of a part
of the biliary tree, almost
invariably the
aberrant right hepatic
ducts
Type C Transection
without ligation of the
aberrant right hepatic
ducts
Type D Lateral injuries
to major bile ducts
Type E Subdivided as
per Bismuth
classification into E1 to
E5
Strasberg Classification, cont’d
E:
injury to main duct
(Bismuth)
E1: Transection >2cm from
confluence
E2: Transection <2cm from
confluence
E3: Transection in hilum
E4: Separation of major ducts
in hilum
E5: Type C plus injury in
hilum
AMESTERDAM ACADEMIC
MEDICAL CENTER
4 TYPES OF BDI CAN BE IDENTIFIED (MCMOHAN)
TYPE A:cystıc duct leak or leakage from a
berrant or perıpheral hepatıc radıcles.
TYPE B:major bıle duct ınjury wıth or wıthout
concomıtant bılıary strıcture.
TYPE C:bıle duct stıcture wıthout bılıary
leakage.
TYPE D:complete transectıon of BD wıth or
wıthout excısıon a part of the duct.
. Stewart-way classification
]
Class Criteria
of BDI
(2004)
Ⅰ CBD mistaken for cystic duct, but recognized
Cholangiogram incision in cystic duct extend
Ⅱ Bleeding, poor visibility Multiple clips placed on
CBD/CHD
CBD mistaken for cystic duct, not recognized
CBD, CHD, or right or left hepatic ducts transected and/or
resected
Ⅳ Right hepatic duct (or right sectorial duct) mistaken for
cystic duct
Right hepatic artery mistaken for cystic artery
Right hepatic duct (or right sectorial duct) and right
hepatic artery transected
Ⅲ
Way LW et al: An Surge, vole 237 No.4. 460-465, 2003
BUT NON OF THESE
CLASSIFICATION SYSTEM IS
UNIVERSALLY ACCEPTED AS EACH
HAS ITS OWN LIMITATION
About 25% of BDI discovered ıntraoperatıvely.
About 25% of BDI dıscovered after
24-48 hs post-operatıvely.
And about 50% of BDI present
weeks ,months or years post
operatıvely
CLINICAL PRESENTATION
Many injuries are unrecognizedd at
the time of the initial operation, and
their presentation will vary
Those with associated bile leak will
present early and often acutely ill
from bile peritonitis or sub-hepatic
abscess
CLINICAL
PRESENTAION….CONT
Those with an injury but not leak, usually
develop jaundice sometime after discharge
from hospital, depending of the nature of
the injury
Some injuries evolve slowly or cause partial
obstruction
Stricture may involve principally the right or
left hepatic duct or one of the right sectorial
hepatic ducts
BILE LEAK IS RECOGNIZED EARLIER
Presentation:
Acutely ill
Gut failure
Warko karnadihardja- 2004
Intraoperative Detection
Only 25% of injures are recognized
intraoperatively
If experienced, convert to Open Procedure and
perform Cholangiography (determine extent of
injury)
If not experienced, perform the cholangiogram
laparoscopically with intent of referring patient
(placement of drains)
Consult an experienced hepatobiliary surgeon.
Quicker the repair, the better the outcome!!!
Post-Operative Detection Plan
Controlling sepsis, establish biliary
drainage,
Broad-spectrum antibiotics.
No need for urgent reconstruction of the
biliary tree.
Reconstruction of the biliary tract is best
performed electively after an interval of at
least 6 to 8 weeks.
TIPS & TRICKS TO DIAGNOSE
BILE DUCT INJURY
History of unexplained fevers, pain,
abnormal liver function test results, or
pruritus
Should prompt an investigation
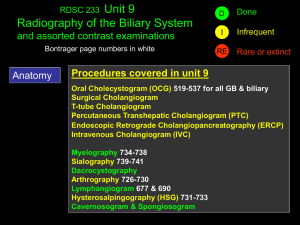
TYPES OF IMAGING INVESTIGATION
Ultrasonography
:
May reveal the :
ductal dilatation and or fluid
collection(biloma
Of little value if bile ducts are
decompressed
TYPES OF IMAGING INVESTIGATION (2)
Cholangiography
PTC is superior to ERCP
MRCP : Noninvasive, provides striking
images of biliary tree
HIDA scan ; may show presence of
active bile leak and general anatomic
site of leakage.
MRC ;
Demonstrating dilatation or stenosis of
the biliary tract; and stones in the bile
duct remnant; the pancreas; and
pancreatic duct;
However it doesn’t allow concomitant
therapeutic measures.
ERCP; PTC
Can provide an exact anatomical
diagnosis of bile duct leak.
Allowing for treatment of the leak by
appropriate decompression of the
biliary tract
TYPES OF IMAGING INVESTIGATION
Contrast-enhanced CT
The best initial study
May define level of injury, fluid collection or
ascites
Reveal lobar atrophy
For vascular ınjury; CT –angıography, MR angıography
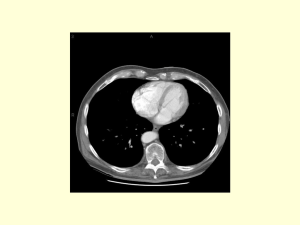
RIGHT LOBE ATROPHY AND COMPENSATORY LEFT LOBE
HYPERTROPHY
Can BDIs be prevented?
Conclusions
Bile duct injury during cholecystectomy,
either laparoscopic or open, is a complex
and a dreaded complication
The proximal bile duct is at greater risk for
injury in laparoscopic surgery and may
require biliary-enteric reconstruction
Early recognition, good surgical technique;
adequate multidisciplinary approach in a
tertiary care center are the cornerstones for
good outtcome.
Thank you