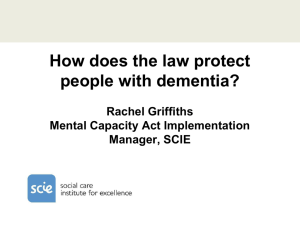
The Mental Capacity Act in practice
advertisement
Dementia: protection of human rights Oxford Brookes 11 June 2013 Rachel Griffiths Care Governance Lead, Oxfordshire County Council Consultant in human rights-based practice Magna Carta (1297) "No freeman shall be taken or imprisoned, or disseised of his freehold, or liberties, or free customs, or outlawed, or exiled, or any otherwise destroyed; nor will we not pass upon him, nor condemn him, but by lawful judgment of his peers, or by the law of the land." Legal frameworks for protection European Convention on Human Rights Mental Health Act 1983 Human Rights Act 1998 Mental Capacity Act 2005 Deprivation of Liberty Safeguards 2009 European Convention on Human Rights Product of the Council of Europe set up in 1949 in aftermath of WW2 Largely protects civil and political rights Human Rights Act 1998 enshrines the ECHR in UK Law so that it is unlawful for a public body to act in a way that is incompatible with ECHR rights Human Rights Act 1998: articles relevant to care Article 2 –Right to life Article 3 – Prohibition against torture and inhuman or degrading treatment Article 5 – Right to liberty and security of person Article 8 – Right to private and family life ‘very essence ... is respect for human dignity and human freedom’ Pretty v United Kingdom (2002) MCA: human rights for those aged 16+ who might lack capacity MCA Principles: Presumption of capacity (not incapacity) maximisation of capacity: empower people to make their own decisions Unwise decisions don’t necessarily mean lack of capacity Decisions must be in P’s best interests Look for the least restrictive option that meets the person’s need MCA s.1 What does ‘capacity’ mean? It is ‘decision specific and time specific’: Can the person make THIS decision at the time it needs to be made? Must be able to: understand, retain, use and weigh information relating to the decision, and then communicate it. Using the MCA to plan in advance Planning Ahead Advance Decision to Refuse Treatment Must have capacity to do this You can only REFUSE treatment, you can’t insist on a certain treatment being provided You CAN refuse in advance life-sustaining treatment but special rules apply You can always change your mind if you have the mental capacity to do so Lasting Powers of Attorney (LPA) Before the MCA, Enduring Powers of Attorney (EPA), covering financial matters MCA created 2 LPAs: one similar to EPA New LPA for health and welfare Can give trusted relatives/friends right to make health/welfare decisions, but they are then bound by MCA Code of Practice Do all you can to empower someone Right setting, right time of day, right mood Explain simply and make sure the person has any aids they need (including friendly support) Remember an “unwise decision” doesn’t of itself mean lack of capacity Human Rights Act Article 8 Everyone has the right to respect for his private and family life, his home and his correspondence. There shall be no interference by a public authority with the exercise of this right except such as is in accordance with the law and is necessary in a democratic society [...] for the protection of health or morals, or for the protection of the rights and freedoms of others. What freedoms does Article 8 protect? To text, phone, e-mail or write To choose own friends Access to fresh air and exercise Privacy in washing and toilet Privacy for visits Confidentiality of medical records Freedom from intrusion into private life Freedom from searches of living space and person Get to know the person (1) Jimmy is 78, and has dementia: he can be aggressive and irritable. Staff panic when he is found trying to take the back door off its hinges: they discuss how to restrain him His wife visits, and explains he used to be a carpenter, and had noticed the door was sticking. The home manager gives him access to some tools, and staff bring in small items of furniture for him to mend. How should we approach ‘risk’? What good is it making someone safer if it merely makes them miserable? We must tolerate acceptable risks as the price appropriately to be paid in order to achieve some other good – in particular to achieve the vital good of the elderly or vulnerable person’s happiness Lord Justice Munby, re MM Get to know the person (2) Mick has early onset dementia: he finds it hard to talk. His wife has died recently, and he has come to live in a small care home. Staff find him a ‘handful’. In particular it takes up to 4 people to restrain him to be shaved: staff justify this as in his best interests. A neighbour comes to visit, and says, ‘Why, Mick, I’ve never seen you without your beard before!’ Proportionality: a golden thread Any interference in the rights of someone lacking capacity to consent to your action must be a proportionate response to The likelihood of the person suffering harm if we don’t act, and The seriousness of that harm. Need to consider level of incapacity when thinking about autonomy Warning from CQC research A care home had a ‘no restraint’ policy therefore restraint was not acknowledged… Therefore it was not identified as such… Therefore not described clearly in care plans ... Therefore a less restrictive option not sought… Therefore there was no learning from incidents (which were not correctly recorded in case files)... ‘We never use restraint’ MCA defines restraint not only as the use (or threat) of force to make someone who lacks capacity do something they’re resisting, but any restriction on their movement whether they resist or not. Locked doors do restrict movement; they may well be lawful, if in a person’s best interests, but must be recognised as restraint and the effects minimised as much as possible. Deprivation of Liberty Safeguards (‘DoLS’) Protect the human rights of people (18+) who lack capacity to consent to staying in a hospital or care home, for treatment or care in their best interests These Safeguards do not authorise treatment They enable a person to challenge a very restrictive regime DOLS fit inside MCA which fits inside human rights law ‘Rules of the House’ Experienced as arbitrary, disempowering: You must go to bed at 9 to be safe; you can’t have a mobile phone because one person used it to order drugs; you can’t go out alone because one resident got lost; your family can’t bring in a home-made curry because someone once had an upset tummy How do general restrictions arise? Overarching imperative to keep people safe Fear of things going wrong Often a chaotic changing situation Physical/psychological restraint a default option for everyone, rather than last resort Balance between risk and autonomy loaded towards risk avoidance Staffing shortages and strains Misleading language Language of restraint is sometimes blurred: “we never restrain anybody” yet evidence of restraint in MCA terms (locked doors to, say, kitchen, outside space, wider world) Rooms used for isolation in care homes can be given innocuous names, e.g. The Blue Room, the Quiet Room…“duty of care” used to overrule autonomy “activities” or sensory room dull, unstimulating MCA as lever to improve practice Process for best interests decision-making in complex, individual, HUMAN contexts Steeped in regard for autonomy MCA-compliant care plans only restrict freedoms, on an individual basis, where necessary to prevent harm and proportionate to the likelihood and seriousness of that harm Sources of information and advice SCIE http://www.scie.org.uk/mca Rachel Griffiths: Consultant in MCA and human rights-based practice rachel.griffiths@talktalk.net