Slides - Projects In Knowledge
advertisement
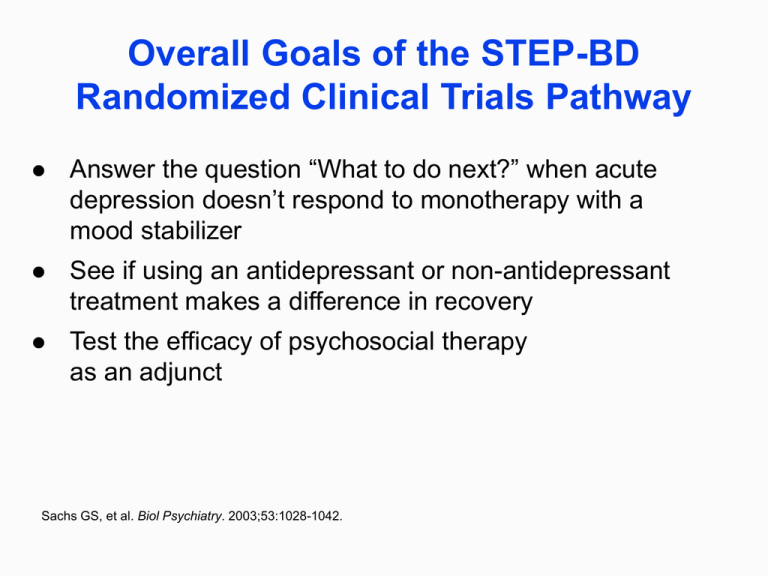
Overall Goals of the STEP-BD Randomized Clinical Trials Pathway Answer the question “What to do next?” when acute depression doesn’t respond to monotherapy with a mood stabilizer See if using an antidepressant or non-antidepressant treatment makes a difference in recovery Test the efficacy of psychosocial therapy as an adjunct Sachs GS, et al. Biol Psychiatry. 2003;53:1028-1042. Overview—Randomized Clinical Trials Interventions Duration Outcomes Acute depression1 Mood stabilizer + antidepressant: bupropion or paroxetine 26 weeks No increased risk of TEAS Recovery rates: 24% on MS + either antidepressant 27% on MS + placebo No benefit seen from adding an antidepressant Refractory depression2 Mood stabilizer + nonantidepressant adjunct: lamotrigine, inositol, or risperidone 16 weeks Recovery rates: 24% on lamotrigine, 17% on inositol, 5% on risperidone No statistical difference in the 3 adjuncts; no additive benefit in treating depression Ad hoc analyses: lamotrigine may have some modest therapeutic benefit Psychosocial therapy3 (for treating depression) Adjunctive treatment for acute depression: CBT, FFT, or IPSRT Control: CC 1 year Recovery rates: 77% in FFT, 64.5% in ISPRT, 60% in CBT, 51.5 in CC All 3 intensive psychotherapies were statistically superior to CC; all 3 also had clear benefits of patients becoming well sooner and staying well longer Abbreviations: CBT, cognitive behavioral therapy; CC, Collaborative Care; FFT, family-focused psychoeducational treatment; IPSRT, Interpersonal Social Rhythm Therapy; MS, Mood Stabilizer; TEAS, treatment-emergent affective switch. 1. Sachs GS, et al. N Engl J Med. 2007;356:1711-1722. 2. Nierenberg AA, et al. Am J Psychiatry. 2006;163:210-216. 3. Miklowitz DJ, et al. Arch Gen Psychiatry. 2007;64:419-427. Advantages of Using Intensive Psychotherapy as an Adjunct Patients were 1.6 times more likely to be well in any given study month if they received intensive psychotherapy Patients became well an average of 110 days faster than those in collaborative care Miklowitz DJ, et al. Arch Gen Psychiatry. 2007;64:419-427. Risk Factors that Increase the Chance of Recurrence after Recovery If any of the following happened the year prior to recovery from an acute episode, the risk of recurrence increased: Previous lifetime episodes >20 Number of residual symptoms – For every depressive symptom remaining, risk increases by 14% – For every manic symptom remaining, risk increases by 20% Length of time spent in prior episode (longer = worse) Length of time with anxiety symptoms (longer = worse) Miklowitz DJ, et al. Arch Gen Psychiatry. 2007;64:419-427. Recovery and Recurrence in STEP-BD Entered STEP-BD symptomatic Only ~1/4 of the cohort in this study achieved recovery without a relapse in ≤2 years Achieved recovery 1469 858 58% Perlis RH, et al. Am J Psychiatry. 2006;163:217-224. Recurrence within 2 years 416 41% Ancillary Anxiety Study in STEP-BD ANY current anxiety disorder increases the risk of an earlier acute recurrence1 Presence of anxiety disorder causes, on average, a loss of 39 days being well1 As the number of anxiety disorders increase, it increases the loss of days being well1 Anxiety disorders also increase suicide risk2 In the 239 STEP-BD patients who were tracked for a year in follow-up, 41% of the patients with at least 1 anxiety disorder relapsed1 1. Otto MW, et al. Br J Psychiatry. 2006;189:20-25. 2. Simon NM, et al. J Psychiatr Res. 2007;41:255-264. Ancillary ADHD Study in STEP-BD In bipolar children, ADHD co-occurs 60%–90% of the time This comorbidity has not been studied at length in adults STEP-BD showed that bipolar adults with ADHD – Have a poorer prognosis with bipolar disorders – Are more symptomatic – Are less likely to recover from mood episodes – Are more likely to have more mania episodes – Are more at risk for other psychiatric comorbidities Nierenberg AA, et al. Biol Psychiatry. 2005;57:1467-1473. Functional Impairment After Recovery Followed 103 STEP-BD subjects who had been in remission at least 4 weeks The Work and Social Adjustment Scale (WSAS) was used to assess overall functional status Findings: bipolar patients still have substantial functional deficits even during periods of sustained remission (in this cohort, 4 weeks to 13 years) Degree of functional impairment correlates with degree of residual depressive symptoms (but not panic/mania symptoms) Patients may benefit from comprehensive psychosocial and rehabilitative interventions Nierenberg AA, et al. Biol Psychiatry. 2005;57:1467-1473. Take-Away Messages Despite best efforts, recurring illness is still too common in bipolar disorders The value of antidepressants as adjunctive therapy in acute bipolar depression has yet to be established Nonantidepressant adjunctive therapy may have modest benefits in refractory bipolar depression Intensive psychotherapy has value as perhaps the most useful adjunct to pharmacotherapy in treating bipolar depression Careful evaluations tracking patient symptoms at recovery can help alter recurrences The most important single independent predictor of risk was residual, subthreshold mood elevation symptoms Thase ME. Curr Psychiatry Rep. 2007;9:497-503. Suggested Readings Fagiolini A, Kupfer DJ, Masalehdan A, et al. Functional impairment in the remission phase of bipolar disorder. Bipolar Disord. 2005;7:281-285. Miklowitz DJ, Otto MW, Frank E, et al. Psychosocial treatments for bipolar depression. Arch Gen Psychiatry. 2007;64:419-427. National Institute of Mental Health. Effectiveness of Lithium Plus Optimized Medication in Treating People With Bipolar Disorder (LiTMUS). http://clinicaltrials.gov/show/NCT00667745. Accessed November 8, 2008. Nierenberg AA, Ostacher MJ, Calabrese JR, et al. Treatment-resistant bipolar depression: a STEP-BD equipoise randomized effectiveness trial of antidepressant augmentation with lamotrigine, inositol, or risperidone. Am J Psychiatry. 2006;163:210-216. Perlis RH, Brown E, Baker RW, Nierenberg AA. Clinical features of bipolar depression versus major depressive disorder in large multicenter trials. Am J Psychiatry. 2006;163:225-231. Perlis RH, Ostacher MJ, Patel JK, et al. Predictors of recurrence in bipolar disorder: primary outcomes from the Systemic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry. 2006;163:217224. Post RM, Altschuler LL, Leverich GS, et al. Mood switch in bipolar depression: comparison of adjunctive venlafaxine, bupropion and sertraline. Br J Psychiatry. 2006;189:124-131. Sachs GS, Nierenberg AA, Calabrese JR. Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med. 2007;356:1711-1722. Suppes T, Dennehy EB, Hirschfield R, et al. The Texas implementation of medication algorithms: update to the algorithms for treatment of bipolar I disorder. J Clin Psychiatry. 2005;66:870-886. www.grandrounds.com/v66n0710.pdf. Accessed November 8, 2008. Suppes T, Leverich GS, Keck PE, et al. The Stanley Foundation Bipolar Treatment Outcome Network II. Demographics and illness characteristics of the first 261 patients. J Affect Disord. 2001;67:45-59.