Chapter 6-Bone Formation
advertisement

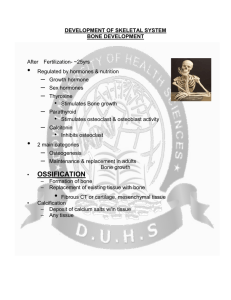
Ch 6.4-Bone Formation When does bone formation occur? 1) During embryonic development 2) During infancy, childhood, and adolescence 3) Remodeling of bone 4) Repair of fractures Embryonic Bone Formation Two Patterns Intramembranous Ossification Forms directly within mesenchyme (Simple; few # of bones) Endochondral Ossification Forms within hyaline cartilage that develops from mesenchyme (Complex; most bones) Intramembranous Ossification STEP 1: Development of ossification center Blood capillary Ossification center Mesenchymal cells cluster Mesenchymal cell Form osteogenic cells → osteoblasts Osteoblast Secrete organic bone EC matrix Collagen fiber Intramembranous Ossification STEP 2: Calcification Osteocyte Osteocytes become fully developed Extend cytoplasmic projections Osteoblast Newly calcified bone EC matrix Surrounding osteoblasts deposit calcium and mineral salts Intramembranous Ossification STEP 3: Formation of trabeculae Mesenchyme condenses Blood vessel Ossification centers fuse to form trabeculae Spongy bone trabeculae Osteoblast Blood vessels grow in between Intramembranous Ossification STEP 4: Development of the periosteum Periosteum Mesenchyme condenses Spongy bone tissue Forms periosteum Compact bone replaces surface Compact bone tissue layer of spongy bone Endochondral Ossification STEP 1: Development of cartilage model Perichondrium Proximal epiphysis Hyaline cartilage Mesenchymal cells form shape of future bone Diaphysis Develop into chondroblasts Distal epiphysis Secrete cartilage EC Matrix Endochondral Ossification STEP 2: Growth of cartilage model Perichondrium Chondroblasts deeply buried in cartilage Uncalcified extracellular matrix Calcified extracellular matrix Now called chondrocytes Mid-region chondrocytes grow; Surrounding EC matrix calcifies Chrondrocytes begin to die, leaving small cavities Endochondral Ossification STEP 3: Development of primary ossification center Nutrient artery penetrates perichondrium Periosteum Osteogenic cells become osteoblasts Nutrient artery Primary ossification center Spongy bone Blood vessels induce growth of primary ossification center Osteoblasts turn cartilage into bone Endochondral Ossification STEP 4: Development of the medullary cavity Uncalcified extracellular matrix Calcified extracellular matrix Periosteum Medullary cavity Osteoclasts breakdown newly formed spongy bone Endochondral Ossification STEP 5: Development of secondary ossification centers Secondary ossification center Epiphyseal artery and vein Uncalcified extracellular matrix Blood vessels enter epiphyses Secondary ossification centers develop Proceeds outward Nutrient artery and vein Endochondral Ossification STEP 6: Formation of articular cartilage and epiphyseal plate Articular cartilage Spongy bone Epiphyseal plate Outer cartilage becomes articular cartilage Cartilage remains between diaphysis and epiphysis Forms epiphyseal plate Epiphyseal Plate - Helps bones grow in length - Contains a group of young chondrocytes - New chondrocytes form on epiphyseal side - Old chondrocytes form bone on diaphyseal side Epiphyseal Line Bone Remodeling - The ongoing replacement of old bone tissue by new bone tissue Bone Resorption Destruction of EC matrix Bone Deposition Formation of EC matrix Fractures Partial or Complete Closed or Open Fractures Phagocytes remove dead bone tissue Chondroblasts form fibrocartilage bridge Fibrocartilage turned to spongy bone Bone Remodeling Factors Affecting Bone Growth - Mineral supply - Calcium - Phosphorus - Magnesium - Vitamins A, C, and D - Hormones - Human growth hormone (hGH): Before puberty - Estrogens and Androgens: At puberty - Weight-bearing exercise Some stimulus disrupts homeostasis by Calcium Homeostasis Decreasing Blood calcium (Ca2+) level Receptors - Bones store 99% of body’s calcium Parathyroid gland cells detect lowered Ca2+ level Input - Acts as a “buffer” for blood calcium levels Control center PTH gene “turned on” - Ca released into blood by osteoclasts and removed from blood by osteoblasts Output - Negative feedback loop - Receptor: Parathyroid gland - Control Center: Parathyroid Hormone (PTH) gene - Effector: Osteoclasts and Kidneys Increased production of cyclic AMP Increased release of PTH Effectors Osteoclasts Kidneys retain increase bone Ca2+ in blood, resorption excrete phosphate in urine, and produce calcitriol Increase in blood Ca2+ level Return to homeostasis when response brings blood Ca2+ level back to normal Osteoporosis Risk Factors - Over 50 yrs old Female Low estrogen/testosterone Excess alcohol consumption Smoking Inactivity Soft drinks