the Corporate Compliance Training PPT Here
advertisement

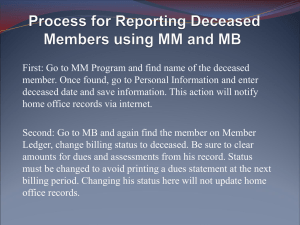
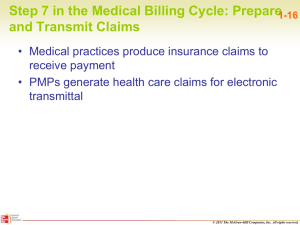
Who, What, Why and When? 1. What is Corporate Compliance and a Compliance Program? 2. Reasons for and Value of an Effective Compliance Program 3. Essential Elements of a Comprehensive Compliance Program 4. Policies, Roles and Responsibilities – Compliance Committee, Compliance Officer 5. What are Some Areas Prone to Non-Compliance? 6. Items or Processes Leading to Non-Compliance 7. Reporting of Non-Compliance 8. How do I Know What is Right or Wrong? The Office of the Inspector General (OIG) lists four aspects of compliance efforts: 1. Establishes a culture within a health care agency that promotes prevention, detection, and resolution of instances of conduct that do not conform to Federal and State law, and Federal, State, and private payer health care program requirements, as well as the health care agency’s business policies. 2. Demonstrates the organization’s commitment to ethical conduct. 3. The existence of benchmarks that demonstrate implementation and achievements are essential to any effective compliance program. 4. Needs to become part of the fabric of routine health care agency operations. Federal Register / Vol. 63, No. 152 / Friday, August 7, 1998 / Notices 42411 The OIG’s guidance calls for: Setting guidelines for ethical and compliant behavior including how to report non-compliance Taking actions – to measure and inspect what we do Using information – benchmarks to improve our daily activities and processes Making compliance a part of our daily behavior Success is the progressive realization of a worthy ideal. -- Earl Nightingale A compliance program provides confidence that the right things are getting done in our daily activities. It helps build a culture that strives to do “right” – We will understand what should be done, how to conduct ourselves, and how to monitor for inappropriate issues which can arise. A compliance program will help Ambercare: Institute and educate staff on best compliance practices from top to bottom Assess and manage our areas at “risk” Provide for open communication and properly handle questions/concerns Establish methods to monitor compliance performance and conduct corrective action 1. Helps meet governance responsibilities “Specifically, compliance programs guide a health care agency’s governing body, Chief Executive Officer (CEO), senior managers, clinicians, billing personnel, and other employees in the efficient management and operation of a health care agency.” OIG’s Guidelines from Federal Register on August 7, 1998, Vol. 63. No. 152/42412 Example: Ambercare’s Executive Committee 2. Helps meet legal requirements “It is incumbent upon a health care agency’s corporate officers and managers to provide ethical leadership to the organization and to assure that adequate systems are in place to facilitate ethical and legal conduct.” OIG’s Guidelines from Federal Register on August 7, 1998, Vol. 63. No. 152/ 42412-3 Example: Ambercare’s Executive Committee 3. Increased enforcement efforts A. B. C. New funding for Medicare and Medicaid Enforcement HEAT (Healthcare Fraud Prevention and Enforcement Action Team) Initiative – OIG, Department of Justice, FBI, CMS New guidance on suspensions of payments and overpayments – HHS may suspend Medicare and Medicaid payments “pending an investigation of a credible allegation of fraud.” Retention of overpayments after 60 days may lead to False Claims Act liability D. E. Triple damages $5,500 to $11,000 per claim Amendments to False Claims Act – expands government and whistleblower options Multiple and growing number of fraud and recovery auditors Eyes are everywhere! 4. Other benefits A. B. C. Fulfill a legal duty to ensure that false or inaccurate claims to Government and private payers are not being submitted Realize additional benefits from the effective compliance program makes good business sense When we can identify weaknesses in our internal systems and management, Ambercare can fulfill our fundamental caregiving mission to our consumers and our community by working more effectively List of major legal and regulatory sources requiring compliance: Medicare Conditions of Participation (CoPs) Civil Monetary Penalties, SSA 1128(a)(5) False Claims Act (FCA) (False Claims Act 31 U.S.C. 3730) (includes Qui Tam provisions) Fraud Enforcement and Recovery Act of 2009 (FERA) Federal and State Wage and Hour Laws HIPPA compliance regulations Patient Freedom of Choice §1802 Self-referral, Kickbacks (Stark, SSA 1877) State False Claims Laws With a Compliance Program, Ambercare… Demonstrates to the community our strong commitment to honest and responsible conduct Protects against fraud, abuse and waste which furthers our mission of achieving and providing quality patient and consumer care Provides clarity by establishing consistent codes of conduct and trust that Ambercare will be consistent and fair with enforcement of that conduct At Ambercare… When our daily, weekly and quarterly activities operate in a compliant manner, the right things are occurring therefore risks are low, quality patient care and organizational effectiveness will be realized. AND – bad things, like poor care, fraud, abuse and waste are not happening in our organization. OIGs’ seven fundamental elements to an effective compliance program are: 1. Implementing written policies, procedures and standards of conduct; 2. Designating a compliance officer and compliance committee; 3. Conducting effective training and education; 4. Developing effective lines of communication; 5. Enforcing standards through well-publicized disciplinary guidelines; 6. Conducting internal monitoring and auditing; and 7. Responding promptly to detected offenses and developing corrective action. Federal Register on August 7, 1998, Vol. 63. No. 152/ 42410 EVERYONE! Compliance involves all of us. It starts at the top with the leaders and affects every level of employee Ambercare’s mission, values and vision statement Adherence to laws and regulations Standards for Business Conduct Code of Personal Conduct or Code of Ethics Confidentiality (HIPAA) and in reporting of non-compliance Billing Whistleblower protection Corporate Compliance Plan Policies are the backbone of the Compliance Program This committee is comprised of staff members from each department and functions to support the Corporate Compliance Officer. Together, they ensure that Ambercare’s compliance program is operating effectively. They meet at least quarterly and report to the Executive Committee annually or more often, if needed. They… Assess the risks and steps being taken to monitor and report such risks; Review updates for compliance policies and any codes of conduct and ethics; Review any significant items concerning compliance with laws and regulations; Evaluate any significant compliance investigations and corrective plans; and Review the knowledge, capabilities, resources, independence and past performance of any external professionals who may be used to assess or support the status of the compliance program. “The Compliance Officer must have the authority to review all documents and other information that are relevant to compliance activities, including, but not limited to, patient records, billing records, and records concerning the marketing efforts of the facility and the home health agency’s arrangements with other parties, including employees, professionals on staff, relevant independent contractors, suppliers, agents, supplemental staffing entities, and physicians. This policy enables the compliance officer to review contracts and obligations (seeking the advice of legal counsel, where appropriate) that may contain referral and payment provisions that could violate the anti-kickback statute, as well as the Stark physician self-referral prohibition and other legal or regulatory requirements.” OIG Guidelines stated in the Federal Register on August 7, 1998, Vol. 63. No. 152/ 42420 Ambercare’s Corporate Compliance Officer is: Joann Strandberg She can be reached at: (505) 861-0060, Ext. 10107 She is the ONLY one who CONFIDENTIALLY MONITORS OUR COMPLIANCE HOTLINE: 1-855-833-0004 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Billing for items or services not actually rendered Billing for medically unnecessary services Giving incentives to actual or potential referral sources Billing for services to patients that are not homebound or do not require a qualifying service Over and under-utilization (visit frequency) Knowingly billing for inadequate or substandard care False dating of amendments to nursing notes Forging beneficiary signatures on visit slips or logs that verify that services were performed Untimely and/or forged physician certifications on plans of care And more Lack of updated information - logs, policies, responsibilities Agreements, activities with no review or prior approvals Personnel acting outside of their stated level of authorities Personnel without proper background or training to do the work Reports or information that is not current or relevant Excessive or unnecessary reports Excessive work arounds and duplications of tasks Poor expenditure control and no budget accountabilities Complaints / Deficiencies with no corrective action taken Lack of compliance education and training No progressive disciplinary guidelines - no linkage to compliance adherence High levels of billing adjustments, no explanations as to why Recent and/or repeated turnover, particularly at supervisory levels Are any of these happening here? Bulletin boards postings Ambernet Report ANONYMOUSLY by calling the toll-free Hotline at 855-833-0004 Leave your message with as much detail as possible o The Corporate Compliance Officer will be the only person accessing that hotline o The CCO will investigate and take appropriate action Disciplinary Action o Intent is to improve your performance o Depends on severity of the misconduct and if the act continues repeatedly o Can be a write-up up to termination o Termination will occur for physical abuse, overt harassment, gross misuse of position, deliberate acts of non-compliance, etc. False claims penalties and judgments Under the False Claims Act the standard of proof for Government prosecutors is only a preponderance of the evidence. In addition, direct knowledge of the bad acts is also not necessary as a liability can be established for "deliberate ignorance" and "reckless disregard" of the truth. o Damages are treble damages and civil fines of $5,000 to $10,000 per claim. For qui tam plaintiffs, rewards are between 15–30 percent of the funds recovered. Also they can receive employment protection for the whistleblower including reinstatement with seniority status, special damages, and double back pay. Defendants in False Claims Action must also pay the successful plaintiff's expenses and attorney's fees. Other sanctions and criminal punishments may be involved. Doing the Right Things Right We want to do what is right for our patients, our community, our organization and ourselves