Co-Occurring Disorders
Co-Occurring Disorders
J. H. Shale, MD, JD
Psychiatric Director Serenity House, Abilene, TX
Clinical Prof. UCSD School of Medicine, San Diego, CA
Overview
• Definitions of terms
• Propositions
• Statistics
• Diagnosis v. Misdiagnosis
• Treatment
Definitions 1
• Dual Diagnosis (DD) was an early term used for the presence of a mental disorder and a SADO
• DD has been used interchangeably with Co-occurring disorders and co-morbidity.
• But DSM IV TR also uses co-morbidity to describe two mental disorders in the same person
• And DSM IV TR does not define any of these terms
• Here we use any of these terms in the original sense
Mental DO + SADO
Definitions 2
• Serious persistent mental illness
• Public systems often have a limited spectrum of disorders that qualify for treatment
• LA and SD County and MHMR here in TX
• SCZ, SczAff DO, Bipolar DO and MDD, maybe
BPDO and less often Anxiety DO’s
• SADO are usually treated in a parallel system if at all
• This has a huge impact on the quality of DX
Definitions 3
• DSM Axis I = clinical disorders and SADO
• DSM Axis II = MR and PDO’s
• DSM III = general medical conditions
• DSM IV = Psychosocial/environmental problems
• DSM V = GAF
• This has a huge impact on the quality of DX
Proposition 1
Persons with SADO are at increased risk to develop mental disorders.
Persons with mental disorders are at increased risk to develop SADO
There is a clear consensus on this proposition, the only controversy is about the magnitude
Proposition 2
There is a major tendency to misdiagnose these cooccurring disorders.
This results in both over and under diagnosis
Statistics
The mark of a truly educated man is to be moved deeply by statistics.
Geo. B. Shaw
There are lies, damn lies and statistics
Mark Twain
Problems getting good data
• Denial
– Folks with SADO don’t tend to admit it
• Poor History taking
– don’t ask, don’t tell
• Lack of experience and training in SADO
• Politics
• Confusion on rules for Dx
– Tendency to over Dx
– Rule of parsimony
Schizophrenia
• Lifetime Prevalence 1% - 1.5%
• Alcohol abuse/dep 24%
• Drug abuse/dep 14%
• Life expectancy 20% less than Gen pop
• Suicide rates > 15%
• Smoking 80 %
• Diabetes rates 1.5 times matched controls
Schizophrenia Dx
• A. Sx’s
– delusions (bizarre), hallucinations, disorganized thinkng
(speech/behavior, includes catatonia) neg sx’s of flat affect alogia, avolition. Active sx’s for at least a month
• B. social/occupational dysfunction
• C. Duration at least 6 months
• D. Exclusions: MDD, BPDO1, SczAffective DO
• E. Exclusions: SADO, gen med condition
• F. Relation to Autism/ Pervasive DDO
– prominent Hallucination/Delusion for at least a month
Major Depressive Disorder
• Lifetime Prevalence 18%
• Early use of ETOH, tobacco, drugs increases risk of
MDD and may cause earlier onset of MDD
• “former drinkers” at 4 fold risk of MDD in the period measured ( 1-4 yrs abstinent)
• Question is to what extent A causes B
– Texas Sharpshooter Fallacy
Major Depressive Disorder Dx
• Sx’s 5 or more of following and 1 or 2 must be among them:
1.depressed mood, 2. Diminished interest
– wgt change >5% in a month, insomnia/hypersomnia, psychomotor agitation/retardation, decreased energy, guilt/worthlessness, decreased concentration, recurrent thoughts of death/ SI/SA
• Exclude mixed episode (Dx of BPDO1)
• Sig interfere with major area of life function
• Not due to SADO, meds or med. Condition
• Sx’s are not form bereavement
• Sx’s duration > 2 month
Bipolar Disorder I Mania
• Distinct period at least a week of persistently elevated or expansive or irritable mood
• Sx’s 3 or more of: grandiosity/inflated self-esteem, decreased sleep, increased talk/pressured speech, thoughts racing/flgt of ideas, distractable, can’t focus, increase goal directed activity, psychmotor agitation, excessive involvement in sex, spending, or risk taking with potential for harm (poor jusdgment)
• exclude mixed episode (sx’s of both mania and dep)
• Sig interferes with major area of life function
• Excludes SADO or meds or Med condition
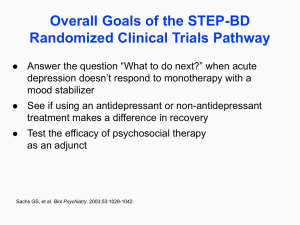
Bipolar Disorder in Clinical Populations
Patients Treated for Depression in Community Psychiatry
602 outpatients receiving treatment for unipolar depression with at least 1 failed antidepressant trial
19% screened positive* for bipolar disorder
• The average number of failed antidepressants was 2.9
• No significant differences seen in rate of positive MDQ screens based on # of failed antidepressants
*Using the Mood Disorder Questionnaire (MDQ)
Calabrese JR, et al. MedGenMed. 2006;8.
Bipolar Disorder Symptoms Are
Chronic and Predominantly Depressive
1% 2%
9%
6%
53%
50%
46%*
32%
146 bipolar I patients followed 12.8 years
% of Weeks
Asymptomatic
Depressed
Manic/hypomanic
Cycling/mixed
Judd LL, et al. Arch Gen Psychiatry . 2002;59:530-537.
Judd LL, et al. Arch Gen Psychiatry. 2003;60:261-269.
86 bipolar II patients followed 13.4 years
*%s do not add to 100 due to rounding
Epidemiology
•
Bipolar disorder is estimated to affect approximately 3.7% of the US population 1
•
Disease onset at 15 to 24 years of age, but accurate diagnosis may take 5 to
10 years 1,2
•
Equal incidence in men and women 2
1 Hirschfeld RMA, et al. J Clin Psychiatry.
2003;64:53-59.
2 Evans DL. J Clin Psychiatry.
2000;61(suppl 13):26-31.
Epidemiology
• 15% to 20% of untreated patients succeed in committing suicide 1
• High recurrence rate of bipolar disorder 2
• High economic burden 2
• Bipolar is a multidimensional disease 1,3
1 Evans DL. J Clin Psychiatry . 2000;61(suppl 13):26-31.
2 Woods SW. J Clin Psychiatry . 2000;61(suppl 13):38-41.
3 Goodwin FK, et al. In: Goodwin FK, Jamison KR, eds. Manic-
Depressive Illness .
New York, NY: Oxford University Press; 1990:74-84.
Bipolar Disorder:
Unrecognized and Underdiagnosed
Mood Disorders Questionnaire
Positive Rates (US Population)
Prevalence of bipolar I and II disorder*
Correctly diagnosed by a doctor as having bipolar disorder
Incorrectly diagnosed as unipolar depression
Not diagnosed as bipolar disorder or unipolar depression
3.7%
20%
31%
49%
* Weighted to match national demographics
† When adjusted for frequency of bipolar disorder in nonresponders
Hirschfeld RMA, et al. J Clin Psychiatry .
2003;64:161-174.
†
Cross Addiction
The APA Glossary, 8 th Ed. 2003 defines crossdependence: “ A drug’s ability to suppress physical manifestations of substance dependence produced by another drug and to maintain the physically dependent state. It provides the rationale for the treatment of dependence on one substance, such as alcohol, by the short-term substitution of a less dangerous and more controllable substance that is cross-dependent with alcohol (e.g. Librium, [chlordiazepoxide]) to treat the symptoms of alcohol withdrawal.”
Cross Addiction
It has become a staple of teaching in addiction medicine that one should not use potentially addicting medications in patients with a history of substance abuse or dependence if it can be avoided.
Reasons For Misdiagnosis
• Problems getting good data
• Statistical issues and definitions of terms
• Payment mis-incentives
• Changing roles of “mental health professionals”
• Ignorance and sloth, maybe greed
– TDPS: Harris county docs rank first in prescribing a combo of three highly addictive meds that give a “heroin high”
– hydrocodone, alprazolam and carisoprodol
– C.M. Schade, MD past president of TX Pain Society: No legitimate medical reason for this combo. (Temple Sentinel,
B1, 6/1/10)