Unique Anticoagulation Issues at University Hospitals Case Medical
advertisement

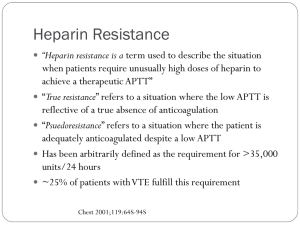
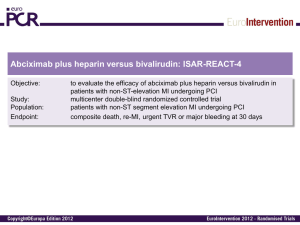
Unique Anticoagulation Issues at University Hospitals Case Medical Center Teresa L. Carman, MD Director, Vascular Medicine Case Medical Center Pager 33515 Discussion • • • • Use of the heparin protocol Anti-Xa assay vs. aPTT Safe discharge of patients Anticoagulation monitoring service referrals Heparin Order Set IV Heparin Protocol • Diagnosis / Weight Based Dosing Low intensity dosing • ACS, Stroke High intensity dosing • VTE, CVT, Afib • Nurse Driven Titration Titration table based on 4 hr anti-xa lab value obtained after initial dosing or titration changes With the change in monitoring the titration table will change to reflect a 6 hr interval for required titrations IV Heparin Protocol • Full Protocol Includes: Initial Loading Bolus Titrated Drip Additional (Repeat) Bolus IV Heparin Protocol Ordering Choose the “Loading Dose” to order the initial bolus IV Heparin Protocol Ordering Choose “Continuous Infusion” to order the drip • Includes standard nurse driven titration protocol IV Heparin Protocol Ordering Choose the “Repeat Bolus” for nursing to give a bolus based on Q 4 hr aPTT (anti-Xa) lab value X IV Heparin Protocol Why order the full protocol? Clinical Results: • Full protocol NOT ordered 39 hr average time to therapeutic • Full protocol ordered 11 hr average time to therapeutic • All patients were either therapeutic or supratherapeutic within 6 hrs IV Heparin Protocol Why the 4 hour dosing change to the protocol? • With a 6 hour protocol it usually takes 8 hours between dose adjustments • The 4 hour protocol should decrease this interval to approximately 6 hours • This should allow patients to a reach consistent therapeutic range sooner thus impact the risk for recurrent events aPTT VS. Heparin Assay Monitoring Overview of aPTT • The aPTT is used in most clinical laboratories to monitor coagulation and specifically monitor anticoagulants ie. intravenous unfractionated heparin and direct thrombin inhibitors • Clinicians have familiarity with assay • Readily automated • Current targets were established based on data from a post-hoc analysis of a 1972 study which suggested 1.52.5 times aPTT control reduced risk the of recurrent thromboembolism Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Disadvantages of Using aPTT to Monitor Heparin • aPTT has variable a response to heparin determined by the different coagulometers and the reagents There is no aPTT “standard” When the tissue thromboplastin lot changes, a new therapeutic range needs to be established for the new lot of reagent • Test may be affected by numerous factors other than heparin concentration Baseline elevated aPTT makes titration difficult and inaccurate Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Conditions that May Prolong the Baseline aPTT • Lupus anticoagulants • Other antiphospholipid antibodies • Prekallikrein, High Molecular Weight Kininogen Level • Low levels (<40%) of: Fibrinogen Prothrombin Factors V, VIII, IX, X, XI, and XII Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Current Recommendations from CHEST Guidelines • Each coagulation laboratory determines the therapeutic range for their aPTT reagent that correlates with a heparin assay level of 0.3 to 0.7 international units (IU)/mL (by anti-Factor Xa assay) • Each laboratory must determine its own therapeutic range for heparin for the aPTT whenever the aPTT reagent changes or with a change in instrumentation Therefore, the range changes almost annually Hirsh J. Chest 2008;133:141-59 Monitoring Update on Monitoring • As of summer 2011 the use of the “aPTT, heparin” is not available for monitoring IV unfractionated heparin therapy at University Hospitals Case Medical Center. (no correlations have been done) • The “aPTT, heparin” has been replaced by anti-Xa monitoring using the “heparin assay, UFH” • The use of the “heparin assay, UFH” will standardize IV unfractionated heparin monitoring and make the use of the aPTT inaccurate Heparin Assay • Specifically determines anticoagulant activity of IV unfractionated heparin by measuring ability of heparinbound antithrombin to inhibit a single enzyme • More specific than aPTT since it measures inhibition of a single enzyme • Major advantage is lack of biologic factors that affect its result Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Limitations of Heparin Assay • Clinical data examining outcomes is limited Eikelboom JW. Thromb Haemost 2006;96:547-52. Francis JL. Pharmacotherapy 2004;24:108S-19S. Comparison of Monitoring with aPTT vs. Anti-Factor Xa Assay • Prospective, single-center study 1.8 P<0.0001 1.6 • 268 patients on IV heparin for variety of indications 1.4 1.2 P<0.0001 1 • Utilizing anti-Factor Xa assay led to fewer tests and dose adjustments N= APTT 0.8 0.6 0.4 0.2 • Cost increase of $1.09/day more using anti-Factor Xa assay Anti-Factor Xa Assay 0 Monitoring Tests/24 hours Dosage Changes/24 Rosborough TK. Pharmacotherapy 1999;19:760-66. “High-Intensity Therapeutic Heparin” Anticoagulation Orders for Adult Patients Current “High-Intensity Therapeutic Heparin” Anticoagulation Orders Using Heparin Assay for Adult Patients (VTE etc) Current “Low-Intensity Therapeutic Heparin” Anticoagulation Orders Using Heparin Assay for Adult Patients (ACS, stroke) No Changes for the Monitoring of Other Anticoagulants • Prothrombin time/INR is still be used to monitor warfarin • Therapeutic monitoring of direct thrombin inhibitors (bivaliruding and argatroban) still use the aPTT • Special monitoring for enoxaparin (Lovenox®) is done by Heparin assay, Lovenox Summary Order Set Changes Heparin assay, UFH will be done after initiation and dose changes as well as each morning. Timing will be changed to a 4 hour response time for all dose adjustments. Summary • UH uses the heparin assay, UFH for monitoring all intravenous unfractionated heparin therapy. • The order set will change to reflect the therapeutic ranges for “High-dose” and “Low-dose” indications “high-dose” anti-Xa = 0.3-0.7 IU/ml “low-dose” anti-Xa = 0.3-0.6 IU/ml • The time between adjustments and monitoring will decrease to 4 hours in an effort to shorten the time to therapeutic Summary • No changes will occur related to warfarin monitoring Prothrombin time/INR is the standard • No changes will occur related to direct thrombin inhibitor monitoring, aPTT • Enoxaparin (Lovenox®) is monitored by the Heparin assay, Lovenox. Overview of the Trends In VTE Management • Prevention** - to decrease the incidence of VTE ALL PATIENTS REQUIRE PROPHYLAXIS** • Improved sensitivity/specificity and ease of diagnosis • Improve treatment – increased efficacy and reliability of pharmaceuticals • Improve outcomes - decrease risk of recurrence • Decrease longterm morbidity from VTE Post-thrombotic syndrome (PTS) Chronic thromboembolic disease (CTED) Anticoagulation Committee • Meaningful Use VTE quality measure – VTE prophylaxis within 24 hours of arrival – ICU VTE – Anticoagulation overlap therapy – Platelet monitoring for unfractionated heparin – Comprehensive discharge instructions – Incidence of potentially preventable VTE • Approach – Fit compliance into current clinician workflow • No additional resources • No retrospective chart abstraction Essentials 1. All patients require DVT prophylaxis screen on admission 2. The proper prophylaxis is ordered or an appropriate reason of ommission is documented Hospital acquired VTE is considered a “never event” 3. VTE treatment transition must meet current guidelines and this is documented and supported by the discharge orders VTE Quality Measure • To meet certain care standards to prevent and treat DVT/PE • Must complete the DVT Risk Assessment Screening on admission – Includes orders based on risk score for both pharmacologic and mechanical – Be sure to enter omission reason if choosing not to order prophylaxis Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Deep Vein Thrombosis Risk Screening Safe Discharge on Anticoagulation Anticoagulation Medication Reconciliation • New drop down box specific to anticoagulant drugs Show screen shot of the drop down • May enter up to 2 anticoagulants that the patient is being discharged on • Will include a question about whether the patient had a DVT or PE confirmed during this hospital admission. If yes, then you must enter in the date of the diagnostic test that gave the confirmation. Warfarin Anticoagulant effect (VII, IX) vs. Antithrombotic effect (X, II) Anticoagulant effect can be seen within 2 days Antithrombotic effect takes minimum of 4-5 days due to the t ½ of prothrombin (24-48 hours) Warfarin • Current ACCP guidelines recommend 5-10 mg initial dosing In the elderly, patients who are debilitated, malnourished, have CHF, liver disease or recent surgery or who are taking medications which increase sensitivity to warfarin - initial dose should be ≤ 5 mg • Hospitals patients should RARELY receive more than 5 mg initial coumadin dosing • Higher initial doses may be suitable for stable, healthy outpatients • Monitoring should begin after 2-3 doses • 5 mg vs. 10 mg initial dose debate Early INR changes are due to FVII depletion Minimum of 4-5 days are required to deplete FX and FII Chest 2008;133(3Suppl):454-545. Warfarin Follow Up Appointment All patients discharged on Warfarin: • Discharge instructions must include an appointment for Warfarin follow up monitoring. • Discharging provider enters this information in the follow up section on patient profile (CMC) which has a new option specific to Warfarin follow up. • Includes: The clinic or physician that will cover the follow up monitoring • (UH “Coumadin Clinics” are now called “Anticoagulation Monitoring Services” Phone number Date next PT/INR is due Anticoagulation Monitoring Service AKA – Coumadin Clinic Anticoagulation Monitoring Service Referral AMS Referral Anticoagulation Monitoring Service Referral Anticoagulation Monitoring Service Therefore – engage the PCP early and often Anticoagulation Management • Must document and “manage” all aspects of anticoagulation • Minimum of 5 days overlap required • INR max 3 days after starting therapy • Min every 2 days during the transition • Need 2 checks the week following Anticoagulation Monitoring Service • Monitor anticoagulation for a MANAGING PHYSICIAN Nurse driven protocol following the orders of the physician • We ARE NOT responsible for the patient until the first visit – usually 3-5 days after dc If the visit is delayed someone else needs to be monitoring If the visit is missed someone else is responsible • We do NOT dose adjust without orders • Expectations are that the orders are followed – any desirable adjustments may be made and will be followed Ie shorter or longer intervals for management • If warfarin or lovenox etc are required the managing physician must be engaged We will facilitate referrals for the physician with the pharmacy Warfarin Follow Up Appointment All patients discharged on Warfarin: • Discharge instructions must include an appointment for Warfarin follow up monitoring. • Discharging provider enters this information in the follow up section on patient profile (CMC) which has a new option specific to Warfarin follow up. • Includes: The clinic or physician that will cover the follow up monitoring • (UH “Coumadin Clinics” are now called “Anticoagulation Monitoring Services” Phone number Date next PT/INR is due Conclusions • On admission ALL patients require DVT risk assessment and prophylaxis orders • Heparin when required - use the order sets High dose vs. Low dose • Anti-Xa monitoring is the UHCMC standard for adult patients • Discharge on anticoagulation requires effort PCP contact for follow up AMS referral Interim plan for delays in presentation to the AMS ****LMWH or other anticoagulants may require preauthorization so request SW/pharmacy approvals early