fourth presentation - Global Health 2035
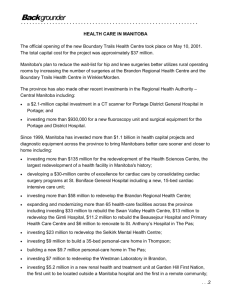
advertisement

Progressive Pathways to Universal Health Coverage David B Evans, Director Health Systems Governance & Financing Background 1. Grand Convergence: once in a lifetime opportunity 2. It will cost money – in low-income countries, increases in external financial will be necessary unless exceptional growth 3. Nevertheless, virtually all countries could raise or spend more on health if they wished - Sanjay Gupta IMF gave options for raising and spending wisely 4. What to do with the money? Commission on Investing in Health, London, December 2013 2| The Objective: Universal Health Coverage All people have access to needed services Without the risk of financial ruin linked to paying for care Universal Health Coverage: coverage with needed health services (of good quality); coverage with financial risk protection for all Commission on Investing in Health, London, December 2013 3| Financial Risk Protection 1. Requires: Prepayment and pooling of resources - compulsory Minimizing user fees and charges – zero for the poor and vulnerable (possibly "negative fees") Good quality services are available 2. The combination of financial risk protection with the availability of good quality services – instrumental to increasing health and economic wellbeing, but also valued for its own sake Commission on Investing in Health, London, December 2013 4| Resource Scarcity and Progressive Universalism Commission on Investing in Health, London, December 2013 5| Progressive Universalism: Features 1. The poor and vulnerable should be covered from the start – do not start with insurance for the formal sector and civil servants with the intention of bringing in the poor and informal sector later 2. Start by covering interventions against infectious diseases, targeting RNMCH, expanding to NCDs rapidly – the most highly cost-effective interventions 3. Limited if any payments at the point of service – poor and vulnerable exempted if fees are charged 4. Expand health services over time as rapidly as possible – prevention, promotion, treatment, rehabilitation, palliation Commission on Investing in Health, London, December 2013 6| Country Choices: Practicality and Politics 1. Begin by targeting poor and vulnerable versus universal from the start – practical questions: how easy to identify, restrict 2. Ways of ensuring poor can afford: zero user fees/copayments vs. exemptions (or cash transfers) – efficiency question 3. What to call compulsory prepaid contributions: taxes, charges or compulsory insurance? Sometimes people more willing to contribute to a tax called insurance than pay increases in overall taxation used to fund health 4. How many pools? Less fragmentation better 5. How to purchase services from pooled funds: fee for service inefficient, what role for results based payments? Commission on Investing in Health, London, December 2013 7| What Does Not Work 1. Voluntary insurance cannot get to UHC – at best, a supplement to compulsory pooling 2. Catastrophic insurance – e.g. insurance for unpredictable high cost items such as inpatient care - cannot get to UHC Commission on Investing in Health, London, December 2013 8| 9.0 Total Health Expenditure as % GDP: Selected Low Income Countries 8.0 7.0 Low income 6.0 Bein Cambodia 5.0 CAF Chad Eritrea 4.0 Guinea Haiti Myanmar 3.0 Nepal 2.0 1.0 0.0 2001 2002 2003 2004 2005 2006 Commission on Investing in Health, London, December 2013 9| 2007 2008 2009 2010 Thank you Commission on Investing in Health, London, December 2013 10 |