Infantil infected chronic subdural hematoma
advertisement

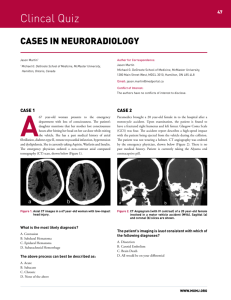
Infantil infected chronic subdural hematoma Case presentation Helene Hurth, MS6 Innsbruck Medical University M.M. • H&P: 5 m.o. male: fever, irritability for 3 days, intermittent emesis poor hygiene, macrocephaly no h/o trauma, no LOC alert, moves all extremities, PERRL, EOMI, bulging fontanelle, Temp: 40,6°C (105,1°F), BP 82/67mmHg, HR 180, RR 34, SpO2 99% no ecchymosis/lacerations/abrations/deformities/crepitus • Lab: CRP 40,3 mg/dl, WBC 14,8 • PMH:term born, methamphetamine pos at birth PICU at 1 month for RSV, apnea spells • SH: father retains full custody open CWS case – mother: substance abuse 3y/o healthy sibling M.M. Preoperative MRI Bilateral chronic subdural hematoma Le: 25 mm Ri: 15 mm Enhancement of membranes 3mm rightward midline shift M.M. • Subdural tab via AF after admission: 4+ GNR in gram stain – E.coli • Burr hole drainage w/ bilateral drains the next morning • Abx: Ceftriaxone, Meropenem Postoperative MRI Le: 12 mm Ri: 7-8 mm Resolution of midline shift Septations OP • Craniotomy w/ resection of membranes on day 5 after borr hole drainage due to remaining fever and up trending inflammatory markers Childhood extraaxial CNS infections • Age peaks: >11y (50%) & <1y (>20%) • Duration of symptoms based on underlying cause • Fever, headache, altered consciousness, focal deficits, full AF, poor feeding, seizures S. Gupta, J Neurosurg Pediatrics 2011 Childhood extraaxial CNS infections • Postsinusitis: (frontal) SDE, epidural abscess, Pott‘s puffy tumor; +- cerebritis • Postmeningitis: diffuse hemispheric/infratentorial SDE • Postoperative: epidural abscess, SDE, osteomyelitis at OP-site • Otogenic -> mastoiditis: SDE, epidural abscess S. Gupta, J Neurosurg Pediatrics 2011 Childhood extraaxial CNS infections • Treatment: Initial wide craniotomy + abx • Complications: recurrent seizures, venous sinus/ cortical vein thrombosis • Outcome: preoperative presentation Etiology early, aggressive surgical treatment S. Gupta, J Neurosurg Pediatrics 2011 Infected CSDH • Rare • Strept spp, Staph aureus, H. influenzae, E. coli, Salmonella spp • Hematogenous • Satisfactory outcome • Antibiotic treatment • Drainage vs craniotomy Surgical treatment: CSDH • Pre-OP T2*-MRI, randomly BH or SC • Burr holes: equivalent, lower mortality/morbidity/hospital stay • Small craniotomy w/ resection of outer and intrahematomal membranes: superior if intrahematomal membranes present N=20 N=29 M. Tanikawa, Acta Neurochirurgica 2001 Surgical treatment: CSDH • Outcome, reoperation, hospital stay • Hematoma recurrance: thick membranes -> residualhematoma -> rebleeding MRI (T2*) imaging to predict need for craniotomy M. Tanikawa, Acta Neurochirurgica 2001 Case Tanikawa et al. Summary • Neurosurgery often required in extraaxial CNS infections • Early diagnosis! • Consider infected CSDH with signs of bacteremia