vomiting prescription
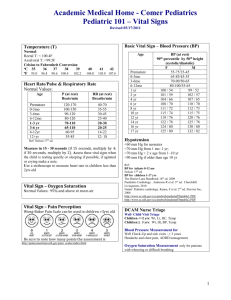
advertisement
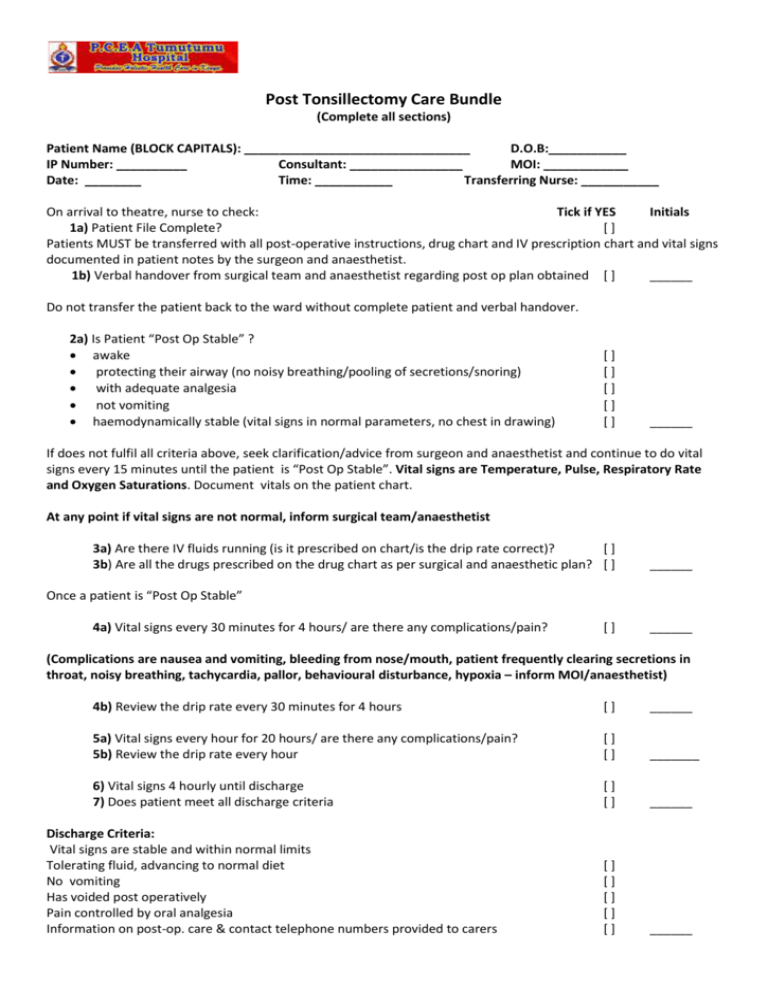
Post Tonsillectomy Care Bundle (Complete all sections) Patient Name (BLOCK CAPITALS): ________________________________ D.O.B:___________ IP Number: __________ Consultant: ________________ MOI: ____________ Date: ________ Time: ___________ Transferring Nurse: ___________ On arrival to theatre, nurse to check: Tick if YES Initials 1a) Patient File Complete? [] Patients MUST be transferred with all post-operative instructions, drug chart and IV prescription chart and vital signs documented in patient notes by the surgeon and anaesthetist. 1b) Verbal handover from surgical team and anaesthetist regarding post op plan obtained [ ] ______ Do not transfer the patient back to the ward without complete patient and verbal handover. 2a) Is Patient “Post Op Stable” ? awake protecting their airway (no noisy breathing/pooling of secretions/snoring) with adequate analgesia not vomiting haemodynamically stable (vital signs in normal parameters, no chest in drawing) [] [] [] [] [] ______ If does not fulfil all criteria above, seek clarification/advice from surgeon and anaesthetist and continue to do vital signs every 15 minutes until the patient is “Post Op Stable”. Vital signs are Temperature, Pulse, Respiratory Rate and Oxygen Saturations. Document vitals on the patient chart. At any point if vital signs are not normal, inform surgical team/anaesthetist 3a) Are there IV fluids running (is it prescribed on chart/is the drip rate correct)? [] 3b) Are all the drugs prescribed on the drug chart as per surgical and anaesthetic plan? [ ] ______ Once a patient is “Post Op Stable” 4a) Vital signs every 30 minutes for 4 hours/ are there any complications/pain? [] ______ (Complications are nausea and vomiting, bleeding from nose/mouth, patient frequently clearing secretions in throat, noisy breathing, tachycardia, pallor, behavioural disturbance, hypoxia – inform MOI/anaesthetist) 4b) Review the drip rate every 30 minutes for 4 hours [] ______ 5a) Vital signs every hour for 20 hours/ are there any complications/pain? 5b) Review the drip rate every hour [] [] _______ 6) Vital signs 4 hourly until discharge 7) Does patient meet all discharge criteria [] [] ______ [] [] [] [] [] ______ Discharge Criteria: Vital signs are stable and within normal limits Tolerating fluid, advancing to normal diet No vomiting Has voided post operatively Pain controlled by oral analgesia Information on post-op. care & contact telephone numbers provided to carers