High Grade Gliomas: Case Presentation and Discussion of
advertisement

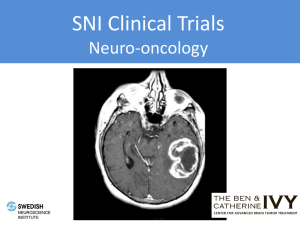
Jonathan Klein PGY3, Radiation Oncology University of Toronto Case #1 Mr. A 64M presents to ER with two weeks of dizziness and “things on my left side look funny”. Feels he veers to the left side when walking. Workup History Physical Workup History Characterize symptoms: OPQRST General: headache, seizures, N/V, syncope, cognitive Δ Focal: weakness, sensory loss, aphasia, visual Δ Family history PMHx/Meds/allergies Physical Workup History Characterize symptoms - OPQRST General: headache, seizures, N/V, syncope, cognitive Δ Focal: weakness, sensory loss, aphasia, visual Δ Family history PMHx/Meds/allergies Physical CNS: GCS, CNII-XII, gait, strength, DTRs, Babinski Screening CVS, lung, abdomen exam Imaging MRI with gadolinium is preferred modality Relevant imaging findings for contouring T1 with gadolinium: enhancing cavity T2/FLAIR: edema and enhancement Workup Imaging Histology 4 criteria (AMEN) : nuclear Atypia Mitosis Endothelial proliferation Necrosis # Criteria Grade 0 I 1* II *1 criterion = atypia for Grade II 2 III 3-4 IV Staging AJCC TNM Staging System not used Staging GBM can be primary or secondary (10%) Prognosis Prognosis by classification Oligodendroglial component is positive prognostic factor Prognosis Curran, JNCI, 1993 Recursive partitioning analysis to retrospectively analyze 1578 patients with high grade glioma 3 RTOG studies testing RT +/- Chemo Results <50yo: histology most important prognostic factor >50yo: KPS most important prognostic factor Mental status differentitated poor KPS group Conclusion: Older and poor KPS do worse Curran et al. J Natl Cancer Inst. 1993 May 5;85(9):704-10. Lamont ED, Christakis NA. Survival estimates in advanced cancer. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA, 2013. Prognosis By recursive partitioning analysis (RPA) Curran et al. J Natl Cancer Inst. 1993 May 5;85(9):704-10. Management Referred to Neurosurgery What should they do? Surgery NO RCTs have studied Surgery vs not Total vs subtotal resection Standard: Attempt at gross resection Not always possible Location Critical structures Surgery Simpson, Int J Radiat Oncol Biol Phys, 1993 Review of 3 RTOG trials: 643 patients with GBM Improved survival with more resection Surgery: % of patients: MS (months): Biopsy Partial Total 17% 64% 6.6 10.4 Simpson JR et al. Int J Radiat Oncol Biol Phys. 1993 May 20;26(2):239-44. 19% 11.3 Surgery Lacroix, J Neurosurg, 2001 Retrospective review, 416 patients with GBM Improved survival with total resection (>98%) Surgery MS (months) Partial (<98%) 8.8 Total (>98%) 13 Predictors of survival Age, KPS, extent of resection, degree of necrosis, pre-op MRI enhancement Lacroix M, et al. J Neurosurg. 2001 Aug;95(2):190-8. Back to Case Patient taken to OR Resection attempted, but 2.4cm segment of tumour remains Management Referred to Radiation Oncology What should we do? Radiation Walker, J Neurosurg, 1978 Phase III, 303 patients with anaplastic glioma Surgery then randomized to: MS (mo) RT vs BCNU vs 8.1 4.2 RT+BCNU vs Obs 8 3.2 Showed no benefit from chemo RT = 50Gy WBRT + 10 Gy boost BCNU = carmustine 80mg/m2 x days 1-3 every 6-8 weeks Walker MD et al. J Neurosurg. 1978 Sep;49(3):333-43. Radiation Walker, Int J Radiat Oncol Biol Phys, 1979 Meta-analysis of 3 RCTs 621 patients with Gr. III/IV glioma Surgery then: MS (mo) Obs vs 45Gy vs 50Gy vs 55Gy vs 60Gy 4 3 7 9 10 Showed benefit for RT and dose-response relationship Walker MD, et al.Int J Radiat Oncol Biol Phys. 1979 Oct;5(10):1725-31. Radiation Walker, NEJM, 1980 Phase III, 358 patients with anaplastic glioma Surgery then randomized to RT vs RT+BCNU vs RT+Semus vs Semus Results No arm significant difference between arms Conclusion: RT alone remains standard Walker MD et al. N Engl J Med. 1980 Dec 4;303(23):1323-9. Radiation Kristiansen, Cancer, 1981 Phase III, 118 patients with Gr III/IV astrocytoma Surgery then randomized to: MS (mo) RT vs RT+Bleomycin vs Obs 10.8 10.8 5.2 Showed no benefit from chemo RT = 45Gy WBRT Bleomycin = carmustine 180mg 3/week, 1hr prior to RT, weeks 1,2,4,5 Kristiansen K et al. Cancer. 1981 Feb 15;47(4):649-52. Radiation Laperriere, Radiother apy + Oncology, 2002 Systematic review of 6 RCTs Confirmed benefit from post-op RT Recommended: Young (< 70 yo) Treat enhancing tumour + margin (e.g. 2 cm) Dose: 50-60 Gy in 1.8-2Gy per fraction Older with good KPS Can use short course RT Older with poor KPS Can consider supportive care alone This review did not recommend addition of chemo Laperierre N et al. Radiother Oncol. 2002 Sep;64(3):259-73. Radiation So RT is good… What dose should we give? Radiation Nelson, NCI Monog., 1988 RTOG 74-01 626 patients with Gr III/IV astrocytoma Randomized to: 60Gy* vs 60+10 vs 60+B** vs 60+C+D*** Median survival: 60Gy: 9.3 months vs 60+10Gy: 8.2 months Subsets: >60 yo: RT+chemo did not improve survival 40-60 yo: RT+BCNU = 23% 2 year survival vs RT alone = 8% *60 Gy WBRT **60 Gy + carmustine (=BCNU) ***60 Gy + semustine + dacarbazine Nelson DF et al. NCI Monogr. 1988;(6):279-84. Radiation Bleehen, BJC, 1991 474 patients with Gr III/IV astrocytoma Surgery, no chemo, then randomized to: MS (mo) 45/20* vs 40/20+20/10** 9 12 60/30 improved survival with similar toxicity *=45/20 to “all known and potential tumour” **=40/20 as above, then 20/10 to “defined tumour volume together with a 1 cm margin around it.” Bleehen NM, Stenning SP. Br J Cancer. 1991 Oct;64(4):769-74. Radiation Scott, Int J Radiat Oncol Biol Phys, 1998 RTOG 9006 712 patients with Gr III/IV glioma Randomized to carmustine + : MS (mo) 60/30 vs 72/60 (1.2 Gy/# BID) 13.2 11.2 72/60 not better for any subgroup 60/30 was better for all patients < 50 yo Scott CB et al. Int J Radiat Oncol Biol Phys. 1998 Jan 1;40(1):51-5. Radiation Should we use SRS? ?SRS? Early series showed promising survival w/SRS Buatti et al., 1995 Gannett et al., 1995 Int J Radiat Oncol Biol Phys. 1995 Apr 30;32(1):205-10. Int J Radiat Oncol Biol Phys. 1995 Jul 15;32(4):1161-6. Int J Radiat Oncol Biol Phys. 1995 Sep 30;33(2):461-8. Masciopinto et al., 1995 J Neurosurg. 1995 Apr;82(4):530-5. ?SRS? RTOG 9305 Souhami, Int J Radiat Oncol Biol Phys, 2004 RCT, 203 GBM pts all received 60Gy EBRT +carmustine Randomized to upfront SRS vs no SRS (15-24Gy) Median survival not different: 13.5 v 13.6 months SRS not currently standard for GBM Souhami et al. Int J Radiat Oncol Biol Phys 2004;60:853-860. Management Referred to Medical Oncology Should the patient have chemotherapy? Chemotherapy Stewart, Lancet, 2002 Metanalysis, 12 RCTs, 3004 patients Hazard ratio for death = 0.85 Chemotherapy group did better Stewart LA. Lancet. 2002 Mar 23;359(9311):1011-8. Review. Chemotherapy Stewart LA. Lancet. 2002 Mar 23;359(9311):1011-8. Review. Chemotherapy Stupp, JCO, 2002 Phase II, 64 patients with primary GBM RT + Temozolomide RT: 60Gy/30 TMZ: 75 mg/m2/d x 42d then 200 mg/m2/d for 5d q28d x6 cycles Median survival = 16 months OS: 1 yr = 58% ; 2 yr = 31% Grade ≥3 toxicity = 6% Good prognosis subsets: ≤50 years old patients who had debulking surgery Stupp R et al. Clin Oncol. 2002 Mar 1;20(5):1375-82. WAKE UP!!!! Important Study Alert EORTC 26981 Stupp, NEJM, 2005 (2009 Lancet Oncology update) Phase III, 573 patients <70 yo with primary GBM Randomized to RT alone vs Stupp Phase II protocol: RT: 60Gy/30 TMZ: 75 mg/m2/d x 42d then 200 mg/m2/d for 5d q28d x6 cycles Stupp R et al. N Engl J Med. 2005 Mar 10;352(10):987-96. EORTC 26981 88% of patients received full course ChemoRT 40% of patients completed adjuvant Chemo Grade ≥3 toxicity = 4% EORTC 26981 MS (med) PFS (med) OS: 2 yr 4 yr 5 yr RT ChemoRT 12.1 mo 5 mo 10% 3% 2% 14.6 mo 6.9 mo 26% 12% 10% EORTC 26981 Overall survival curve Stupp R et al. N Engl J Med. 2005 Mar 10;352(10):987-96. EORTC 26981 Subgroups: Methylated MGMT Unmethylated Stupp R et al. N Engl J Med. 2005 Mar 10;352(10):987-96. EORTC 26981 Improved response for patients with methylated MGMT gene Epigenetic silencing of MGMT (O6-methylguanineDNA methyltransferase) DNA-repair gene by promoter methylation compromises DNA repair and has been associated with longer survival in patients with glioblastoma who receive alkylating agents. Hegi ME et al. N Engl J Med. 2005 Mar 10;352(10):997-1003. MGMT Methylation Hegi, NEJM, 2005 206 patients from EORTC 26891 trial assessed for MGMT methylation status MethylMGMT found in 45% Results MethylMGMT was a favorable prognostic factor: HR =0.45 For methylMGMT TMZ better than RT: 21.7 vs 15.3 months For unmethylMGMT, no statistically significant difference Conclusions GBM with methylMGMT benefited from TMZ, but unmethylMGMT promoter did not benefit Hegi ME et al. N Engl J Med. 2005 Mar 10;352(10):997-1003. Hegi ME et al. N Engl J Med. 2005 Mar 10;352(10):997-1003. RTOG 0525 Gilbert, ASCO, 2011 RCT, 833 pts > 60 yo with GBM/Gliosarcoma Test dose-dense TMZ regimen Randomized to EORTC 26981 RT+TMZ protocol vs 60Gy/30 + daily TMZ followed by 21d adjuvant chemo Gilbert MR et al. Journal of Clinical Oncology, 2011 ASCO Annual Meeting Proceedings (Post-Meeting Edition). Vol 29, No 15_suppl (May 20 Supplement), 2011: 2006 RTOG 0525 Gilbert MR et al. Journal of Clinical Oncology, 2011 ASCO Annual Meeting Proceedings (Post-Meeting Edition). Vol 29, No 15_suppl (May 20 Supplement), 2011: 2006 RTOG 0525 Gilbert MR et al. Journal of Clinical Oncology, 2011 ASCO Annual Meeting Proceedings (Post-Meeting Edition). Vol 29, No 15_suppl (May 20 Supplement), 2011: 2006 RTOG 0525 Improved response for patients with methylated MGMT continued No difference in PFS or OS between study arms for either methylated or non-methylated subgroups Ongoing Studies What is being tested now? Biologic agents Ongoing Studies RTOG 0837 Phase III RT+TMZ vs RT+TMZ+bevacizumab Bevacizumab (Avastin) shown effect in RCC,NSCLC,CRC RTOG 0825 Phase III RT+TMZ vs RT+TMZ+cediranib Back to case Patient receives concurrent 60Gy/30 RT Planned for continuing adjuvant monthly TMZ Patient returns to clinic 1 month after treatment with MRI Scan shows increased enchancement of treated tumour cavity …Now what? …Did treatment fail? Pseudoprogression Sanghera, Can J Neurol Sci, 2010 Retrospective, 111 patients GBM or Gr.III with GBM-like radiographic features Used Stupp RT+TMZ protocol Pseudoprogression (psP) = no further radiographic progression, without salvage therapy, within 6 months after TMZ+RT Represent transient increase in vessel permeability and damaged peritumoural BBB Sanghera P. Can J Neirol Sci. 2010 Jan;37(1):36-42. Pseudoprogression Results psP group had stable dexamethasone dose 25% had evidence of early progression, with 32% of these representing psP Median OS : whole cohort = 56.7 weeks psP = 125 weeks true early progression = 36 weeks Conclusion: Maintenance TMZ should not be stopped on the basis of seemingly discouraging imaging features within first three months after RT/TMZ. Pseudoprogression Sanghera P. Can J Neirol Sci. 2010 Jan;37(1):36-42. Pseudoprogression Brandes, JCO, 2008 Cohort, 103 patients with MGMT status Treated with Stupp TMZ+RT protocol Results psP occurs in 91% of methylMGMT +ve GBM vs 41% -ve +ve methylMGMT and psP each improved survival Patients more sensitive to treatment more likely to get psP Brandes AA. J Clin Oncol. 2008 May 1;26(13):2192-7. Pseudoprogression Sanghera, Clin Oncol, 2012 Expert consensus on psP Poor efficacy 2nd line Tx so need to minimize inappropriate withdrawal of adjuvant TMZ psP unlikely if radiographic progression over 2 mo within 6 mo post-Tx Sanghera P. Clin Oncol (R Coll Radiol). 2012 Apr;24(3):216-27. Pseudoprogression Sanghera P. Clin Oncol (R Coll Radiol). 2012 Apr;24(3):216-27. Sanghera P. Clin Oncol (R Coll Radiol). 2012 Apr;24(3):216-27. Back to case Patient continues on monthly adjuvant TMZ Returns for 6 month post-RT appointment and has another MRI Scan shows clearly increased size of disease …Now what? Recurrent GBM - RT Median time to recurrence is ~7 months Re-irradiation trials Over 300 patients reported Combs 2005; Nieder 2008; Fogh 2010 Results 6 month PFS: 28-39% 1 year median OS: 26% (range 18-46%) Source: RTOG 0125 protocol. May be accessed at: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=1205 Recurrent GBM - RT Fogh, JCO, 2010 147 patients with recurrent GBM Treated with stereotactic RT 35/10 Cox analysis performed Survival improved with: Younger age Smaller GTV Shorter time between diagnosis and recurrence High RT dose (≥35Gy) showed trend to significance (p = .07). Survival not improved by: Surgical resection Chemotherapy Source: RTOG 0125 protocol. May be accessed at: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=1205 Fogh SE et al. J Clin Oncol. 2010 Jun 20;28(18):3048-53 Recurrent GBM - Chemo Phase II chemo trials Wong ET et al. J Clin Oncol. 1999 Aug;17(8):2572-8. Carson KA et al. J Clin Oncol. 2007 Jun 20;25(18):2601-6. 6 month PFS: 15%; Median OS: 6 months Bevacizumab/other monoclonal Abs studied in ph. II trials Vredenburgh JJ et al. J Clin Oncol. 2007 Oct 20;25(30):4722-9. 32 pts given bevacizumab + irinotecan 6 month PFS: 38%; MS for GBM patients: 9.2 months Kreisl TN et al. J Clin Oncol 2009 Feb 10;27(5):740-5. 48 recurrent glioblastoma patients received bevacizumab alone Response rate: 25%; Median PFS: 16 weeks; 6-month PFS:29 Other trials have added bevacizumab to other chemo agents such as low dose TMZ, etoposide, erlotinib, nitrosurea No improvement in survival shown, but worse toxicity Source: RTOG 0125 protocol. May be accessed at: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=1205 Recurrent GBM - Chemo Friedman HS et al. J Clin Oncol. 2009 Oct 1;27(28):4733-40. RCT, 167 patients with recurrent GBM in 1st or 2nd relapse Randomized to bevacizumab alone 10 mg/kg q2weeks vs bevacizumab +irinotecan (82 patients) Results not significant: 6-month PFS: Median survival: Beva alone 42.6%; 9.2 months Beva+irino 50.3% 9.7 months Conclusion: No increase in efficacy with irinotecan, but increase toxicity Source: RTOG 0125 protocol. May be accessed at: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=1205 Recurrent GBM - Chemo Salvage chemotherapy post-bevacizumab failure has 6- month PFS of 2% (Quant 2009). Recurrent GBM patients should be enrolled on trial whenever possible Ongoing trials include RTOG 1205: Randomized Phase II for recurrent GBM Bevacizumab + RT vs bevacizumab alone Source: RTOG 0125 protocol. May be accessed at: http://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=1205 Case #2 Mr. B. 80M 2 weeks persistent headache and malaise Refractory to OTC analgesia Diagnosed with GBM on imaging Referred to NeuroSx Taken to OR for biopsy Platelets decreasing so procedure abandoned Mr. Z. Referred to Rad Onc for management Work up History Physical Imaging Mr. Z. What to do? No biopsy, so no tissue diagnosis Treated as presumed GBM Management Curran, JNCI, 1993 Recursive partitioning analysis to retrospectively analyze 1578 patients with high grade glioma 3 RTOG studies testing RT +/- Chemo Results <50yo: histology most important prognostic factor >50yo: KPS most important prognostic factor Mental status differentitated poor KPS group Conclusion: Older and poor KPS do worse Curran et al. J Natl Cancer Inst. 1993 May 5;85(9):704-10. Management Bauman, Int J Radiat Oncol Biol Phys, 1994 Prospective, 29 patients with GBM Treated with 30Gy/10 WBRT Compared with historical radical and supportive care controls Results Overall median survival 6 months Median survival: RT = 10 mos; Supp. care = 1 mo Improved survival for radical dose if KPS>50 Conclusion: 30/10 reasonable for older patients with poor KPS Bauman GS et al. Int J Radiat Oncol Biol Phys. 1994 Jul 1;29(4):835-9. Management Roa W, J Clin Oncol, 2004 RCT, 100 patients with GBM ≥ 60 yo Randomized to radical RT 60/30 vs short course RT 40/15 No chemo during Tx (some got for recurrence) Results Median survival: Radical= 5.1 mos; Short= 5.6 mos 6 months survival: Radical= 44.7%; Short= 41.7% Short course reduced steroid requirements Conclusion: Short course reasonable to older patients Roa W et al. J Clin Oncol. 2004 May 1;22(9):1583-8. Management Roa W et al. J Clin Oncol. 2004 May 1;22(9):1583-8. Management Keime-Guibert, NEJM, 2007 RCT, 81 patients with Gr. III/IV astrocytoma All got surgery Age ≥ 70 yo and KPS ≥ 70 Randomized to RT 50 Gy vs supportive care alone Results Trial stopped early due to superiority Median survival: RT= 29.1 wks; No RT= 16.9 wks Survival benefit independent of extent of surgery No effect on HRQoL or cognition from RT Conclusion: RT is good for older, good KPS patients Keime-Guibert et al. N Engl J Med. 2007 Apr 12;356(15):1527-35. Management OS Management Muni, Tumori, 2010 Prospective comparison study 45 patients with GBM Age ≥ 70 yo OR Age 50-70 and KPS < 70 1:1 split of 30Gy/6 ± TMZ 150-200 mg/m2 x5d q28d Median OS 6 mo OS Median PFS 6 mo PFS RT+TMZ 9.4 mos 95% 5.5 mos 45% No TMZ 7.3 mos 78% 4.4 mos 22% Minimal additional toxicity (≥Gr 3 = 46%) Conclusion: RT+TMZ beneficial for older or poor KPS patients Muni R et al. Tumori. 2010 Jan-Feb;96(1):60-4. NOA-08 Wick, Lancet Oncol, 2012 RCT, 412 patients with Gr III/IV astrocytoma Age ≥ 65 yo AND KPS ≥70 Powered for non-inferiority Randomized to: RT 60Gy/30 vs TMZ 100mg/m2 x7d 1wk-on/1wk-off Wick W et al. Lancet Oncol. 2012 Jul;13(7):707-15 NOA-08 Results Median survival: RT=9.6 mo; TMZ=8.6 mo P(non-inferiority)=0.033 Event-free survival: RT=4.7mo; TMZ=3.3mo P(non-inferiority)=0.043 Subgroups MGMT methylation cohort had improved survival Median survival: Methylated=11.9mo; Unmethylated=8.2mo Patients with MGMT methylation did better with TMZ EFS for +ve methMGMT: RT=4.6 months; TMZ=8·4 months; RT=4·6 [4·2-5·0]), Patients without MGMT methylation did better with RT EFS for –ve methMGMT: RT=4.6 months; TMZ=3.3 months Conclusion: TMZ alone is not inferior to RT for elderly, good KPS patients. MGMT methylation status can aid decisions. Wick W et al. Lancet Oncol. 2012 Jul;13(7):707-15 RT +/- TMZ Malmstrom, Lancet Oncol, 2012 RCT, 291 patients with GBM ≥60 yo Randomization stratified by centre TMZ 200 mg/m2 x5d q28d for 6 cycles vs hypo# RT: 34 Gy/3-4 Gy per fraction vs standard RT: 60Gy/30 Malmstrom A et al. Lancet Oncol. 2012 Sep;13(9):916-26. RT +/- TMZ Results Overall TMZ better than standard 60Gy RT median OS: TMZ=8.3 months; 60Gy RT=6.0 month Standard 60 Gy RT not better than hypo# 34Gy RT Median OS: 34Gy RT=7.5 mos; 60 Gy RT =6.0 mos p=0.24 TMZ not better than hypo# 34Gy RT Median OS: TMZO=8·4 mos; 34Gy RT= 7·4 mos p=0·12 RT +/- TMZ Subset results Patients > 70 years old TMZ better than standard RT HR 0.35 p<0.0001 Hypo# 34Gy RT better than standard RT HR 0.59 p=0.02 Patients receiving TMZ Methylated MGMT had better median overall survival vs nonmethylated MGMT MethylMGMT = 9·7 months; nonMethylMGMT= 6·8 months p=0·02 Patients receiving RT No difference between methylMGMT and unmethylMGMT HR=0·97 p=0·81) All patients 60-70 years older than 70 years Figure 2 Kaplan-Meier analysis of overall survival in patients randomised across three treatment groups (A) All patients. (B) Patients aged 60?70 years. (C) Patients older than 70 years. TMZ=temozolomide. 34 Gy=hypofractionated radiotherapy. 60 . Malmstrom A et al. Lancet Oncol. 2012 Sep;13(9):916-26. Back to Case Mr. B treated with 40Gy/15 RT alone No chemo