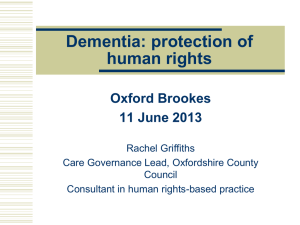
How does the law protect people with dementia?
advertisement

How does the law protect people with dementia? Rachel Griffiths Mental Capacity Act Implementation Manager, SCIE European Convention on Human Rights Mental Health Act 1983 Human Rights Act 1998 Mental Capacity Act 2005 Deprivation of Liberty Safeguards (2009) All this law is aimed at protecting the basic human rights of vulnerable people, who share with all of us the right to live our lives as we choose to do. These laws are intended to keep interference by others in our lives to a minimum If we might lack capacity for some decisions at some times, those others might need to make decisions for us, but they must act in a way that is proportionate Grand laws to protect small freedoms Where, after all, do human rights begin? In small places, close to home – so close and so small that they cannot be seen on any map of the world. Yet they are the world of the individual person… (Eleanor Roosevelt, 1958) A judge links human rights law with dignity: Munby LJ Human dignity is all the more important for people whose freedom of action and choice is curtailed, whether by law or by circumstances such as disability. The Convention is a living instrument...We need to be able to use it to promote respect for the inherent dignity of all human beings but especially those who are most vulnerable to having that dignity ignored. Why adopt human rights as the overarching umbrella? Five Principles of the Mental Capacity Act 2005 Presumption of capacity Do all you can to increase capacity Unwise or eccentric decisions don’t of themselves mean a person lacks capacity If a person lacks capacity to make a decision, the decision must be made in the person’s best interests Seek the least restrictive option to meet the need What is ‘mental capacity’ and how do we assess it? Capacity is the ability to make a decision at the time needs to be made. Two – Stage Test: Is there an impairment /disturbance in the functioning of mind or brain? And, if so, Does that prevent the decision being made? 4 Steps: understand, retain, use/weigh, and communicate. If a person lacks capacity to make a decision, follow the Best Interests track To make a Best Interests decision: If P is likely to regain capacity, can it wait? Avoid discrimination/stereotyping; Involve P in the decision-making; P’s past and present views, wishes, culture; Any Advance Decision or Lasting Power of Attorney who can make that decision; Views of those who care for the welfare of P; Least restrictive option Staff authority to act comes from the MCA The principle: Where the conditions are satisfied, a person who does an act in connection with an incapacitated person’s care or treatment is regarded as having the person’s consent for that act. Negligent acts are not protected, nor are acts that would be illegal if done with consent. New criminal offences: neglect or illtreatment of person lacking capacity Conviction under MCA s. 44, The Green Goblin case Conditions for protection from liability The act is ‘in connection with’ another person’s care or treatment; You have taken ‘reasonable steps’ to establish whether the person lacks capacity; You ‘reasonably believe’ the person lacks capacity; You ‘reasonably believe’ that the proposed act is in the person’s best interests. (MCA s.5) Restraint? You are using restraint if you: Use force (or threaten to use force) to make someone do something they are resisting; Or Restrict a person’s freedom of movement whether they are resisting or not. (MCA s.6(4)) Conditions for restraint If you use restraint you are protected under the MCA if you ‘reasonably believe’: BOTH that it is necessary to use restraint in order to prevent harm to the person, AND That the restraining act is a proportionate response to the likelihood of the person suffering harm and the seriousness of this harm. The effects of restriction must not amount to deprivation of liberty (unless specifically authorised). Munby on the importance of what the person wants or doesn’t want The wishes and feelings of the incapacitated person are an important element in determining what is, or is not, in his best interests. Where he is actively opposed to a course of action, the benefits which it holds for him will have to be carefully weighed against the disadvantages of going against his wishes, especially if force is required to do this. Human rights encourage personalised “least restrictive” care Rights that are at risk in health and social care settings Right to life Right not to be subjected to torture or inhuman or degrading treatment or punishment Liberty and security of person Right to a private and family life Article 8: Right to a private and family life Freedom to text, phone, e-mail or write Right to choose own friends Access to fresh air and exercise Privacy in washing and toilet Privacy for visits Confidentiality of medical records Freedom from intrusion into private life Freedom from searches of living space and person Decisions to interfere with human rights need very careful thought Many rights can be interfered with to some extent, (such as treating a person in their best interests when they lack capacity to give consent), but any interference must be: Allowed by law (inhuman and degrading treatment is NEVER allowed by law) Necessary (in light of risks if you don’t act) Proportionate (don’t use a sledgehammer to crack a nut) Lord Justice Munby on Outcomes: Physical health and safety can sometimes be bought at too high a price in happiness and emotional welfare. The emphasis must be on sensible risk appraisal, not striving to avoid all risk whatever the price, but instead seeking a proper balance and being willing to tolerate manageable or acceptable risks...in particular to achieve the vital good of P’s happiness. What good is it making someone safer if it merely makes them miserable? Encourage Challenges against “Rules of the House” “fossilisation” of risk: You can’t have a phone because one person was abused by direct-sellers; you can’t go out unaccompanied because one resident got lost and had an accident; your family can’t bring in a curry because somebody once got a tummy upset We need person-centred care plans rather than blanket rules Whose job is it to protect human rights? We are required to monitor and report on a number of quality measures to different bodies. Can human rights feel like “just another thing to juggle’”? Staff and family can all be “human rights champions” proactive in scrutinising how people are treated. We all share the responsibility ‘All that is required for evil to prevail is for good people to do nothing.’ (adapted from Edmund Burke, 1770) What does this mean for professionals and for care providers? How can they support whistle blowers? Get it right with FREDA FREDA principles really help: Fairness Respect Equality = FREDA Dignity Autonomy Curtice & Exworthy The Psychiatrist (2010) 34: 150 - 156 Some tentative suggestions about how to create a FREDA culture Piloting (Oxfordshire Health and Social Care, and care providers via the Care Providers Alliance) suggests that a relatively small amount of training empowers people fast Combined with further resources, FREDA makes sense, doesn’t overwhelm with “big law” Empowers service users, relatives and professionals as “human rights champions”, promoting better decision-making, more transparency. Sources of Help and Information Codes of Practice to MCA and DOLS; Department of Justice website: www.justice.gov.uk/guidance Department of Health website: www.dh.gov.uk SCIE website: www.scie.org.uk/mca