lt23879-sup-0001-suppinfo
advertisement
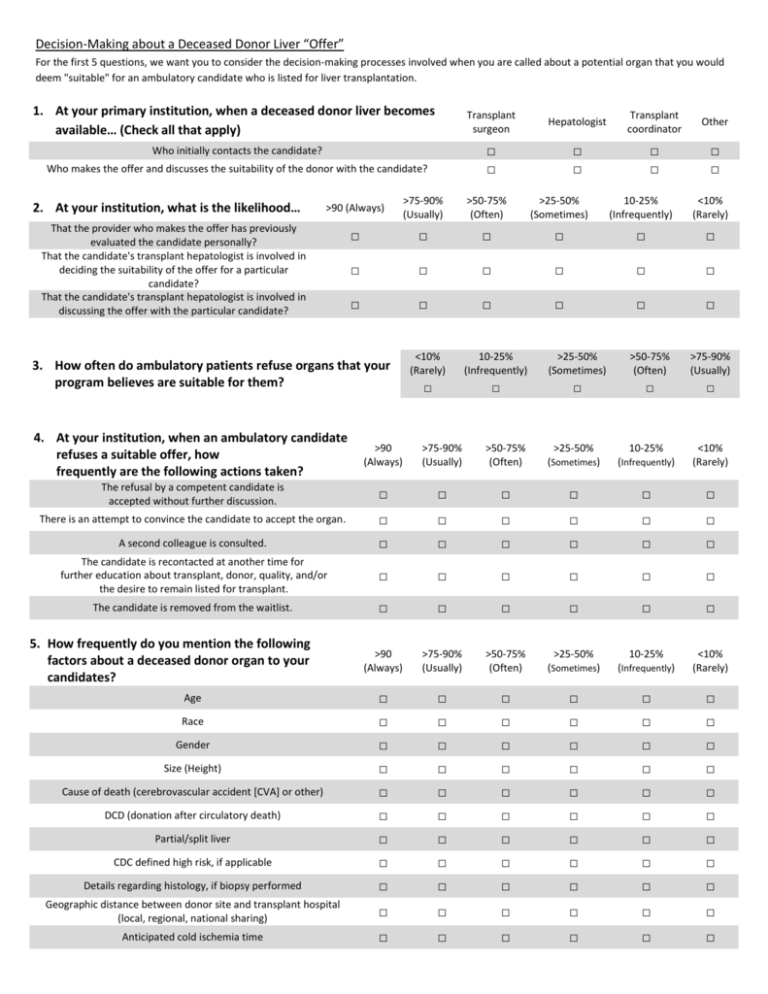
Decision-Making about a Deceased Donor Liver “Offer” For the first 5 questions, we want you to consider the decision-making processes involved when you are called about a potential organ that you would deem "suitable" for an ambulatory candidate who is listed for liver transplantation. 1. At your primary institution, when a deceased donor liver becomes available… (Check all that apply) Transplant surgeon Hepatologist Transplant coordinator Other Who initially contacts the candidate? □ □ □ □ □ □ □ □ Who makes the offer and discusses the suitability of the donor with the candidate? 2. At your institution, what is the likelihood… >90 (Always) >75-90% (Usually) >50-75% (Often) >25-50% (Sometimes) 10-25% (Infrequently) <10% (Rarely) □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ That the provider who makes the offer has previously evaluated the candidate personally? That the candidate's transplant hepatologist is involved in deciding the suitability of the offer for a particular candidate? That the candidate's transplant hepatologist is involved in discussing the offer with the particular candidate? 3. How often do ambulatory patients refuse organs that your program believes are suitable for them? <10% (Rarely) 10-25% (Infrequently) >25-50% (Sometimes) >50-75% (Often) >75-90% (Usually) □ □ □ □ □ 4. At your institution, when an ambulatory candidate refuses a suitable offer, how frequently are the following actions taken? >90 (Always) >75-90% (Usually) >50-75% (Often) >25-50% (Sometimes) 10-25% (Infrequently) <10% (Rarely) The refusal by a competent candidate is accepted without further discussion. □ □ □ □ □ □ There is an attempt to convince the candidate to accept the organ. □ □ □ □ □ □ A second colleague is consulted. □ □ □ □ □ □ The candidate is recontacted at another time for further education about transplant, donor, quality, and/or the desire to remain listed for transplant. □ □ □ □ □ □ The candidate is removed from the waitlist. □ □ □ □ □ □ >90 (Always) >75-90% (Usually) >50-75% (Often) >25-50% (Sometimes) 10-25% (Infrequently) <10% (Rarely) Age □ □ □ □ □ □ Race □ □ □ □ □ □ Gender □ □ □ □ □ □ Size (Height) □ □ □ □ □ □ Cause of death (cerebrovascular accident [CVA] or other) □ □ □ □ □ □ DCD (donation after circulatory death) □ □ □ □ □ □ Partial/split liver □ □ □ □ □ □ CDC defined high risk, if applicable □ □ □ □ □ □ Details regarding histology, if biopsy performed □ □ □ □ □ □ Geographic distance between donor site and transplant hospital (local, regional, national sharing) □ □ □ □ □ □ Anticipated cold ischemia time □ □ □ □ □ □ 5. How frequently do you mention the following factors about a deceased donor organ to your candidates? Liver Donor Risk Index The liver donor risk index (LDRI) model developed by Feng et al (2006) identifies seven donor factors associated with relative risk of allograft failure. These factors are: 1) Age; 2) Race; 3) Height; 4) Cause of death (Cerebrovascular Accident [CVA]); 5) Other cause of death 6) DCD (Donation after Circulatory Death); and 7) Partial/split liver. Feng et al’s model was modified and the final LDRI model also factors in regional and national sharing and cold ischemia time. 20% of transplants had an LDRI <=1 (1 year survival 87.6%) and 6% of transplant had an LDRI >=2 (1 year survival 71.4%). 6. How familiar are you with the LDRI? □ Very familiar 7. How do you use the LDRI? □ Moderately familiar □ Not familiar at all Yes Always Yes Usually Yes Sometimes Yes Rarely No □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ Do you or a member of your team currently discuss the concept of LDRI to your patients at the time of listing? Do you or a member of your team currently tell the patient the specific LDRI of the liver graft that is being offered? If LDRI were to become a part of a new liver allocation system, do you think a candidate should be told the specific LDRI of the liver graft that is being offered? Other (please specify): 8. In your opinion… Does LDRI adequately describe the relative risk of a given donor liver? Are there individual factors for each donor (and recipient) that make discussing a donor liver LDRI potentially misleading? Feel free to elaborate: 9. What impact, if any, will providing a specific LDRI number have on the following ethical considerations? □ Somewhat familiar Yes No □ □ □ □ Increase/Improve Decrease/Worsen No Change □ □ □ □ □ □ □ □ □ □ □ □ Patient autonomy Physician autonomy Shared decision-making Candidate refusal of an "offer" Demographics Professional Role □ Transplant surgeon □ Hepatologist Age _____________ How would you best describe your practice? □ Internist What is your gender? □ Academic Medical Center Clinical care How would you describe the percent of your time spent on each of the following responsibilities? Research Teaching Administration What is the approximate number of deceased donor liver transplants done at your center yearly? __________ □ Nonphysician transplant professional □ Female □ Male □ Private Practice 0-24% □ Other (please specify):______________________________ □ HMO □ □ □ □ □ Other (please specify):_____________________________ 25-49% 50-74% 75-100% □ □ □ □ □ □ □ □ □ □ □ □ What is the approximate number of living donor liver transplants done at your center yearly? What percentage of the liver transplants performed at your institution are outpatients (ambulatory) at the time of the offer? □ >90% Virtually all □ >75-90% □ >50-75% Most Frequently □ >25-50 Sometimes What is the average MELD score at time of transplantation for ambulatory patients of blood type O at your institution? □ <15 □ 15-20 □ 21-25 □ 26-30 __________ □ 10-25% □ <10% Infrequently Rarely □ 31-35 □ 36-40