SOD (NXPowerLite)
advertisement

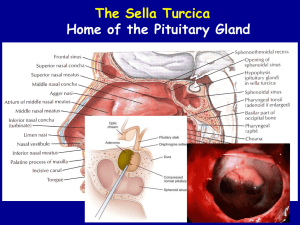
Septo-Optic Dysplasia Tim Alves Outline • • • • • • • Overview Etiology Epidemiology Presentation Workup Radiologic findings Prognosis and Treatment • Key Points • References Septo-optic dysplasia • Previously called De Morsier syndrome • Originally described in 1941 as an absence of the septum pellucidum with optic nerve abnormalities. • Later updated to include pituitary dysfunction • There is some controversy regarding diagnostic criteria, but generally it is a clinical diagnosis made when at least 2 of 3 classic criteria are met: » Optic nerve hypoplasia » Pituitary hormone abnormalities » Midline brain defects, including agenesis of the septum pellucidum and/or corpus callosum Etiology • Early forebrain developmental abnormality • Disorder of midline ventral prosencephalic development (~4th to 6th week of gestation) including optic nerves, forebrain, olfactory bulbs, septum pellucidum, corpus callosum, and pituitary gland • Most cases sporadic/idiopathic Etiology, cont. • Genetic basis? » AD and AR patterns have been described, two genes identified – HESX1 and SOX2 » Genetic diagnosis made in <1% of cases • Environmental? » Associated with maternal diabetes, quinidine ingestion, antiseizure medications, drug abuse, CMV infection, and congenital brain malformations • Multifactorial Epidemiology • 1 in 10,000 to 1 in 50,000 • More common in children born to younger mothers and firstborns • M=F, no ethnic predilection Uncertain classification • Heterogeneous, variable features and severity • Syndrome vs. complex • Continuum… » Milder form of lobar holoprosencephaly? » Milder forms of SOD? Presentation • Generally two presentations: » At birth, in association with multiple congenital anomalies – seizures, apnea, cyanosis, hypotonia, jaundice, microphallus » Later on in childhood, with growth failure and/or visual abnormalities • Approx. 50% do not have a schizencephaly – this group tends to present with endocrine dysfunction • Approx. 50% of patients with SOD have a schizencephaly and present with seizures, almost normal visual apparatus, generally normal endocrine function – “SOD plus” Associated Clinical Findings • Developme • ntal delay • • Seizures • • Visual • impairment • Sleep disturbance s • Precocious puberty Obesity Anosmia SNHL Cardiac anomalies Diagnostic Workup • History – visual problems, symptoms of hormonal deficiencies, other congenital and developmental abnormalities • Opthalmologic exam – optic nerve hypoplasia • Tests of pituitary function • MR is the best imaging modality MRI Findings in SOD • Optic nerve hypoplasia/dysplasia, unilateral or bilateral • Agenesis of the septum pellucidum • Abnormalities of the corpus callosum and hypothalamopituitary axis » Thin pituitary stalk, small anterior pituitary, posterior pituitary ectopia • Findings are variable, and also include… » Olfactory nerve hypoplasia, schizencephaly, cortical dysplasias and heterotopia. MR shows absent septum pellucidum, typical flat ventricular roof, pointy frontal horns, absent pituitary stalk and ectopic posterior lobe. Images show absent septum pellucidum, hypoplastic pituitary stalk and calloso-forniceal continuation. Significantly hypoplastic right optic nerve, ipsilateral to close lip schizencephaly is probably not SOD. The optic nerves are very small as is the optic chiasm and pituitary stalk, the septum pellucidum is absent. Imaging Differential Diagnosis • Lobar holoprosencephaly – similar to SOD but has lack of separation (“fusion”) of cerebral hemispheres, SOD is considered by some to be a milder form of this disorder • Overlap syndromes – Optic-infundibular dysplasia (OID) normal septum; Schizencephaly • Isolated ectopic posterior pituitary lobe –normal optic chiasm/nerves, normal septum • Kallmann Syndrome- absent or dysplastic olfactory nerves/ olfactory sulci, hypogonadotropic hypogonadism, occasionally associated with visual, septal, or pituitary abnormalities Prognosis and Treatment • Variable morbidity and prognosis - depends on associated brain and pituitary malformations • Possible hypothalamic and pituitary crises – sudden death from hypocortisolism • Treatment: Hormone replacement therapy Key points • Classically optic nerve hypoplasia, pituitary hormone abnormalities, and absent septum pellucidum • Disorder of early prosencephalic development with varying presentations and degrees of severity • Mainly a clinical diagnosis » Exact criteria and classification is debatable » Continuum? • Majority of cases are idiopathic/sporadic, but genetic and environmental causes have been identified • MRI of the brain plays a key role in diagnosis » Key findings » Quickly narrows down a broad clinical differential diagnosis References Adam, A. Grainger & Allison’s Diagnostic Radiology, 5th ed. 2008. Ch 70, Malformations of commissural and related structures + Figure 70.11 Barkovich AJ. Diagnostic Imaging: Pediatric Neuroradiology, 1st edition, 2007. Amirsys. I5: 10-13. Castillo M. Neuroradiology Companion: Methods, Guidelines, and Imaging Fundamentals, 3rd ed. 2006. p212-213. Hahn JS and Barnes PD. Neuroimaging advances in holoprosencephaly: Refining the spectrum of the midline malformation. Am J Med Genet C Semin Med Genet. 2010 Feb 15;154C(1):120-32. Webb EA, Dattani MT. Septo-optic dysplasia. European Journal of Human Genetics. 2010; 18:393-397.