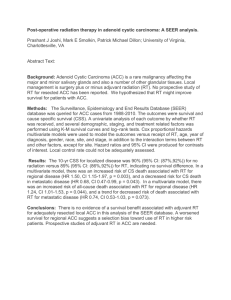
Adenoid Cystic Carcinoma: A clinical and molecular review
advertisement

Adenoid Cystic Carcinoma: A clinical and molecular review Patrick Ha, MD FACS Associate Professor, Johns Hopkins Department of Otolaryngology Johns Hopkins Head and Neck Surgery GBMC Head and Neck Grand Rounds, November 1, 2013 Disclosures • Research Funding: – NIH/NIDCR – Champions Oncology – Adenoid Cystic Carcinoma Research Foundation Adenoid cystic carcinoma Of all tumors in the region of the head and neck, the adenoid cystic carcinoma is one of the most biologically deceptive and frustrating in management. The subtlety of its presence, masquerading often as a benign tumor for years, the unexpected pernicious extensions, the high incidence of local recurrence and systemic spread, and the temporary favorable response to irradiation usually lead on the pathway to death. - John Conley Adenoid Cystic Carcinoma • Second most common salivary gland malignancy • Age: 40-50 • Women > men 3:2 • No associations with known exposures or diseases • 50% present with pain • Minor salivary glands > submandibular > parotid Numbers • Disease free survival: 60%, 50% 45% • Cause specific survival: 80%, 65%, 50%, 40% • 25-50% metastatic rate • Time to metastasis: 36 months (1mo – 19yrs) • Survival after metastasis: 40%, 15%, 10% (isolated pulmonary metastasis > bony mets) Spiro RH, Am J Surg 1997;174(5):495-8 Pathology • Cribriform (swiss cheese) • Tubular • Solid Perineural Invasion Surgical approach • • • • • • Wide local excision Neck dissection (?) Clear margins Balance with functional outcome Nerve preservation when possible Metastatectomy Surgical approach • “the biggest operation that can be rationally developed is the best” (Conley 1974) • Casler and Conley (1992) espoused radical parotidectomy for T2-3 lesions • No difference in survival with radical surgery • Obtain clear margins when feasible, balance with functional outcome • Elective lymph node sampling low yield Metastatectomy • Locati et al (2005) performed 26 procedures • If clear margins, then improved freedom from progression • No benefit to survival shown • Liu et al (1999) – pulmonary resection did not cure patients • Still performed in some centers Peter Tork Radiotherapy • No prospective randomized controlled study • Doses >60Gy more effective • Not effective as primary treatment (may have palliative role) • Appears to be good for local control in adjuvant setting • ?effect on survival • Retrospective bias Garden AS et al, Int J Radiation Oncol Biol Phys 1995 Garden AS et al, Int J Radiation Oncol Biol Phys 1995 Neutron Beam Therapy • Reduced cell damage repair, less variation during cell cycle, less oxygen requirements • 1988 – RTOG study found neutron beam better at local control and trend towards survival1 • Douglas et al2 – 159 patients with unresectable or gross+ margins. 5 yr survival 77%. 1Laramore 2Douglas GE et al. Int J Radiat Oncol Biol Phys. 1993;27(2):235-40 JG et al, Int J Radiat Oncol Biol Phys. 2000;46(3):551-57 Laramore et al. Int. J. Radiat. Biol. Phys. 27: 235-240, 1993 Their conclusion • “Further improvements in local-regional control are not likely to impact survival until more effective systemic agents are developed to prevent and/or treat distant metastatic disease.” 2Douglas JG et al, Int J Radiat Oncol Biol Phys. 2000 Neutron therapy and ACC Huber PE et al. Radiotherapy and Oncol 2001;59(2);161-67 Neutron therapy and ACC Huber PE et al. Radiotherapy and Oncol 2001;59(2);161-67 • Neutron beam less used recently • Follow up studies not as favorable • Toxicity level much higher • Investigators looking at carbon ions (Phase II) • ACCEPT - Cetuximab, IMRT with C12 heavy ion boost) for recurrent disease. • COSMIC – IMRT with C12 boost Adam Yauch (MCA) Role for Chemotherapy in ACC • • • • ACC needs systemic control Many limited trials performed Difficult to quantify response Limited numbers of patients – can one use the same agents across histologies? • Chemotherapy versus targeted therapy Important Guidelines in ACC Trial Evaluation • Evaluate rationale for use of known drugs in ACC: molecular basis for therapy • Enrollment criteria – recurrent vs progressive vs metastatic • Adherence to RECIST criteria reporting Single Agent Chemotherapy Trials Papaspyrou et al, Head Neck, 2011:33:905-11 Molecular targets in ACC • cKIT – growth, differentiation and migration. Expressed highly in 100% of ACC. No mutations found. May not be phosphorylated (activated) in ACC • EGFR – proliferation, motility, adhesion, invasion, angiogenesis, survival. 0-85% expression in ACC • Her-2 – 0-100% in ACC. Liu J et al, Head Neck, 2011 More molecular targets… • VEGFR – angiogenesis. Independent prognostic factor in salivary gland carcinoma. Cell line studies performed* • NFkB – suppresses apoptosis, regulated VEGF - ubiquitin-proteasome degradation pathway. The c-kit story • Identified as a tyrosine kinase receptor in 1987 • Proto-oncogene, found in testicular tumors, AML, GI stromal tumors, ACC • Found in a high percentage of ACC (Jeng et al, 2000, Freier et al 2005) • Loss of function: deafness, pigment defects C-Kit Pathway Imatinib • Blocks abl, c-kit, PDGF-R • Imatinib used in 2 patients with unresectable disease with + response (Alcedo et al 2004) • Formal multicenter trial – 16 patients with unresectable disease (Hotte et al, 2005) • No objective measures of response • 9/16 patients with stable disease • 6 patients with progressive disease • Separate trial with 10 patients also closed (Pfeffer et al, 2006) A decade of trials www.accrf.org Lapatinib • ErbB2 and EGFR inhibitor • Recurrent, progressive, or metastatic disease tested for 1+ EGFR and/or 2+ ErbB2 • 29/33 patients met criteria, 19 assessable patients treated • No objective response, 15 with stable disease (9 with stable disease >6 months), 4 with progressive disease. Agulnik M et al, JCO 2007 25(25):3978-84) ECOG 1303: Bortezomib + doxorubicin • Bortezomib – inhibitor of NFkB and 26S proteasome • If progressed, added doxorubicin • 24 patients received tx, no objective response with bortezomib – stable dz in 15/21. 10 had both D+B, 1 partial response, 6 stable disease • Well tolerated, but no response noted Argiris A et al, Cancer 2011, Aug 1; 117(15):3374-82 Sunitinib • Target VEGF, c-kit, RET, FLT3 • Progressive, recurrent and/or metastatic ACC • 13 assessable patients – no objective response. 11 with stable disease (8>6 months), 2 patients had progression. Chau NG et al. Ann Oncol 2011 Cetuximab and Cis-platinum • Locally advanced* (n=9) or metastatic (n=12) with positive EGFR expression • Loaded with Cetuximab, followed by weekly infusion • Locally advanced tumors received radiation and cisplatin • Metastatic received cis-platin and 5-FU * Refused surgery or unresectable Hitre E, et al. BJC 109, 2013 • Local advanced disease (n=9): – PFS = 64 months – 2-yr OS =100% – 2 CR, 2 PR, 5 SD • Metastatic (n=14): – PFS = 13 months – 2-yr OS = 24 months – 5 cases of PR Hitre E, et al. BJC 109, 2013 Current Trials • Eribulin Mesylate in recurrent or metastatic salivary gland cancer – Phase II. Microtubule inhibitor. Most studies in breast cancer • RTOG 1008: radiation therapy +/- cisplatin in advanced salivary gland cancers • Dovitinib Ways to improve trials • Consider symptom improvement • Include survival statistics • Include progressive or symptomatic patients only and describe criteria • Consider previous therapies and number/site of recurrence • Report ACC results separate from other salivary tumors Laurie SA et al, Lancet Oncology, 2011:12;815-24 John McCain Myb-NFIB fusion gene • NFIB – human nuclear transcription factor (9p23-24) • MYB – oncogene – cell proliferation, apoptosis, differentiation. (6q22-23) Persson et al, PNAS, 2009: 106(44): 18740-44 Implications of Myb-NFIB Fusion Gene • Myb-NFIB fusion present in 28-49% of ACC • Very specific for ACC, not other SGTs • Majority of ACC showed Myb overexpression, but higher levels if fusion present • Fusion may be variable • Unclear prognostic significance – high Myb expression and/or fusion gene may suggest worse outcome West RB et al, Am J Surg Pathol, 2011:35(1):92-9 Mitani Y et al. Clin Cancer Res, 2010;16(19):4722-31 MYB • No drug specifically targeting MYB yet • Possible downstream targets: – Cell cycle control (CCNB1, CDC2, MAD1L1) – Apoptosis (API5, BCL2, BIRC3, SHPA8, SET) – Cell growth/angiogenesis (MYC, KIT, VEGFA, FGF2, CD53) Exome Sequencing • Low mutational rate • Confirmed Myb translocations • Implicated FGFR pathway (3/24 and 30%), chromatin regulation • Underwhelming overall Ho AS et al. Nature Genetics, 2013 Stephens PJ et al, JCI, 2013 Dovitinib • FGFR1 is over-expressed (1a) and phosphorylated (1b) in the preponderance of ACC tumors. • FGF2, a molecule that binds to FGFR1, is a known downstream target of MYB • Screened in several xenograft mouse models of ACC and demonstrated activity Dovitinib Trial • Recurrent or metastatic disease • Phase II – endpoint = survival • Orally dosed – 500 mg, 5 days on, 2 days off for 4 weeks. • Treatment continues • 10 accrued in Uva, open enrollment for 33 in Korea Other Possibilities? • Personalized medicine approaches – Identification of specific known tumor markers – Xenograft model creation • In vivo testing for predictive tumor behavior • Identification of novel personal markers • Molecular profiling for identification of newer drug-able targets Moskaluk CA et al, Lab Invest, 2011:91(10);1480-90 Conclusions • Difficult tumor to treat when recurrent or metastatic, which is common • Surgery + radiation are standard • Numerous clinical trials, but limited conclusions drawn • Supports enrollment in clinical trials • Hope for molecular discovery leading to newer rational targets Irwin Jacobs ACCRF