Mental health payment - The Office of London CCGs
advertisement

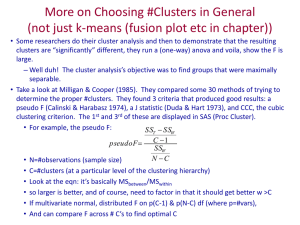
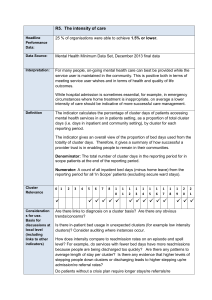
Mental Health Payment Martin Campbell Head of Pricing Overview What’s the rationale for a new payment approach for mental health services How far have we got in implementing a new payment approach for working age adults and older people What do we need to do to bring in new approaches for other MH services 2 The challenge Investment patterns by commissioners do not necessarily reflect need although allocations now do Weighted Expenditure on Mental Health Services 2011 Source: Department of Health 3 Mental Health Payment system needs to support delivery of improved mental health Enhanced personalisation and choice Reduction of variation in mental health services Value for money Quality Indicators Mental Health payment Improved, comparable data Parity of esteem Service Organisation and SLM Recovery and policy objectives Mental Health Payment by Results The model at its simplest Currency Model Activity (intervention) Cluster Algorithm Mental Health Clustering Tool Care Transition Protocols Quality Indicator 1 £ Quality Indicator 2 Quality Indicator 3 Quality Indicator 4 21 Clusters Resource utilisation (Tariff) Quality Indicators 1 2 3 Mental Health Payment by Results What’s been achieved nationally? Care clusters made available for use – February 2010 Costing data collected on a cluster basis – September 2011 All service users allocated to care clusters – December 2011 Mental health currencies mandated – April 2012 Quality measures available for use – April 2013 Cluster pricing methodology – April 2014 HSCIC quality and outcomes reports – July 2014 6 What’s the data showing • 81% of in-scope service users now assigned to a cluster, more than 95% in the top ten providers • 70% of initial cluster allocations meet the “red-rules” set out in the clustering booklet • 72% of service users being re-clustered within the suggested maximum review periods 7 What’s been achieved at the local level? • 2014 HFMA survey - 41 out of 59 trusts responded • 95% in regular dialogue with commissioners in relation to the payment mechanism • 68% have block contracts in place with a shadow tariff for 2014/15 • 95% had used the methodology for calculating local prices as set out in the National tariff document • 57% envisaged movement towards national prices by 2019/20 • 72% use active caseload monitoring to ensure that reported activity is accurate • 66% reasonably confident that in scope patients were clustered correctly as initial assessment, rising to 73% on re-clustering following review • 61% using a PROM short WEMWBS being the most popular • 78% use HoNOS as the clinical rated outcome measure (CROM) 8 Development of other services CAMHS • Pilots collecting data on resource usage using CYP IAPT dataset • Some initial thoughts on clusters but will be reviewed when data collection ends summer 2014 • Currencies available by 2015 Forensic services • Second year of piloting proposed currencies • Currencies available for use from late 2014 Learning Disabilities • Data collection to test potential approach • Engagement with service users, provides and commissioners during 2014 Psychological medicine • Tool kit being prepared as part of supporting guidance for 2015-16 Aim is to have alignment and support integration and transitions between services Mental Health Payment by Results