Chapter 12

Chapter 12
Personality Disorders
Personality Disorders: An Overview
Enduring and pervasive predispositions
Perceiving
Relating
Thinking
Inflexible and maladaptive
Distress
Impairment
Coded on Axis II
Personality Disorders
10 specific personality disorders
Several under review for DSM-V
3 clusters
High comorbidity with Axis I disorders
Poorer prognosis
Therapist reactions
Countertransference
Personality Disorders: An Overview
Categorical vs. Dimensional Views
“Kind” vs. “Degree”
DSM is categorical
Reifies concepts
Less flexible
Loss of individual information
Sometimes arbitrary
Personality Disorders: An Overview
Five factor model of personality (“Big Five”)
Openness to experience
Conscientiousness
Extraversion
Agreeableness
Emotional stability
DSM Personality Disorder Clusters
Cluster A
Odd or eccentric
Paranoid, schizoid, schizotypal
Cluster B
Dramatic, emotional, erratic
Antisocial, borderline, histrionic, narcissistic
Cluster C
Fearful or anxious
Avoidant, dependent, obsessive-compulsive
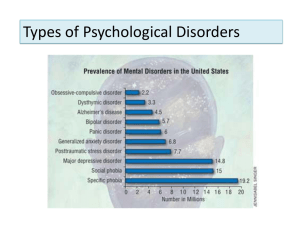
Personality Disorders: Facts and Statistics
Prevalence = 0.5 - 2.5%, may be closer to 10%
Outpatient = 2 - 10%
Inpatient = 10 – 30%
Origins and Course
Begin in childhood
Chronic course
High comorbidity
Personality Disorders: Gender Differences
Differences in diagnostic rates
Borderline (75% female)
Clinician bias
Assessment bias
Measures
Criterion bias
Histrionic = extreme “stereotypical female”
No “macho” disorder
Personality Disorders: Gender Differences
Personality Disorders Under Study
Individual disorders
Sadistic
Self-defeating
Categories of disorders
Depressive
Negativistic
Passive aggressive
Cluster A: Paranoid Personality Disorder
Clinical Description
Mistrust and suspicion
Pervasive
Unjustified
Few meaningful relationships
Volatile
Tense
Sensitive to criticism
Cluster A: Paranoid Personality Disorder
Causes
Possible relationship to schizophrenia
Possible role of early experience
Trauma
Abuse
Learning
“World is dangerous”
Cluster A: Paranoid Personality Disorder
Treatment
Unlikely to seek on own
Crisis
Focus on developing trust
Cognitive therapy
Assumptions
Negative beliefs
No empirically-supported treatments
Cluster A: Schizoid Personality Disorder
Clinical Description
Appear to neither enjoy nor desire relationships
Limited range of emotions
Appear cold, detached
Appear unaffected by praise, criticism
Unable or unwilling to express emotion
No thought disorder
Cluster A: Schizoid Personality Disorder
Causes
Limited research
Precursor: childhood shyness
Possibly related to:
Abuse/neglect
Autism
Dopamine
Cluster A: Schizoid Personality Disorder
Treatment
Unlikely to seek on own
Crisis
Focus on relationships
Social skills therapy
Empathy training
Role playing
Social network building
No empirically-supported treatments
Cluster A: Schizotypal Personality Disorder
Clinical Description
Psychotic-like symptoms
Magical thinking
Ideas of reference
Illusions
Odd and/or unusual
Behavior
Appearance
Socially isolated
Highly suspicious
Cluster A: Schizotypal Personality Disorder
Causes
Schizophrenia phenotype?
Lack full biological or environmental contributions
Preserved frontal lobes
Cognitive impairments
Left hemisphere?
More generalized?
Cluster A: Schizotypal Personality Disorder
Treatment Options
Treatment of comorbid depression
Multidimensional approach
Social skill training
Antipsychotic medications
Community treatment
Cluster B: Antisocial Personality Disorder
Clinical Description
Noncompliance with social norms
“Social Predators”
Violate rights of others
Irresponsible
Impulsive
Deceitful
Lack a conscience, empathy, and remorse
Cluster B: Antisocial Personality Disorder
Nature of psychopathy
Glibness/superficial charm
Grandiose sense of self-worth
Proneness to boredom/need for stimulation
Pathological lying
Conning/manipulative
Lack of remorse
Overlap with ASPD, criminality
Intelligence
Cluster B: Antisocial Personality Disorder
Cluster B: Antisocial Personality Disorder
Cluster B: Antisocial Personality Disorder
Developmental considerations
Early histories of behavioral problems
Conduct disorder
Families history of:
Inconsistent parental discipline
Variable support
Criminality
Violence
Causes of Antisocial Personality
Gene-environment interaction
Genetic predisposition
Environmental triggers
Arousal hypotheses
Underarousal
Fearlessness
Causes of Antisocial Personality
Gray’s model of brain functioning
Behavioral inhibition system (BIS)
Low
Reward system (REW)
High
Fight/flight system (F/F)
Causes of Antisocial Personality
Interactive, integrative model
Genetic vulnerability
Neurotransmitters
Environmental factors
Family stress
Reinforcement of antisocial behaviors
Alienation from good role models
Poor occupational/social function
Antisocial Personality Disorder
Treatment
Unlikely to seek on own
High recidivism
Incarceration
Early intervention
Parent training
Prevention
Rewards for pro-social behaviors
Skills training
Improve social competence
Cluster B: Borderline Personality Disorder
Clinical Description
Patterns of instability
Labile, intense moods
Turbulent relationships
Impulsivity
Fear of abandonment
Very poor self-image
Self-mutilation
Suicidal gestures
Cluster B: Borderline Personality Disorder
Comorbid disorders
Depression – 24-74%
Suicide – 6%
Bipolar – 4-20%
Substance abuse – 67%
Eating disorders
25% of bulimics have BPD
Cluster B: Borderline Personality Disorder
Causes
Genetic/biological components
Serotonin
Frontolimbic circuit
Cognitive biases
Early childhood experience
Neglect
Trauma
Abuse
Cluster B: Borderline Personality Disorder
Treatment
Highly likely to seek treatment
Antidepressant medications
Dialectical behavior therapy
Reduce “interfering” behaviors
Self-harm
Treatment
Quality of life
Outcomes
Demonstrated efficacy
Cortical activation changes
Cluster B: Borderline Personality Disorder
Cluster B: Histrionic Personality Disorder
Clinical Description
Overly dramatic
Sensational
Sexually provocative
Impulsive
Attention-seeking
Appearance-focused
Impressionistic
Vague, superficial speech
Common diagnosis in females
Cluster B: Histrionic Personality Disorder
Causes
Little research
Links with antisocial personality
Sex-typed alternative expression?
Cluster B: Histrionic Personality Disorder
Treatment
Problematic interpersonal behaviors
Attention seeking
Long-term consequences of behavior
Little empirical support
Cluster B: Narcissistic Personality Disorder
Clinical Description
Exaggerated and unreasonable sense of self-importance
Require attention
Lack sensitivity and compassion
Sensitive to criticism
Envious
Arrogant
Cluster B: Narcissistic Personality Disorder
Causes
Deficits in early childhood learning
Altruism
Empathy
Sociological view
Increased individual focus
“Me generation”
Cluster B: Narcissistic Personality Disorder
Treatment focuses on:
Grandiosity
Lack of empathy
Hypersensitivity to evaluation
Co-occurring depression
Little empirical support
Cluster C: Avoidant Personality Disorder
Clinical Description
Extreme sensitivity to opinions
Avoid most relationships
Interpersonally anxious
Fearful of rejection
Cluster C: Avoidant Personality Disorder
Causes
Sub-schizophrenia disorder?
Difficult temperament
Early parental rejection
Interpersonal isolation and conflict
Cluster C: Avoidant Personality Disorder
Treatment
Similar to social phobia
Increase social skills
Reduce anxiety
Importance of therapeutic alliance
Moderate empirical support
Cluster C: Dependent Personality Disorder
Clinical Description
Rely on others for major and minor decisions
Unreasonable fear of abandonment
Clingy
Submissive
Timid
Passive
Feelings of inadequacy
Sensitivity to criticism
High need for reassurance
Cluster C: Dependent Personality Disorder
Causes
Little research
Early experience
Death of a parent
Rejection
Attachment
Cluster C: Dependent Personality Disorder
Treatment
Limited empirical support
Caution: dependence on therapist
Gradual increases in:
Independence
Personal responsibility
Confidence
Cluster C: Obsessive-Compulsive Personality Disorder
Clinical Description
Fixation on doing things the “right way”
Rigid
Perfectionistic
Orderly
Preoccupation with details
Poor interpersonal relationships
Obsessions and compulsions are rare
Cluster C: Obsessive-Compulsive Personality Disorder
Causes
Limited research
Weak genetic contributions
Predisposed to favor structure?
Cluster C: Obsessive-Compulsive Personality Disorder
Treatment
Similar to OCD
Address fears related to the need for orderliness
Decrease:
Rumination
Procrastination
Feelings of inadequacy
Limited efficacy data
Personality Disorders: Future Directions
Completely rethinking personality disorders
Dimensional models