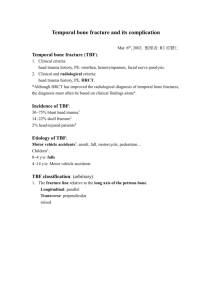
Pediatric Temporal Bone Fractures: Evaluation and
advertisement
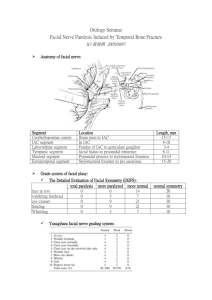
Pediatric Temporal Bone Fractures: Evaluation and Management Dennis J Kitsko, DO, FACS, FAOCO Assistant Professor of Otolaryngology Children’s Hospital of Pittsburgh University of Pittsburgh School of Medicine Clinical Findings - Overview Bleeding from ear canal Tympanic membrane perforation Hemotympanum Hearing loss – Conductive (43%) – Sensorineural (52%) CSF leak (28%) Facial paralysis (6%) Vestibular symptoms McGuirt 1992 Imaging CT temporal bones is the preferred study – Contrast not necessary – Coronal sections if possible – Classified as longitudinal and transverse – Indications: • Fracture on initial head CT • CSF otorrhea, CSF rhinorrhea, facial paralysis, hearing loss, severe vertigo MRA/MRV, CTA/CTV – May be indicated if suspicion of injury to dural sinus, jugular bulb, or ICA Longitudinal Fracture Parallel to long axis of t bone More common (70-90%) Lateral blow EAC fracture TM rupture Ossicular disruption Around otic capsule Foramen lacerum Facial nerve injury uncommon (often delayed sec. to edema) Longitudinal Fracture Injury to the roof of the middle ear (tegmen tympani) CSF otorrhea Transverse Fracture Perpendicular to long axis of t-bone Less common (10-30%) Frontoocciptal blow Otic capsule/vestibule/lateral IAC Sensorineural hearing loss and vertigo Facial paralysis TM often intact CSF rhinorrhea Longitudinal Fracture Transverse Fracture External Auditory Canal Injury Identify source of bleeding Assess extent of TM injury Clean cerumen and blood clots Check TMJ If significant displacement, may need ear packing CSF Leak 20-25% of pediatric temporal bone fractures (McGuirt 1992) Skull fracture + meningeal tear Permanent pathway for bacterial contamination and meningitis CSF Leak If TM rupture, will have otorrhea If TM intact, will appear as serous effusion – Lean the patient forward – if CSF, may drain down eustachian tube and out the nose (CSF rhinorrhea) Collect fluid – Beta-2-transferrin – protein found in CSF, perilymph • High sensitivity and specificity • Contamination with blood does not affect interpretation CSF Leak Initial management – Bed rest, head of bed elevation, avoid straining – Usually will stop spontaneously in 4-5 days – Prophylactic abx controversial Lumbar drain if persists >4-5 days Surgery when: – Leak persists >1-2 wks – Large bony defect – Brain herniation – Recurrent meningitis Hearing Loss Sensorineural Hearing Loss MUST get audiogram on all tbone fractures More common (50%) May be due to direct cochlear trauma (transverse fx) May also be concussive Treat expectantly (serial audiograms) Conductive Hearing Loss 20-65% of T-bone fractures Hemotympanum – Intact TM – Resolves spontaneously – Follow up 4-6 wks TM rupture – May heal spontaneously Ossicular disruption – Surgical intervention – Wait at least 6 wks Ossicular Disruption Incudostapedial joint separation (#1) Incudomalleolar dislocation Stapes crural fracture Vertigo Vertigo Labyrinthine concussion Fracture through the labyrinth (transverse fx) Perilymphatic fistula Shearing of 8th nerve (IAC) Vertigo Treat expectantly – CNS compensates and usually resolves within 6 wks – Exception – if strongly suspect perilymph fistula, consider exploration and round/oval window graft If persistent: – Consider electronystagmography – Rarely, surgical vestibular neurectomy or labyrinthectomy Facial Paralysis 50% of transverse fractures – Nerve transection 5-25% of longitudinal fractures – Often delayed secondary to edema and may spontaneously resolve Usually occurs in horizontal portion, between geniculate ganglion and second genu Facial Paralysis – Physical Exam Evaluate upper and lower face – Lower 2/3 only, consider CNS injury Difficulties: – Lacerations, ecchymosis, swelling, LOC If unconscious, attempt to elicit grimace and assess facial tone Facial Paralysis If immediate and complete: – CT T-bone • Localize site of injury – Audiogram • Helps determine surgical approach – Electrical testing • Inaccurate for 48-72 hrs Facial Paralysis Delayed onset: – Usually secondary to edema rather than direct injury – Spontaneous recovery may occur Facial Paralysis - Testing Nerve Excitability Test and Maximum Stimulability Test – Subjective – Can be performed after 48-72 hrs ENoG – evoked EMG – Objective – Can be performed after 6 days – >90% degeneration suggests poor outcome and may be used to determine if surgical intervention is necessary Facial Paralysis - Surgery 3 approaches: – Transmastoid – perigeniculate to stylomastoid foramen – Translabyrinthine – no cochlear function, allows exposure to labyrinthine segment and lateral IAC – Middle fossa – intact cochlear function, labyrinthine segment and IAC Decompress the nerve sheath If lacerated: – Direct reanastomosis if tension free – Greater auricular n graft • No return of function for at least 6 months • Incomplete return of function Summary Clinical examination: – Bleeding from ear canal – Tympanic membrane perforation – Hemotympanum – CSF leak – Vestibular signs and symptoms – Facial paralysis Studies: – Temporal bone CT scan – Audiogram Questions?