UNOS/OPTN PPT template 04/2012 - dark
advertisement
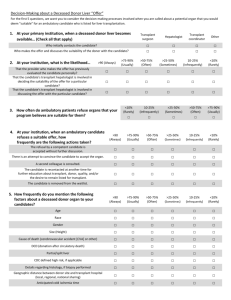
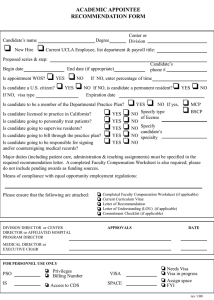
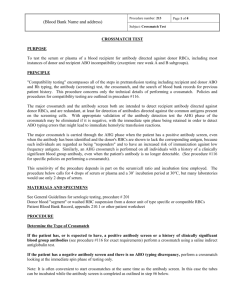
OPTN Kidney Paired Donation (KPD) Histocompatibility Testing Policies Kidney Transplantation Committee Spring 2014 Background Kidney Committee distributed KPD policies for public comment in March 2012 A number of commenters had concern with histo section due to missing requirements Professional societies brought together a KPD consensus conference around same time This proposal incorporates spring 2012 OPTN public comment feedback findings from KPD consensus conference recommendations from OPTN Histo Committee The Problem Low match success rate in KPD program Antibody related issues and positive crossmatches continue to account for a number of match failures Insufficient histocompatibility testing requirements to prevent match failure Goal of the Proposal Increase match success rate in KPD program by preventing unexpected positive crossmatches that can break chains and prevent candidates and donors from accessing subsequent match runs and transplant opportunities Promote transplant safety through more effective screening of kidney offers Proposed: HLA Typing Molecular HLA typing required for donors and candidates Loci required for donors: HLA-A, B, Bw4, Bw6, C, DR, DR51, DR52, DR53, DPB, DQA, DQB Loci required for candidates: HLA-A, B, Bw4, Bw6, DR If candidate has unacceptable antigens, additional loci required: C, DR51, DR52, DR53, DPB, DQA, DQB Candidate’s hospital must retype donor to confirm HLA type Proposed: Antibody Screenings Candidate’s transplant hospital must screen for antibodies at all of the following times: every 90 days when potentially sensitizing event occurs if candidate reactivated after more than 90 inactive days if unacceptable positive crossmatch occurs that prevents transplant with matched donor Labs must use method at least as sensitive as crossmatch method Physician/surgeon (or designee) and lab director (or designee) must review and confirm UA’s listed for candidate Proposed: Crossmatching Candidate’s transplant hospital must perform physical crossmatch before donor’s nephrectomy is scheduled Must report crossmatch results to donor’s transplant hospital and UNOS If unacceptable positive crossmatch occurs between candidate and matched donor, candidate’s hospital must inactivate candidate before next match run, review the unacceptable antigens (UA), and report reason to UNOS w/in 7 days Candidate can be reactivated once review and update (if applicable) of UAs is complete Supporting Evidence Crossmatch-related refusals (postive crossmatch or unacceptable antigens) account for ~30% of failed matches 61 programs had accepted at least one match offer for which the entire exchange fell through Some programs may have had a disproportionately high number of crossmatch-related refusals 39 programs refused at least one match offer due to a crossmatch-related reason Specific Feedback Request If unacceptable positive crossmatch occurs between candidate and matched donor, candidate’s hospital must inactivate candidate in the KPD program before next match run If this change is approved, is it less burdensome for transplant programs if the inactivation is automatic (completed by UNOS)? Specific Feedback Request Is it burdensome to require antibody screenings every 90 days for ALL candidates (even if not sensitized?) Should longer timeframe between screenings apply for non-sensitized candidates? 180 days? What Members will Need to Do Donor’s transplant hospital responsible for reporting donor HLA info, arranging shipment of donor blood sample to candidate’s hospital or histo lab Candidate’s transplant hospital responsible for reporting candidate HLA info, confirming donor HLA info, antibody screening requirements, crossmatching requirements Questions? Mark Aeder, MD KPD Work Group Chair mark.aeder@uhhospitals.org Name Region # representative Email Gena Boyle Committee Liaison gena.boyle@unos.org