The Long-Term Outcomes Literature for Psychiatric Medications
advertisement

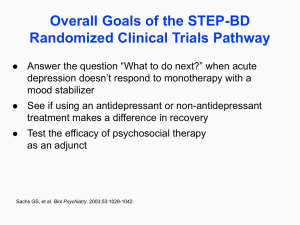
Citations for Many of Studies Discussed in Talk “If we wish to base psychiatry on evidence-based medicine, we run a genuine risk in taking a closer look at what has long been considered fact.” --Emmanuel Stip, European Psychiatry, 2002 Many of these studies can be downloaded from madinamerica.com, or from roberwhitaker.org. Also, key findings are often to be found in data tables, or in the text of the article, as opposed to the abstract. I. Schizophrenia/Antipsychotics A. Outcomes from 1945 to 1955 (pre-drug) 1. Sixty-two percent of first-episode psychotic patients admitted to Warren State Hospital from 1946 to 1950 were discharged within 12 months. At end of three years, 73 percent were living in the community. J. Cole, editor, Psychopharmacology (National Academy of Sciences, 1959):142. 2. In a study 216 schizophrenia patients admitted to Delaware State Hospital from 1948 to 1950, six years after initial hospitalization 70% were successfully living in the community. Cole, ibid. 3. In studies of schizophrenia patients in England (where the disorder was more narrowly defined), 33% enjoyed a complete recovery, and another 20 percent a social recovery, which meant they could support themselves and live independently. Warner, Recovery from Schizophrenia (Routledge, 1985), 74. B. California’s 1961 Report 1. In a study of all 1,413 first-episode schizophrenia patients hospitalized in California in 1956, 88 percent of those who weren’t medicated were discharged within 18 months, compared to 74 percent of those treated with a neuroleptic. Epstein, “An approach to the effect of ataraxic drugs on hospital release rates,” AJP 119 (1962):246-61. C. Long-Term Studies, 1960s and 1970s 1. NIMH’s first follow-up study. At end of one year, patients who were treated with placebo upon initial admission to hospital “were less likely to be rehospitalized than those who received any of the three active phenothiazines.” N. Schooler. “One year after discharge.” AJP 123 (1967):986995. 2. Comparison of Outcomes in the pre-Thorazine era and the post-Thorazine era. 45% percent of the patients treated at Boston Psychopathic Hospital in 1947 did not relapse in the five years following discharge; 76% were successfully living in the community at the end of that follow-up period. In contrast, only 31% of patients treated in 1967 with drugs at a Boston community health center remained relapse-free for the next five years, and as a group they were much more "socially dependent" than those in the 1947 cohort. Bockoven. “Comparison of two five-year follow-up studies.” AJP, 132 (1975): 796-801. 3. 1977 in-house NIMH study 35% percent of the non-medicated patients relapsed within a year after discharge, compared to 45% of drug-treated patients. Medicated patients suffered more from depression, blunted emotions, and retarded movements. Carpenter. “The treatment of acute schizophrenia without drugs.” AJP 134 (1977): 14-20. 4. NIMH-funded three year study, 1970s 27% of newly diagnosed schizophrenia patients treated initially without drugs in the hospital relapsed in the three years following discharge, compared to 62% of the medicated group. Of the 41 patients initially treated without antipsychotics, 24 remained unexposed to antipsychotics at end of three years, and this group had by far the best overall outcomes. Rappaport. “Are there schizophrenics for whom drugs may be unnecessary or contraindicated?” International Pharmacopsychiatry 13 (1978):100-111 5. Loren Mosher’s Soteria project, 1970s Treatment in homelike environment (Soteria), where antipsychotics were minimally used, compared to conventional treatment in a hospital setting. At the end of two years, the Soteria patients had “lower psychopathology scores, fewer (hospital) readmissions, and better global adjustment” than those treated conventionally with antipsychotics. Medication use at Soteria: 42 percent never exposed to antipsychotics; 39% only on a temporary basis; 19% on a continual basis. Mathews, “A non-neuroleptic treatment of schizophrenia.” Schizophrenia Bulletin 5 (1979), 322-332. Bola, “Treatment of acute psychosis without neuroleptics.” J Nervous and Mental Disease 191 (2003):219-229. D. A Biological Explanation for Increased Chronicity 1. Drug-induced supersensitivity psychosis Physicians at McGill University in Montreal explain that antipsychotics trigger an increase in the density of dopamine receptors, and they reason that this dopamine supersensitivity makes the patient more biologically prone to psychosis and to worse relapses upon drug withdrawal. Chouinard. “Neuroleptic-induced supersensititivity psychosis.” AJP 135 (1978):1409-1410. Chouinard. “Neuroleptic-induced supersensitivity psychosis.” AJP 137 (1980):16-20. 2. Tardive dyskinesia, tardive psychosis, and tardive dementia When patients stay on neuroleptics indefinitely, the dopaminergic pathways begin to become permanently dysfunctional. Dysfunction in the limbic system leads to tardive psychosis, which develops at the rate of 3% per year. Chouinard, “Neurolepticinduced supersensitivity psychosis, the ‘hump course,’ and tardive dyskinesia.” J Clinical Psychopharmacology 2 (1982):143-4. Chouinard, “Severe cases of neuroleptic induced supersensitivity psychosis.” Schizophrenia Research 5 (1991):21-23. E. Twenty-five Years of Confirming Evidence 1. MRI Studies In the 1990s, researchers report that antipsychotics shrink the frontal lobes and cause an enlargement of the basal ganglia. a) University of Pennsylvania study Swelling of basal ganglia and thalamus is “associated with greater severity of both negative and positive symptoms.” Gur, “Subcortical volumes in neuroleptic naïve and treated patients with schizophrenia.” AJP 155 (1998):1711-17. Gur, “A followup magnetic resonance imaging study of schizophrenia.” Arch Gen Psychiatry 55 (1998):145-152. b) Nancy Andreasen’s study Shrinkage of frontal lobes is associated with a worsening of negative symptoms, functional impairment, and cognitive decline. (Disease may cause shrinkage, which drugs then exacerbate.) Ho, “Progressive structural brain abnormalities and their relationship to clinical outcomes,” Arch Gen Psychiatry 60 (2003):585-94. Andreasen. “Longitudinal changes in neurocognition during the first decade of schizophrenia illness.” International Congress on Schizophrenia Research (2005):348. Dreifus. “Using imaging to look at changes in the brain.” New York Times, September 16, 2008. 2. Observational studies a) The Vermont Longitudinal Study Twenty years after release from back wards of Vermont State Hospital, one-third of schizophrenia patients completely off medications an recovered. Harding, “The Vermont longitudinal study of persons with severe mental illness, II. AJP 144 (1987):727-734. Hardin “Empirical correction of seven myths about schizophrenia with implications for treatment.” ACTA Psychiatrica Scandinavica 90, suppl. 38 (1990):140-146. b) World Health Organization studies In two studies, outcomes for schizophrenia patients in “developing” countries were much better than outcomes in the U.S. and other “developed” countries. In developing countries, 15.9% of patients were continuously maintained on neuroleptics, compared to 61% of patients in the developed countries. Jablensky. “Schizophrenia: manifestations, incidence and course in different cultures.” Psychological Medicine, supplement 20 (1992):1-95. c) Martin Harrow’s NIMH-Funded study Outcomes for schizophrenia patients at end of 15 years: On Medication Recovered Fair Poor Off Medication 5% 46% 49% 40% 44% 16% Harrow. “Factors involved in outcome and recovery in schizophrenia not on antipsychotic medications.” J Nerv and Mental Disease, 195 (2007): 407-414. F. An Evidence-Based Model for Promoting Long-Term Recovery Open-dialogue therapy in Western Lapland At the end of five years 79% of the patients did not have psychotic symptoms, 80% had returned to school or were working, and only 20% were on a disability allowance. Only 33% had ever been exposed to an antipsychotic during the five years, and only 20% were on antipsychotics at the end of the study. Seikkula, “Five-year experience of first-episode nonaffective psychosis in open-dialogue approach.” Psychotherapy Research 16 (2006):214-228 II. Depression/Antidepressants A. In pre-drug era, natural recovery rates from depressive episodes are high. Cole, “Therapeutic efficacy of antidepressant drugs,” JAMA 190 (1964):448-55. Kline, “The practical management of depression,” JAMA 190 (1964):122-30. Winokur, Manic Depressive Illness (St. Louis: The C.V. Mosby Company, 1969):19. Schuyler, The Depressive Spectrum (New York: Jason Aronson, 1974):47. B. Physicians report that depression is changing to more chronic course with introduction of antidepressants Van Scheyen, “Recurrent vital depressions,” Psychiatria, Neurologia, Neurochirurgia 76 (1973): 93-112. C. High relapse rates following drug exposure In metanalysis of the literature, Harvard researchers report that fifty percent of patients withdrawn from antidepressants relapse within 14 months. The longer the exposure to the drug, the greater the relapse rate. Viguera, “Discontinuing antidepressant treatment in major depression,” Harvard Review of Psychiatry 5 (1998):293-305. NIMH study, after 18 months, stay well rate is highest for cognitive therapy group (30%), and lowest for imipramine group (19%). Shea, “Course of symptoms over follow-up,” Arch Gen Psychiatry 49 (1992):782-87. D. Giovanna Fava raises possibility that antidepressants are turning depression into a chronic disorder Fava, “Do antidepressant and antianxiety drugs increase chronicity in affective disorders?” Psychotherapy and Psychosomatics 61 (1994):125-31. Fava, “Can long-term treatment with antidepressant drugs worsen the course of depression?” J Clin Psychiatry 64 (2003): 123-33. E. Naturalistic studies 1. Dutch study of ten-year outcomes of 222 people who suffered a first episode of depression. 76% of those not treated with an antidepressant recovered and never relapsed, compared to 50 percent of those prescribed a drug. Weel-Baumgarten, “Treatment of depression related to recurrence,” J Clin Pharmacy and Therapeutics 25 (2000):61-66. 2. Canadian study of 9,508 depressed patients for five years. Those who took antidepressants were symptomatic on average 19 weeks per year, versus 11 weeks for those not on medication. Patten, “The impact of antidepressant treatment on population health.” Population Health Metrics 2 (2004): 9. 3. WHO screening study of 740 people conducted in 15 cities. At end of year, those who weren’t exposed to drugs had much better “general health;” their symptoms were milder; and a lower percentage were judged to still be mentally ill. Goldberg, “The effect of detection and treatment on the outcome of major depression in primary care,” Brit J of General Practice 48 (1998):184044. 4. Ontario study of 1,281 people who went on short-term disability for depression. Only 9 percent of those who didn’t take an antidepressant went on to long-term disability, versus 19 percent of those who took an antidepressant. Dewa, “Depression in the workplace,” A report to the Ontario Roundtable on appropriate prescribing,” Nov. 2001. 5. In six year study by NIMH researchers, depressed people who got treated were three times more likely to suffer a cessation of their principal social role, and seven times more likely to become incapacitated than those who didn’t get treated. Coryell, “Characteristics and significance of untreated major depressive disorder,” AJP 152 (1995):1124-29. F. Course of unmedicated depression today NIMH study of untreated major depression; Twenty-three percent of non-medicated patients recovered after one month; 67 percent in six months; and 85% within a year. Posternak, “The naturalistic course of unipolar major depression in the absence of somatic therapy,” J Nervous and Mental Disease 194 (2006): 324-49. III. Bipolar Disorder A. Antidepressants create iatrogenic pathway to bipolar disorder In a review of 87,290 depressed patients, those treated with antidepressants converted to bipolar at rate of 7.7% per year, which was three times greater than for those not exposed to the drugs. Martin, “Age effects on antidepressant-induced manic conversion.” Arch Pediatrics & Adolescent Medicine 158 (2004): 773-80. B. In pre-drug era, manic-depressive illness was episodic with favorable long-term outcomes 1) Nearly 70% of manic-depressive patients hospitalized between 1935 and 1944 had good 30-year outcomes, which meant they married, lived in their own homes, and worked. Tsuang, “Long-term outcome of major psychoses,” Arch Gen Psychiatry 36 (1979):1295-1301. 2) Review of literature by Winokur, Manic Depressive Illness (St. Louis: The C.V. Mosby Company, 1969):21 C. Psychiatrists see increase in recurrence rates in bipolar patients with introduction of antidepressants Goodwin, Manic Depressive Illness (New York: Oxford University press, 1990): 647. Zis, “Major affective disorder as a recurrent illness,” Arch Gen Psychiatry 36 (1979):835-39. Koukopoulos, “Rapid cyclers, temperament, and antidepressants,” Comp Psychiatry 24 (1983):249-58. D. Increase in recurrence following lithium withdrawal Time to recurrence is seven times shorter than normal following lithium withdrawal. Baldessarini, “Discontinuing lithium maintenance treatment in bipolar disorders,” Bipolar Disorders 1 (1999):17-24. E. Chronicity in drug-treated patients today. 1) NIMH study: 146 bipolar patients followed for 12 years: they were depressed 32 percent of time, manic or hypomanic 9 percent, and suffering from mixed symptoms six percent of time. Judd, “The long-term natural history of the weekly symptomatic status of bipolar I disorder.” Arch Gen Psychiatry 59 (2002):530-37. 2) NIMH study: Bipolar II patients depressed 50% of time. Judd, “A prospective investigation of the natural history of the longterm weekly symptomatic status of bipolar II disorder,” Arch Gen Psychiatry 60 (2003): 261-69. 3) Two-thirds of 258 bipolar patients followed for one year had four or more episodes. Post, “Morbidity in 258 bipolar outpatients followed for 1 year with daily prospective ratings on the NIMH life chart method,” J Clin Psychiatry 64 (2003): 680-90. 4) 33 percent of bipolar I patients and 22 percent of bipolar II patients are rapid cyclers, and both groups symptomatic nearly half of time. Joffe, “A prospective, longitudinal study of percentage of time spent ill in patients with bipolar I or bipolar II disorders.” Bipolar Disorders 6 (2004):62-66. E. Deterioration in Functional Outcomes 1) Admission of deterioration of bipolar outcomes. Zarate, “Functional impairment and cognition in bipolar disorder.” Psychiatric Quarterly 71 (2000):309-29. 2) Admission of deterioration of outcomes. Huxley, “Disability and its treatment in bipolar disorder patients,” Bipolar Disorders 9 (2007):183-96. 3) Only 28% of bipolar patients have a good occupational outcome at end of five years. Gitlin, “Relapse and impairment in bipolar disorder,” AJP 152 (1995):1635-40. 4) Only 24% functionally recovered at end of one year. Keck, “12-month outcome of patients with bipolar disorder following hospitalization for a manic or a mixed episode,” AJP 155 (1998):64-52. 5) In study of 2,839 bipolar patients, two-thirds are unemployed. Kupfer, “Demographic and clinical characteristics of individuals in a bipolar case registry.” J Clin Psychiatry 63 (2002):129-25. F. Cognitive Decline 1) See Zarate and Huxley, ibid. 2) Bipolar patients today almost as cognitively and socially impaired as schizophrenia patients. Dickerson, “Outpatients with schizophrenia and bipolar I disorder,” Psychiatry Research 102 (2001):21-7. G. Medicated bipolar and medicated schizophrenia outcomes converge Data is from Harrow’s 15-year study ibid; but see Anatomy of an Epidemic, p. 195, for composite graphic of outcomes data for bipolar and schizophrenia patients, which shows that bipolar patients on medications fared worse than schizophrenia patients off medications long-term. IV. Psychiatric Medications and Children A. Long-term results in NIMH’s MTA study of ADHD 1) At end of three years, medication use a marker of deterioration. Jensen, “3-year follow-up of the NIMH MTA study,” J Amer Academy of Child & Adolescent Psychiatry 46 (2007):989-1002. 2) At end of six years, medication use associated with worse hyperactivity-impulsivity and ODD symptoms. Molina, “MTA at 8 years,” J Amer Academy of Child & Adolescent Psychiatry 48 (2009):484-500. B. Antidepressants in pediatric populations. 1) Tricyclics are ineffective even over the short term. Fisher, From Placebo to Panacea (New York: John Wiley & Sons, 1997):309. 2) Pediatric drug trials of SSRIs were biased by design, and results were not accurately reported in scientific journals. Editorial, “Depressing Research,” Lancet 363 (2004):1335. 3) 12 of 15 pediatric trials of SSRIs failed. T. Laughren, memorandum, “Background comments for Feb. 2, 2004 meeting of psychopharmacological drugs advisory committee,” Jan. 4, 2004. Accessed at fda.gov. 4) Prozac approval for pediatric populations based on grossly biased trial design. Leo, “The SSRI Trials in Children,” Ethical Human Psychology and Psychiatry 8 (2006):29-41. 5) British researchers conclude that SSRIs are not recommended for children and youth. Editorial, “Depressing research,” Lancet 363 (2004):1335. Jureidini, “Efficacy and safety of antidepressants for children and adolescents,” Brit Med Journal (2004):87983. C. Iatrogenic pathways to bipolar 1) 62 percent of juvenile bipolar patients treated with stimulant or antidepressant prior to becoming bipolar. Cicero, “Antidepressant exposure in bipolar children,” Psychiatry 66 (2003):317-22. 2) 83% of 195 juvenile bipolar patients had been diagnosed with other psychiatric illness first, and 66% had been to an antidepressant. Papolos. “Antidepressant-induced adverse effects in juvenile-onset bipolar disorders,” paper presented at the Fifth International Conference on Bipolar Disorders, June 12-14, 2003, Pittsburgh. 3) 84% of juvenile bipolar patients at NYC clinic previously exposed to psychiatric drugs; only 10% showed signs of bipolar before that drug exposure. Faedda, “Pediatric bipolar disorder,” Bipolar Disorders 6 (2004):305-13. D. Poor outcomes in medicated juvenile bipolar patients 1. They exhibit symptoms to severely ill, treatment-resistant adults. Geller, “Child and adolescent bipolar disorder,” J Amer Academy of Child & Adolescent Psychiatry 36 (1997):1168-76. 2. 87% of 195 juvenile bipolar patients suffer from ultra, ultra rapid cycling. Papolos, ibid. 3. 66% of juvenile bipolar patients are ultra, ultra rapid cyclers, and another 19% rapid cyclers. Faedda, “Treatment-emergent mania in pediatric bipolar disorder,” J Affective Disorders (82):149-58. 4. Juvenile bipolar patients symptomatic 60% of time; shift polarity 16 times a year. Birmaher, “Course and outcome of bipolar spectrum disorder in children and adolescents,” Development and Psychopathology 18 (2006):1023-35.