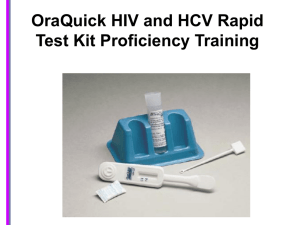
OraQuick ADVANCE Rapid HIV Test Training Presentation
advertisement

OraQuick ADVANCE How to Run the Test Overview Background Presentation Demo of the test Practice tests - You will practice running 2 tests – We will not be testing anyone in the room Proficiency Test - You will run 5 tests without assistance – Run, read, and document 5 tests – Read results of 10 test images – Pass / fail course, must get 100% to pass What Do You Know About Rapid HIV Tests? Intro to OraQuick ADVANCE Rapid Test One-step test Visual interpretation Uses blood or oral fluid Looks for HIV antibodies Results in 20 to 40 minutes In California…. Individuals who have been trained by CDPH/OA and are working in a OA-funded HIV testing site can run HIV/Hep C rapid tests OR Are working in an HIV testing site that meets these two criteria: – Utilizes HIV counseling staff who are trained by OA or its agents and – Has a quality assurance plan (QA) approved by the local health department in the jurisdiction where the site is located and has HIV testing staff who comply with specific QA requirements.* They must also be certified to perform finger sticks (or be occupationally exempt, like nurses) * QA requirements are specified in Section 1230 of Title 17 of the California Code of Regulations Package Insert Contains instructions CLIA requires following the manufacturer’s instructions to the letter!! Subject Information Brochure Contains information about the test that is relevant to the client Package Insert says, “All subjects must receive the Subject Information Brochure” Check in with your site to see how this is handled Test Accuracy We’re going to talk about how well the test works You do not need to memorize the details - only need to know test is very accurate There are two components of test accuracy: Sensitivity Specificity Specificity When a test finds something, it should be the right thing Tests ability to detect a true negative Specificity Test True Neg Tested Neg False Pos Specificity EIA 1 467 442 25 94.7% EIA RR 467 463 4 99.1% OraQuick I 464 463 1 99.8% OraQuick RR 464 463 1 99.8% More specific than standard HIV test (EIA) – – – – Test is very accurate (but not perfect) Screening test is designed to be very sensitive. Due to this design, we sacrifice a little specificity. Must confirm preliminary positives (SOC, false+) • Draw blood and send to lab (conventional oral test is back up) Sensitivity The ability of a test to find what it’s looking for and not miss anything. Test’s ability to detect a true positive Sensitivity Test True Pos Tested Pos False Neg Sensitivity EIA 1 340 340 0 100% EIA RR 340 340 0 100% OraQuick 1 340 340 0 100% OraQuick RR 340 340 0 100% Rapid test is at least as sensitive as conventional HIV test (EIA) – RR = repeatedly reactive Combining Specificity and Sensitivity An ideal test would find the right thing (specificity) and not miss anything (sensitivity) Think of a Tuna net…. A net that gets all the tuna and none of the dolphins Because Test is Highly Sensitive… We do not need to confirm negatives We do, however, always need to confirm reactive/ preliminary positives 2 Different Tests Stat-Pak 1st Test _ Negative, please come back and see us in 6 months + ++ OraQuick Test Reactive, 2nd Test _ Lab Testing Both tests were reactive your next step is to see a doctor and we can help you with that With Clients… Emphasize that the test is extremely accurate De-emphasize statistics and percentages For example “This test is highly accurate” Quality Assurance Requirements QA are practices and procedures which ensure that every client receives an accurate test result QA reduces human error as much as possible Components of Quality Assurance • Personal and logistical characteristics • External controls • Lab space • Universal precautions Must Have… Steady hand Good eye sight Organizational skills Adequate lighting Full/bright light, task light Do not use a flashlight External Controls Fluids made from human plasma Biohazards – wear gloves! Controls can be negative, positive for HIV-1, or positive for HIV-2 Expire 56 days after opening External Controls are Used for: Training, we will use them today Determining if test is working properly Determining if lighting is adequate Determining if the test reader has sufficient eye site HIV-1 vs HIV-2 Two different strains Both are transmitted the same way HIV-2 is less infectious HIV-2 progresses more slowly HIV-2 found in West Africa and is rarely found elsewhere When to Run External Controls • New operator • New setting or conditions changed significantly • New test kit lot or shipment • Out of range testing area or storage area temperature • Two invalid results in a row • Every 40 tests or once a month (whichever comes first) Why? Temperature Control Perform test, 59-99 degrees If testing temperature is out of required temperature range stop testing If out of temp range, run controls before proceeding (ask State) Store test: 35-80 degrees Lab Space A space for undisturbed test processing Your site is a lab Separate from counseling area No smoking, eating or drinking Universal Precautions The universal practice of avoiding contact with patients' bodily fluids (blood), by means of the wearing of nonporous articles such as medical gloves Gloves Wear them when handling blood or blood products, and…. TODAY – whenever you touch the control fluid vials!!!! How often do you change them? How do you remove them? Sharps: Handling & Disposal Sharps are Medical instruments that are used to puncture the skin (syringes, lancets, needles) Dispose of sharps immediately, in a hard red plastic bio bin! Do NOT dispose of sharps in a red bio hazard bag Biohazard Bags: Handling & Disposal Bandages, used cotton and gauze, and gloves with body fluids on them are bio hazardous waste By law, if fluid cannot be squeezed out of the cotton, gauze, etc., the waste item can be disposed of in regular trash. For Today’s Training Place loops and used Place gloves and all test kits in the sharps other trash in the container brown paper bag Paperwork Needed Expanded Checklist Short Checklist (Competency Assessment Test list) Rapid testing log or lab slip Lab stickers HIV Testing Form Always use blue or black ink only! Introduction to the Test • Control line • Test line • Flat pad Trainers Demonstrate Trainer Reads Other Trainer preforms test Participants follow along (Expanded Checklist) Participants’ First Practice No food or drink Listen to detailed steps: Only do what we tell you to do Do all steps in order If you finish a step quickly, wait for the next step Reading Time Results in 20-40 minutes If a reactive result appears before 20 minutes have passed, the result may still not be read until at least 20 minutes have passed OraQuick Test Results • Two lines: “C” - Control line “T” - Test line • Negative result • Reactive result • Invalid result What causes invalids? Human error (e.g., no specimen) Unknown Manufacturer error If you ever have an unusual result, do not deliver it What does it mean if a client has an invalid test result? What does the darkness of the lines mean? NOTHING A B D C C C C C T T T T G F E H C C C C T T T T Participants’ Second Practice Pair up – One person run a test at their own pace, using the short checklist – Partner observe them and help only as needed (e.g., if you see any steps that were missed, say something) – Switch Use the checklist!!!! Internal Control – The “C” Line The control line is the “C” line Internal control tells us: Specimen was adequately applied Proper hydration Migration of reagents past the “T” zone. Internal & external controls are standard lab practice – not a sign of test kit unreliability Test Line – The “T” Line The “T” line is the “test line”. It works with the external control fluids to: tell us if the result is reactive or non-reactive. tell us if the reader can see lines. tell us if there is proper lighting. tell us if the reader’s eyesight is adequate to run the test. Controls Work Together If the internal control & the external controls both tell us the test kit is working, why do we need both? Because they tell us something different! “C” line tells us test kit is working properly “T” line tells us the test kit can detect HIV antibodies when they’re present Results of Practice Test Did you get the correct result? Any questions? The control fluid that we use provides a “challenge sample” Light control line verifies lighting is OK Verifies test kit detecting small amount of antibody Darkness of line NOT related to viral load, disease progression, or anything else about the client If a Client Asks to See the Test Kit, What Would You Do? Say “No” – Why? Could compromise confidentiality Only trained personnel may read the test Test is disposed of in biohazard bag as soon as it’s read Think about the picture with the pink background – if you have a light line would you be able to see it on this test? How Do You Correct a Written Mistake? A single crossed-out line, corrected entry written clearly above, include date and initials of the individual making the change. At no time should an original entry be obliterated or otherwise made illegible by a change on the record. 7:22pm T.K. 12/15/2011 End time: 7:12pm Any questions? Proficiency tests coming next…. OraQuick HIV Test Proficiency: Words of Caution Follow the checklist!!!! This is not a test of memorization Run five tests using five different vials Put your name on the top of your paper(s) Take your time, double & triple checking your work If you make a mistake on your paperwork and you catch it, you can fix it. and I catch it, you will have to come back another day