Pharmacology : Getting to Know Your Drugs
advertisement
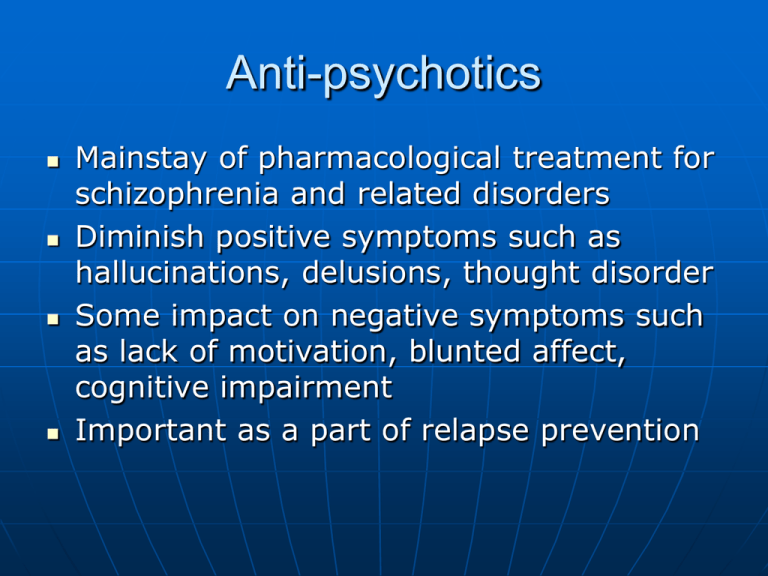
Anti-psychotics Mainstay of pharmacological treatment for schizophrenia and related disorders Diminish positive symptoms such as hallucinations, delusions, thought disorder Some impact on negative symptoms such as lack of motivation, blunted affect, cognitive impairment Important as a part of relapse prevention Anti-psychotics Antagonise dopamine receptors, resulting in anti-psychotic effects Indications-schizophrenia, acute mania, psychotic depression, Conventional and atypical Both of equivalent efficacy when taken at recommended dosages Atypicals have lower incidence of EPSE Dopamine Theory The dopamine hypothesis of psychosis – overactivity of dopamine neurons in the mesolimbic pathway of the brain may mediate the positive symptoms of psychosis Mesolimbic pathway responsible for pleasure, effects of drugs and alcohol and hallucinations and delusions Blockade Of D2 Receptors? D2 ANTAGONIST Nigrostriatal pathway extrapyramidal side effects (EPS) and tardive dyskinesia Mesocortical pathway enhanced negative and cognitive psychotic symptoms Mesolimbic pathway dramatic therapeutic action on positive psychotic symptoms Tuberoinfundibular pathway hyperprolactinemia (lactation, Dopamine Receptors Five subtypes – D2 most important in terms of psychosis Blockade of mesolimbic receptors leads to reduced psychotic symptoms Blockade of the mesocortical pathway leads to increased negative symptoms Dopamine Receptors Dopamine and acetylcholine have a reciprocal relationship• Blockade of dopamine receptors increases the activity of acetylcholine • Over activity of acetylcholine causes EPSE • Blockade of dopamine causes movement disorders in the nigostriatal pathway • Long tem blockade causes “upregulation” and leads to Tardive Dyskinesia Conventional or typical Antipsychotics Have four actions – blockade of: • Dopamine 2 • Muscarinic/choliner gc • Alpha adrenergic • Histamine Serotonin and Dopamine Interactions The Dopamine Receptor Antagonist Hypothesis of Antipsychotic drug Action Blockade of post synaptic dopamine receptors in the mesolimbic pathway is thought to mediate the efficacy of the drug and its ability to diminish positive symptoms Receptor Affinity Low Affinity (loosely bound) - Quetiapine, Olanzapine, Amisulpride, Clozapine High Affinity (tightly bound) - Chlorpromazine, Haloperidol, Flupenthixol, Fluphenazine Tightly bound drugs lead to increased sensitivity to dopamine blockade so more likely to cause EPSE Atypical Antipsychotics Pharmacologic Properties • 5HT2A and D2 antagonism (as opposed to conventional drugs which are D2 without 5HT2A antagonism) • Atypicals – blockade of D2 and 5HT2A Dopamine and Serotonin Receptors Dopamine and serotonin have a reciprocal relationship Serotonin opposes the release of dopamine in the nigrostriatal and tuberofundibular pathways Dopamine and Serotonin Receptors Action of atypicals – firstly binds to the D2 receptor Secondly, binds to the 5HT2A receptor The second action reverses the first – reverses the blockade of D2 Blocking 5HT2A disinhibits the dopamine neuron causing dopamine to pour out Dopamine and Serotonin Receptors The dopamine and serotonin then compete with the drug for the D2 receptor Increased dopamine in the mesocortical pathway Reduction in movement disorders/EPSE for atypical antipsychotics Atypicals In reality – not simple serotonin-dopamine antagonists Most complex pharmacological properties Act on multiple serotonin and dopamine receptors, histamine, alpha adrenergic & cholinergic Atypicals versus conventional All equal efficacy (except Clozapine) Consideration for: • Merits of high versus low affinity drugs • Cerebral selectivity of the drugs • Adverse effect profile • Dose necessary to achieve optimal D2 blockade • Patient tolerability, preference, response Anti-psychotics Conventional – eg chlorpromazine, haloperidol, stelazine, depots such as flupenthixol, zuclopenthixol, fluphenazine Atypical – eg olanzapine, risperidone, quetiapine, amisulpride, clozapine, risperdal consta intramuscular injection, aripiprazole, paliperidone, ziprasidone Also have effects on acetylcholine, histamine,serotonin receptors – Atypical antipsychotics The ‘newer” antipsychotics Effectively treat psychotic symptoms Lower incidence of extra pyramidal side effects than conventional agents Have effects on dopamine, serotonin, histamine and muscarinic receptors Atypical antipsychotics Current atypicals in use in Australia are: Amisulpride Aripiprazole Quetiapine Olanzapine Risperidone Clozapine Ziprasidone Paliperidone Therapeutic effects on symptoms Agitation, sleep and appetite often respond in the first 1-2 weeks Personal hygiene and basic interpersonal socialisation may take 2-3 weeks and psychotic symptoms can gradually decrease over 2-6 weeks An effective trial should be at least 6-8 weeks at doses that are within the prescribed range How long should antipsychotics be taken for? At least 6 months after an acute episode reduces relapse rates If the person experiences another episode they may need antipsychotic medication for 2-5 years before ceasing use For those with multiple episodes, they may need medication for much of their life Adverse Effects Sedation Postural hypotension Anticholinergic effects – dry mouth, blurred vision, constipation, urinary hesitancy Weight gain-clozapine, olanzapine Metabolic effects-increased serum lipids, impaired glucose toleranceclozapine, olanzapine, quetiapine Adverse Effects Hyperprolactinaemia-leads to galactorrhoea, amenorrhoea, decreased libido Sexual dysfunction QTc prolongation-leads to cardiac arrhythmias EPSE-extrapyramidal side effects • Acute dystonias -laryngeal spasm, oculogyric crises • Akathisia-severe sense of agitation, inner restlessness in the limbs, especially the legs Adverse Effects Akathesia – a severe sense of psychomotor agitation Parkinsonism -poverty of movement, tremor, rigidity, drooling, hypersalivation Tardive dyskinesia-involuntary hyperkinetic movements, affects the mouth, lips, tongue, jaws with smacking, tongue writhing, sucking,chewing and tic like movements,limbs and trunk can be affected Adverse Effects Irreversible in some patients Neuroleptic malignant syndrome-rare but potentially fatal – high temp, muscle rigidity, altered consciousness, raised creatinine kinase –cease medication Can happen at anytime during treatment 30% patients will develop syndrome again on rechallenge Depot Anti-psychotics Used when concerns around compliance Conventional-zuclopenthixol(useful for agitated,aggressive,disturbed behaviour) flupenthixol (may have mood elevating effects) fluphenazine -EPSE common Typical-Risperdal Consta – onset of action 3 weeks, need oral Risperidone to supplement until peak Comparative Information for Anti-Psychotics Chlorpromazine, Pericyazine Most sedating, most potent anticholinergic effects, least likely to cause EPSE, most likely to cause orthostatic hypotension. Low potency antipsychotics Trifluperazine, Fluphenazine Moderately sedating, intermediate propensity to cause EPSE, some potential to cause orthostatic hypotension Haloperidol, Droperidol, Thiothixene, Pimozide Least sedating, almost no anticholinergic effects, most likely to cause EPSE, least likely to cause orthostatic hypotension, sometimes referred to as ‘high potency’ antipsychotics Atypical antipsychotics Amisulpride Less potential for weight gain and sedation Aripiprazole May cause insomnia, less potential for hyperprolactinaemia Clozapine Effective treatment-resistant patients but has serious sideeffects (blood dyscrasias, seizures, cardiomyopathy, myocarditis, orthostatic hypotension, sedation, weight gain). Atypical antipsychotics Olanzapine Related to Clozapine may cause sedation, weight gain, peripheral oedema; increased risk of stroke and related mortality in elderly dementia patients Quetiapine Sedating and vasoactive, less potential for hyperprolactinaemia Risperidone, Paliperidone Orthostatic hypotension and hyperprolactinaemia, may be a problem; increased risk of stroke and related mortality in elderly dementia patients Ziprasidone Less potential for weight gain Drug Interactions Cytochrome P450 isoenzymes are significant in psychotropic drug interactions Inducers or inhibitors of this pathway may produce clinically important drug interactions May lead to increase or decrease of medications due to interactions Cytochrome P450 Examples • Fluvoxamine inhibits olanzapine and clozapine metabolism • Smoking induces Olanzapine metabolism • SSRIs inhibit most antipsychotics and therefore increase serum concentrations • Phenytoin reduces serum concentration of Quetiapine • Others – grapefruit juice, Antibiotics, Clozapine Used when previously unresponsive to other antipsychotics Serious adverse effect profile Strict guidelines relating to commencement and monitoring Significant risk of agranulocytosis Trial at least 2 different standard antipsychotics at an adequate dose and for an adequate duration prior to commencing Clozapine Use of antipsychotics with older persons Various disorders treated with antipsychotics in the elderly – psychosis, bipolar affective disorder, delirium & dementia Use extreme caution because of side effect profile ‘Start low & go slow’ (Malone et al 2007) & titrate over longer periods of time to reach the required dose Avoid polypharmacy wherever possible Pregnancy & lactation Avoid antipsychotics if possible Use the lowest effective dose Neonatal adverse effects observed include generalised hypertonicity and dystonic reactions Pregnancy & lactation The safety of atypical agents is yet to be established but preliminary reports there to be no deleterious effects to the foetus Isolated cases of congenital abnormalities with the use of Clozapine Pregnancy & Lactation No increased risk has emerged with the use of Olanzapine The conventional agents are generally preferred Supervised dose reduction and cessation 7-10 days prior to delivery should be considered What other treatments are available? Remember that antidepressant medication is only part of the treatment for antenatal depression and anxiety. Also consider: Psychological therapies Exclude organic illness as a cause of mental health symptoms Address any alcohol and/or illicit substance abuse Assess the social situation General lifestyle measures: adequate rest/sleep, balanced diet, exercise The decision to treat should be made on an individual case basis Conclusion Conventional and atypical antipsychotics are used as the foundation for pharmacological management of schizophrenia and related psychosis All have equal efficacy, exception Clozapine Atypicals generally better tolerated & have less EPSE Atypicals first line treatment Start lowest effective possible dose & titrate upwards Ongoing monitoring & management of adverse effects Caution numerous drug interaction & potential for neuroleptic malignant syndrome Resources Therapeutic Guidelines – Psychotropic Version 5 www.tg.com.au 9329 1566 Australian Medicines Handbook www.amh.net.au 08 8303 6977 MIMS online http://www.ppmis.org.au Perinatal Psychotropic Medicine Information Service