Paste Bandages
advertisement

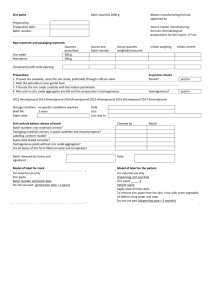
Paste Bandages Indications Management of leg ulcers. Some are also indicated for use in the management of chronic eczema / dermatitis. Seen used to protect legs from incontinence. They have mild astringent and antiseptic properties. Contraindications: ◦ Occasional sensitivity / allergy to ingredients Types Zinc paste bandage (Viscopaste PB7, Steripaste) Zinc paste and ichthammol (Ichthopaste) Zinc paste and calamine Zinc paste and coal tar bandage Zinc paste impregnated stocking (Zipzoc) How could they work? Array of properties that can enhance the healing of wounds. Zinc ions stay within the wound bed for an extended period of time, ensuring a constant tissue zinc level. Zinc: ◦ increases the degradation of collagen in necrotic tissues, ◦ promotes epitheliazation and ◦ increases the expression of insulin-like growth factor, essential for the production of granulation ◦ also required for collagen and protein synthesis, cellular growth and replication, reduction in free radical activity and inhibition of bacterial growth. Bandaging also promotes venous return Application Methods Various suggested: ◦ ◦ ◦ ◦ ◦ cutting and overlap pleating applying the bandages in strips (can be layered) cutting to form stirrups applying in a series of loose folds rather than a continuous spiral No controlled trials support one best method of application A 2007 paper recommend that zinc paste bandages should be applied loosely and lightly with a pleat at each turn to accommodate for oedema and the primary bandage covered by compression bandaging or retention bandages as tolerated by the patient. Instruction leaflets for viscopaste and icthopaste both state that it can be applied in a spiral or with a pleat at the front on every turn. Evidence Meyer et al (2002) used zinc paste bandages as a primary dressing in their study of 112 patients. They could not rule if zinc oxide paste affected the rate of healing achieved. Strömberg and Agren (1984) performed a randomized trial where patients were treated with either a gauze compress medicated with zinc oxide or with an identical compress without zinc oxide. Patients treated with a zinc oxide compress responded significantly better (83% success rate) compared with the placebo group (42% success rate). Limitations of the study included a small sample size, mixed aetiology and outcome measurement at only 8 weeks. Bradley et al (1999) reported significant increase in ulcers healed with zinc oxide impregnated bandages at 58% compared with alginate at 35%. Lack of evidence concerning best practice bandaging technique. A Cochrane review (O’Meara et al 2010) on antibiotics and topical antiseptics for venous leg ulcers makes no mention of paste bandages in this context. Paste bandages are mentioned in a review on compression for venous leg ulcers (O’Meara et al 2009) but it states that the relative effects of 4 layer compression and paste bandage systems are unclear.