RHQN Best Practice VTE 4.10.12
advertisement

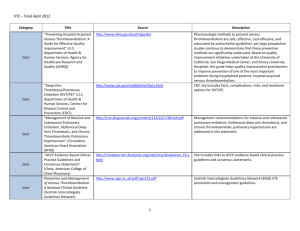
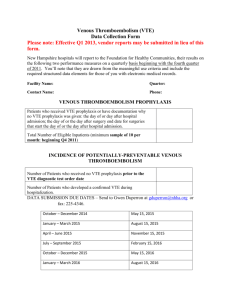
RHQN Best Practice Call: Partnership for Patients (PfP) focus: VTE Tuesday, April 10, 2012 Partnership for Patients includes 10 focus areas: (With Current RHQN Strategies for helping CAHs) 1. 2. PfP: Cultural Transformation Leadership Engagement CEO and Trustee Summit May 2nd or 3rd. Current activities: Hospital Survey of Patient Safety Culture (HSOPS)Second group of 7 CAHs now taking the Survey. Just Culture, Executive WalkRounds and TeamSTEPPS Communication tool training (currently Flex funded) RHQN Root Cause Analysis and Taste of Lean classes 3. PfP: Preventable Readmissions within 30 days Goal: Reduce preventable readmission from 2010 benchmark by 20% to end of 2013. See RHQN Best Practice calls with Whitman in the past on RHQN website. Also focus of future Best Practice calls. 4. PfP: Reduce Hospital Acquired Infections (HAI) and Hospital Acquired Conditions (HAC) by 40% from 2010 to end of 2013. 3. PfP: Infection Prevention Measures (HAI) Safe Table on April 11th. Encourage all to come to the Safe Tables. Sometimes works best for two to come because you have support when you go home and want to implement something 1) CAUTI- On Survey, 20 CAHs indicated they have a CAUTI Bundle. 3 asked for support. February Best Practice Call Fran Petersen, Lourdes : Nurse Initiated Foley Catheter removal-on RHQN Website. 2) Surgical Site Infections- RHQN will follow WSHA lead with CAH Best Practice discussions 3) VAP-Not applicable in many facilities. Others indicated on the RHQN Survey that they had Ventilator Bundle and QI monitoring. 4) CLABSI- 15 CAHs indicated on the Survey that you have CLABSI Bundles. 4 CAHs indicated it is not applicable. 4 asked for support. PfP: Hospital Acquired Conditions (HAC) 1) VTE- On Survey, 15 indicated they had a VTE Prevention and Treatment Protocol. Only 7 CAHs had QI projects to monitor and improve VTE rates. 5 did not and 7 asked for support. 2) Obstetrical Adverse Events-Working with CAHs who have challenges implementing the ACOG Guidelines for 39 weeks. Best Practice Sharing on-going. 3) Pressure Ulcers-April 25th-WSHA Web-conference and RHQN to follow 4) Falls-10 CAHs report on QBS. 6=less than 5%. See 4/25 WSHA Webconference. 5) Adverse Drug Events….27 CAHs indicated they track Adverse Events with 22 having a QI project in this area. We will work especially with the 7 who did not indicate they have a program in place. Also, we will bring Best Practices to you in the future. RHQN Best Practice Call: Partnership for Patients (PfP) focus: VTE April 10, 2012 Facilitated by Bev McCullough, RN, MBA, CPHQ VTE: DVT& PE: Alphabet Soup Venous Thromboembolism (VTE): Deep Vein Thrombosis of the lower leg (DVT) Clot dislodges from DVT, travels to the lungs and becomes a Pulmonary Embolism (PE) Implementing a VTE Protocol The “QI Basics”: “8 Steps for Effective Change” Explain the Urgency Leadership buy-in, Physician Champion, engaged team Have a shared vision Communicate to others: The “elevator speech” Remove barriers: empower to create change Choose well: Implement in one area, do “small tests of change” and then Celebrate Keep improving: PDSAs, Measure, Monitor, SPREAD Sustain VTE: The Urgency “Pulmonary Embolism is the third most common cause of hospitalrelated death and it is the most common preventable cause of hospital-related death.”* *http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/cardiology/venous-thromboembolism/ VTE: CMS Measures SCIP-VTE-1 Surgery Patients with Recommended Venous Thromboembolism Prophylaxis ordered SCIP-VTE-2 Surgery Patients Who Received Appropriate Venous Thromboembolism Prophylaxis Within 24 Hours Prior to Surgery to 24 Hours After Surgery VTE: Making the Case Meaningful Use: 2012 –Eligible CAHs seeking to demonstrate Meaningful Use are required to electronically submit aggregate CQM numerator, denominator, and exclusion data to CMS or the States. VTE: Making the Case Meaningful Use for Hospitals: VTE prophylaxis w/in 24 hrs. of arrival Intensive Care Unit VTE prophylaxis Anticoagulation overlap therapy Platelet monitoring on unfractionated heparin VTE discharge instructions Incidence of potentially preventable VTE VTE: Making the Case: TJC measures: CMS 2013 VTE-1* Venous Thromboembolism Prophylaxis VTE-2 Intensive Care Unit Venous Thromboembolism Prophylaxis VTE-3* Venous Thromboembolism Patients with Anticoagulation Overlap Therapy VTE-4 Venous Thromboembolism Patients Receiving Unfractionated Heparin with Dosages/Platelet Count Monitoring by Protocol VTE-5 Venous Thromboembolism Discharge Instructions VTE-6* Incidence of Potentially-Preventable Venous Thromboembolism VTE: Making the Case: The CAH National Measures Brief VTE prophylaxis VTE patients with anti-coagulation overlap therapy Incidence of potentially preventable VTE VTE Implementation The “QI Basics”: “8 Steps for Effective Change” Explain the Urgency Leadership buy-in, Physician Champion, engaged team Have a shared vision Communicate to others: The “elevator speech” Remove barriers: empower to create change Choose well: Implement in one area, do “small tests of change” and then Celebrate Keep improving: PDSAs, Measure, Monitor, SPREAD Sustain Choose a VTE Protocol Standardized processes The key to reliability All patients, Every time Example: 1. Wells Risk Assessment Tool 2. D-Dimmer blood test 3. Menu of appropriate prophylaxis options 4. Screening for pharmacological contraindications Scoring: Which Risk Tool do you use? Wells? Cabrini? Other: Wells with D-Dimer test ? Wells Score 1-Active Cancer 1=Paralysis, paresis, or recent plaster immobilization of lower extremities 1=Recently bedridden > 3 days or major surgery within 4 weeks 1=Localized tenderness along the deep venous system 1=Entire leg swollen 1=Calf swelling > 3 cm vs asymptomatic leg* 1=Pitting edema greater in symptomatic leg 1=Collateral superficial veins (not varicose) -2=Alternative dx as likely or greater than deep-vein thrombosis Wells Scoring High >=3 Moderate 1 or 2 Low 0 Modify by adding one point if there is a previously documented DVT Likely=>2 Unlikely=<1 Wells Scoring High >=3 Moderate 1 or 2 Low 0 Modify by adding one point if there is a previously documented DVT Likely=>2 Unlikely=<1 D-Dimer Test A blood test of a fibrin degradation product, present in the blood after a blood clot is degraded by fibrinolyis. Combined with the Wells clinical decision rule it has @ 99% predictive value for VTE. Choose a VTE Protocol Standardized processes Are the key to reliability All patients, Every time Example: 1. Wells Risk Assessment Tool 2. D-Dimmer blood test 3. Menu of appropriate prophylaxis options 4. Screening for pharmacological contraindications Menu of Treatment Options Pharmacological prophylaxis reduces the incidence of asymptomatic and symptomatic DVT and PE by 50-65%* Resources: Society of Hospital Medicine http://www.hospitalmedicine.org/ResourceRoomRedesign/RR_VTE /VTE_Home.cfm http://www.hospitalmedicine.org/ResourceRoomRedesign/R R_VTE/PDFs/SAMPLEVTEPROTOCOLS.pdf VTE Order Sets AHRQ Suggests the Society of Hospital Medicine site for CAHs Getting to 100% Situational Awareness and "Measure-intervention"— Identify patients on no anticoagulation-Put on the daily checklist. Empower nurses to place mechanical prophylaxis. Contact MD if no anticoagulant in place and no obvious contraindication: Template note, text page, etc. Back up these interventions: Physicians can not "shoot the messenger." Create Highly Reliable Strategies Desired Action is the Default (You have to Opt-Out if you don’t do it) Desired Action is Prompted by a reminder or decision aide Desired Action is Standardized into a process (a deviation feels weird) Desired Action is Scheduled to occur at known intervals Responsibility for the Desired Action is Redundant (Example: The clerk or pharmacist is empowered to halt processing of an admission order set that has not prophylaxis selected) Implementing a VTE Protocol The “QI Basics”: “8 Steps for Effective Change” Explain the Urgency Leadership buy-in, Physician Champion, engaged team Have a shared vision Communicate to others: The “elevator speech” Remove barriers: empower to create change Choose well: Implement in one area, do “small tests of change” and then Celebrate Keep improving: PDSAs, Measure, Monitor, SPREAD Sustain RHQN Website: http://www.rhqn.org/ Select “Resources”: User Name: RHQN Password: Quality1 Or contact: Bev McCullough, RN, MBA,CPHQ bevm@wsha.org 206-216-2862