only
advertisement
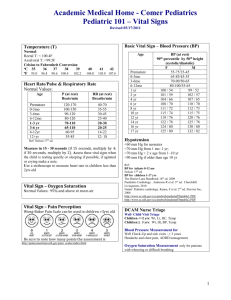
Lesson 8 Secondary Assessment Secondary Assessment (1 of 3) • Completes the full patient assessment • Goals: – Identification and treatment of previously unrecognized life-threatening injuries – Identification and treatment of non-life-threatening injuries Secondary Assessment (2 of 3) • Secondary assessment is completed only when time and situation permits – Critical patients • Focus remains on primary assessment until all lifethreatening conditions are identified and managed • May need to postpone secondary assessment and return to primary assessment based on changes in the patient’s condition Secondary Assessment (3 of 3) • Never delay transporting a critical patient in order to complete a secondary assessment © Kevin Norris/ShutterStock, Inc. Components • • • • • • • • Vital signs History Physical examination Treatment Decision-making Transportation Receiving facility Communication Vital Signs (1 of 6) • First part of the secondary assessment – Reassessment of vital functions • Multiple components – Pulse, ventilatory rate, blood pressure, skin parameters – All components in combination give an overall picture © Jones & Bartlett Learning. Photographed by Darren Stahlman. Vital Signs (2 of 6) • First set of vital sign measurements are used as a baseline for that patient • Repeat (at least) every time the patient’s condition changes • Repeat vital signs should be compared to previous set(s) – Trending Vital Signs (3 of 6) • Pulse – Location – Strength – Rate – Rhythm © Jones & Bartlett Learning. Photographed by Darren Stahlman. Vital Signs (4 of 6) • Respirations – Ventilatory rate – Depth/expansion – Effort • Use of accessory muscles • Mouth breathing versus nose breathing – Breath sounds and location © Jones & Bartlett Learning. Courtesy of MIEMSS. Vital Signs (5 of 6) • Blood pressure – Systolic and diastolic measurements • Automated • Manual – Auscultation – Palpation © WizData, Inc./ShutterStock, Inc. Vital Signs (6 of 6) • Skin parameters – Color – Temperature – Moisture – Capillary refill • May or may not provide accurate information • Age of patient • Underlying medical conditions – The environment may affect findings History • Verbal history from patient, family members, bystanders – Clues from on-scene observation • S-A-M-P-L-E © Robert Byron/Dreamstime.com Physical Examination • Physical examination directed by scene assessment, primary assessment, history, MOI/kinematics, and patient complaints • Detailed versus focused examination – Detailed involves all areas of the body • Head-to-toe – Focused involves limited areas of the body • Systematic approach Monitors • Utilized as indicated by patient condition – Pulse oximetry – Cardiac monitor – End tidal CO2 (ETCO2)/capnography – Continuous blood pressure Courtesy Masimo Treatment Options (1 of 4) • Immobilization – Selective spinal immobilization – Extremities • Open wounds – Control of external hemorrhage – Prevent infection/contamination Treatment Options (2 of 4) • Re-evaluate need for: – Supplemental oxygen – IV access and fluid administration – Prevention of body heat loss Treatment Options (3 of 4) • Comfort Measures: – Pain control – Positioning – Padding Treatment Options (4 of 4) • Comfort Measures: – Emotional support (reassurance) • Patient • Family members © Jones and Bartlett Learning. Courtesy of MIEMSS. Decision-Making Time • Considerations: – Situation – Assessment – History – MOI/kinematics – Patient severity – Treatment available – Additional resources required • Transport decision Transportation (1 of 2) • The receiving facility decision – Level of care needed – Notification • The decision to transport as soon as possible is based on: – Situation – Severity of injuries Transportation (2 of 2) • Other considerations: – Prioritizing multiple patients – Distance to receiving facility – Weather conditions – Traffic conditions Communication (1 of 2) • Receiving facility – Timely notification • Allows receiving facility to prepare – Brief description of scene – Number of patients arriving – Current patient status – Treatment provided – ETA Communication (2 of 2) • Hand-off report – Verbal and written Summary (1 of 3) • If the patient is critical, secondary assessment might not be completed • Continue to monitor and reassess the components of the primary assessment • Repeat vital signs are compared to previous sets for changes (trending) Summary (2 of 3) • The extent of the secondary assessment is based on the patient’s complaints and condition as time permits • Transport decisions are based on the patient’s assessment and needs Summary (3 of 3) • Communicate findings with receiving facility – Prior to arrival – Upon arrival • Verbal • Written Questions?