Power Point CH 6
advertisement
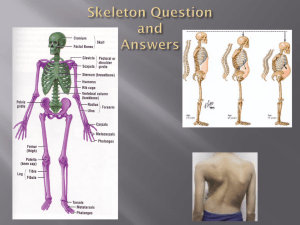
Chapter 6 *Lecture Outline *See separate FlexArt PowerPoint slides for all figures and tables pre-inserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Chapter 6 Outline • • • • • • • Cartilage Bone Classification and Anatomy of Bones Ossification Homeostasis and Bone Growth Bone Markings Aging of the Skeletal System Intro to the Skeletal System • An organ system with tissues that grow and change throughout life – bones – cartilages – ligaments – other supportive connective tissues Cartilage • Semi-rigid connective tissue – not as strong as bone, more flexible/resilient – mature cartilage is avascular • Cells – chondroblasts: produce matrix – chondrocytes: surrounded by matrix • live in small spaces called lacunae Distribution of Cartilage Figure 6.1 Functions of Cartilage • • • Support soft tissues – airways in respiratory system – auricle of ear Articulations – smooth surfaces where bones meet Precursor model for bone growth – fetal long bones Growth of Cartilage • Two patterns – Interstitial growth • from inside of the cartilage – Appositional growth • along outside edge of the cartilage Interstitial Growth • • Mitosis of chondrocytes in lacunae – forms two chondrocytes per lacuna – each synthesize and secrete new matrix – new matrix separates the cells Result: – larger piece of cartilage – newest cartilage inside Figure 6.2 Appositional Growth • Mitosis of stem cells in perichondrium – – – – • adds chondroblasts to periphery produce matrix, become chondrocytes forming new lacunae adding to existing matrix Results: – – larger piece of cartilage newest cartilage on outside edges Figure 6.2 Bones • Living organs containing all four tissue types – primarily connective tissue – extracellular matrix is sturdy and rigid – strengthened by calcification: minerals deposited in the matrix (main store and source of Ca++ and PO4---) Function of Bones • • • • • Support Protection Movement Hemopoiesis Storage Classifying Bones • Long bones – • Short bones – • nearly equal length and width Flat bones – • greater length than width thin surfaces Irregular bones – other/complex shapes Classification of Bones According to Shape Figure 6.3 Long Bone Anatomy • Diaphysis – • Epiphyses – – – • elongated, usually cylindrical, shaft knobby, enlarged regions at ends strengthen joints attachment site for tendons/ligaments Metaphyses – – between diaphysis and epiphysis contains epiphysial (growth) plate Long Bone Anatomy Figure 6.4 Long Bone Anatomy • Articular cartilage – – • thin layer of hyaline cartilage on epiphyses reduces friction between articulating bones Medullary/marrow cavity – – cylindrical space in diaphysis usually contains yellow bone marrow Long Bone Anatomy Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Articular cartilage Spongy bone (contains red bone marrow) Proximal epiphysis Epiphyseal line Metaphysis Compact bone Medullary cavity (contains yellow bone marrow in adult) Endosteum Periosteum Perforating fibers Diaphysis Nutrient artery through nutrient foramen Metaphysis Epiphyseal line Figure 6.4 Distal epiphysis Articular cartilage (c) Bone Coverings • Periosteum – – – – • dense irregular connective tissue covers external surfaces of bones • does not cover articular cartilages acts as anchor for blood vessels and nerves anchored by perforating fibers embedded in the bone matrix Endosteum – covers most internal surfaces of bones Bone Coverings Figure 6.5 Bone Cells • • • • Osteoprogenitors: mesenchymal stem cells, found in endosteum and periosteum, mitotically produce more stem cells or osteoblasts Osteoblasts: form bone matrix Osteocytes: reside in lacunae; maintain matrix and communicate with osteoblasts to cause further deposit of bone matrix Osteoclasts: large, multinucleate cells that dissolve bone, releasing Ca++ Bone Cells Figure 6.6 Bone Matrix • 1/3 organic components – cells – collagen fibers – ground substance • 2/3 inorganic components – bone salt crystals: hydroxyapatite • calcium phosphate and hydroxide –Ca10(PO4)6(OH)2 Comparing Bone Tissues • • Compact bone – solid and relatively dense – external surfaces of long and flat bones Spongy bone – open lattice of narrow plates: trabeculae – internal surface of bones Flat Bones • Have compact and spongy (diploë) bone Figure 6.7 Compact Bone Organization • The basic structural and functional unit of mature compact bone is the osteon – also known as a Haversian system – cylindrical structures – parallel to the shaft of the bone Osteon Components • Canals – – – • central: carries blood vessels and nerves perforating: perpendicular connections to central canal with blood vessels and nerves canaliculi: between lacunae allowing metabolic interactions between osteocytes Lamellae – – – concentric: rings of bone around central canal circumferential: along endosteum and periosteum interstitial: “leftover” pieces of old osteons Osteon or Haversion System Figure 6.8 Ossification • The formation and development of bone – – • also known as osteogenesis begins by 8th week of embryonic development and continues into adulthood Two general patterns: – Intramembranous – Endochondral Patterns of Ossification • Intramembranous ossification – – • develops from mesenchyme produces flat bones of the skull, some facial bones, the mandible, and central portion of clavicle Endochondral ossification – – begins with a hyaline cartilage model produces the majority of bones in the body Stages of Intramembranous Ossification 1. Ossification centers form within thickened regions of mesenchyme Figure 6.10 Stages of Intramembranous Ossification 2. Osteoid (precursor to solid bone matrix) undergoes calcification Figure 6.10 Stages of Intramembranous Ossification 3. Woven (primary) bone and surrounding periosteum form Figure 6.10 Stages of Intramembranous Ossification 4. Lamellar (secondary) bone replaces woven bone as compact and spongy bone form Figure 6.10 Stages of Endochondral Ossification 1. Fetal hyaline cartilage model develops Figure 6.11 Stages of Endochondral Ossification 2. Cartilage calcifies and a periosteal bone collar forms around diaphysis Figure 6.11 Stages of Endochondral Ossification 3. Primary ossification center forms in the diaphysis Figure 6.11 Stages of Endochondral Ossification 4. Secondary ossification centers form in the epiphysis Figure 6.11 Stages of Endochondral Ossification 5. Bone replaces cartilage, except the articular cartilage and epiphyseal plates Figure 6.11 Stages of Endochondral Ossification 6. Epiphyseal plates ossify and form epiphyseal lines Figure 6.11 The Epiphyseal Plate • A layer of hyaline cartilage at the boundary of the epiphysis and diaphysis – site of interstitial growth (bone lengthening) – consists of five distinct microscopic zones Figure 6.12 Zones of Epiphyseal Plate 1. Zone of resting cartilage–farthest from medullary cavity, nearest epiphysis, small chondrocytes in hyaline cartilage Figure 6.12 Zones of Epiphyseal Plate 2. Zone of proliferating cartilage–larger chondrocytes undergoing rapid mitotic cell division, aligned like stacks of coins Figure 6.12 Zones of Epiphyseal Plate 3. Zone of hypertrophic cartilage– chondrocytes not dividing, become enlarged Figure 6.12 Zones of Epiphyseal Plate 4. Zone of calcified cartilage–deposited minerals kill the chondrocytes and make matrix opaque Figure 6.12 Zones of Epiphyseal Plate 5. Zone of ossification–walls between lacunae break, forming channels that become invaded with capillaries and osteoprogenitor cells Figure 6.12 Bone Growth • Bone is constantly being remodeled – • more dense in early adulthood, less in older adults Two types of growth: – – Interstitial: in length Appositional: in diameter Appositional Growth Figure 6.13 Blood and Nerve Supply Three major types of arteries and veins: • Nutrient: supply the diaphysis; nerves usually accompany these into the shaft of the bone • Metaphyseal: supply area between the diaphysis and tepiphysis • Epiphyseal: supply cells in epiphyseal plate Arterial Supply to Bone Figure 6.14 Effects of Hormones and Vitamins on Bone Effects of Exercise on Bone • Mechanical stress (i.e., muscle contraction and gravity) stimulates increase in bone density by increased osteoblast activity • Athletes who engage in these types of activities, on average, have greater bone density Bone Fractures Figure 6.15 Bone Fracture Classification Bone Fracture Repair 1. A bone fracture hematoma (blood clot) occurs. 2. A fibrocartilaginous (soft) callus forms. 3. A bony (hard) callus replaces the soft callus. 4. The bone is remodeled. Bone Fracture Repair Figure 6.16 Anatomical Features of Bones Figure 6.17 Bone Aging • • During aging, bone changes in two ways: – Loses ability to produce organic matrix (mainly collagen) – loses Ca++ and other bone salts This can result in a condition called osteoporosis, decrease in bone density – can result in bone fractures Normal vs. Osteoporotic Bone