Lesson 3 Secondary Assessment - Bsa
advertisement

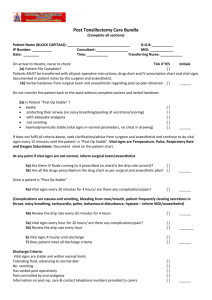
Lesson 3: Secondary Assessment Emergency Reference Guide p. 20-22 Objectives • State the importance of taking a personal history from victim & know how to do it • Demonstrate taking a personal history • Demonstrate a hands on physical exam • Demonstrate how to take vital signs • Demonstrate how to document information gathered Getting the Whole Picture • After primary assessment comes a hands on secondary assessment • Goal is to find EVERY problem • Consider environment when removing clothing during checks • Single person does exam, second person records results – why? • SAMPLE history taken at this time Getting the Whole Picture (cont’d.) • If patient can talk, take SAMPLE first If patient can’t talk, check with other members, use medical forms for info (i.e. allergies, medications, etc.) • • • • Document signs & symptoms Look for signs of injury Listen to victims words & responses Feel body parts Taking a SAMPLE History • S = Signs & symptoms: Ask what hurts? What pain do they have, nausea, lightheadedness? • A = Allergies: do they have any? Did they contact anything they are allergic to? • M = Medications: on any, last time taken? • P = Pertinent medical history: anything like this happened before? Existing conditions? Taking a SAMPLE History (cont’d.) • L = Last intake & output: Last time ate or drank? Last time urinated or defecated? • E = Events: What led up to this injury (Mechanism Of Injury)? Skill Practice • Break into pairs, one victim, one care giver • Scenario: • “While clearing some downed limbs from the trail, a person is apparently stung by a bee.” • Practice taking, and recording SAMPLE Why Documentation is Important? • Responder’s ability to remember details is reduced due to stress/confusion • Specific info helps rescue personnel know what they are facing • Retention for legal/medical reasons • Using a form helps you remember everything you need to look for/ask about Documentation (cont’d.) • SOAP: • S = subjective info (complaints) • O = Objective info (i.e. physical exam, vital signs, SAMPLE • A = Assess patient & situation, what do you think is wrong? • P = Plan, what care do you give & how? Stay or evacuate? Performing Hands On Physical Exam • Using MOI or SAMPLE record circumstances & estimate injuries • Do not make assumptions about MOI • Systematically check from head to toe • Ask where it hurts • Check all body parts, don’t cause unneeded pain Performing Hand On Physical Exam (cont’d.) • Examples of Signs & Symptoms: – Pale sweaty skin – Nervousness – Unnatural position of limbs – Patient guarding an area or unable to move body part • Looks for “DOTS” DOTS • DOTS stands for: • D = Deformities, depressions, indentations and discoloration • O = Open injuries, penetrating wounds, cuts, scrapes • T = Tenderness • S = Swelling Performing Hands On Physical Exam • Check Circulation, Sensation, Motion – Ask about pain first, then touch • Note medical ID bracelets, necklaces • Check pulse away from injury & away from heart (i.e. on hand or foot) • Check for circulation in hands & feet • Pinch & check for capillary refill (nail bed) • If head/neck/back injury possible, ask patient to not move, help restrain from moving Head to Toe Assessment Head to Toe Assessment(cont’d) Physical Exam Practice Session • Form into groups of 3: – One victim – 2 rescuers • Perform SAMPLE • Head to toe check Taking Vital Signs • Vital signs are a measure of the processes needed for life • Changes in time indicate patient condition changing • Take & record vital signs regularly • Basic Set: – – – – Level of Responsiveness Breathing Rate Pulse Skin Color, Temp, Moisture (SCTM) Level of Responsiveness • AVPU: – Alertness • • • • A + Ox4: knows who, where, when, what A + Ox3: knows who, where, when A + Ox2: knows who, where A + Ox1: knows who – V = Responds to verbal stimuli – P = Responds to pain – U = Unresponsive Respiratory Rate/Heart Rate • Respiratory: Number breaths/min., note rhythm and quality: – Normal 12-20 for adults – Place hand on chest to measure – Note any unusual sounds • Heart Rate (pulse): Measure at wrist, brachial artery, or neck – Use 2 fingers (no thumb) – Count for 30 seconds – Note rhythm, quality (strength) Skin Color, Temp, Moisture • Note any differences from normal: – Skin Color should be pink (non-pigmented areas) – Temperature should be warm – Moisture: skin should be dry Practice Session • Form into groups of 3 – One victim – One takes vital Signs – One records Re-Checking Resources • After patient assessment: – Observe changing conditions in environment – Getting unsafe for patient or you? – Getting difficult to get help? – What resources do you have, how can you use them? – Do you need to move the patient? Questions??? What else could you add to your First Aid Kit?