cardio pulmonary cerebral resuscitation (cpr)
advertisement

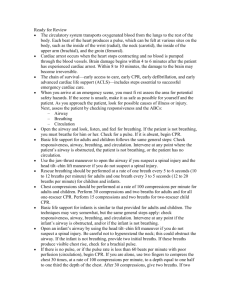
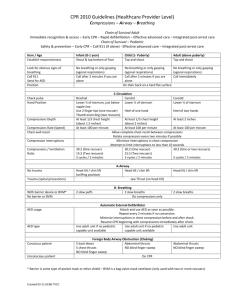
CARDIO PULMONARY CEREBRAL RESUSCITATION (CPR) (18 OCT 2010 GUIDELINES) (CAB) DR J MYBURG DEPT OF FAMILY MEDICINE UNIVERSITY OF THE FREE STATE INTRODUCTION • DEFINITION: CPR is an intervention that attempts to give a person with cardiac and/or respiratory arrest: 1) MECHANICAL CIRCULATION, 2) AN OPEN AIRWAY 3) ADEQUATE VENTILATION in order to restore some blood supply and oxygenation to the brain and other vital organs until such a time that the heart can be restarted. This procedure should take place with GREAT URGENCY because: • Permanent brain damage will occur after 3 – 4 minutes of hypoxia at normal temperature. • Possibility of successful resuscitation, decreases by 10% for every minute that passes after the onset of cardiac arrest. (After 10 minutes prognosis therefore is= +/- 0 at normal body temperature) ADULT CHAIN OF SURVIVAL CONSISTS OF 4 LINKS: 1) 2) 3) 4) Early recognition and call for help (improve prognosis) Early CPR (to buy time) Early defibrillation (to restart the hart) Good post resuscitation care (to restore quality of life) IN ADULTS VENTRICULAR FIBRILLATION IS USUALLY THE CAUSE – NEED DEFIBRILLATOR TO TREAT Exceptions: 1) Near-drowning 2) Cardiac arrest associated with trauma 3) Respiratory arrest is present (drug overdose, airway obstruction) PEDIATRIC CHAIN OF SURVIVAL CONSISTS OF 4 LINKS: 1) 2) 3) 4) Prevention Early CPR Early activation of EMS Early advanced cardio vascular care IN CHILDREN RESPIRATORY ARREST MOST COMMON CAUSE Exceptions: 1) Children known to be at high risk for cardiac arrest (congenital heart lesions) SEQUENCE OF CPR 1) HAZARDS: Assess whether the scene is safe. 2) HELLO: Check responsiveness. Gently shake shoulders and ask loudly: “Are you all right?” If responsive: Treat illnesses or injuries as necessary. REASSESS frequently. 3) HELP: Call for help, defibrillator/AED. Activate EMS Above known as 3 x Hes 4) CABD (Previous: ABCD) CABD • C = COMPRESSIONS OF THE CHEST • A = AIRWAY • B = BREATHING • D = DEFIBRILLATION (CIRCULATION) DIAGNOSIS of CARDIAC ARREST Types of arrest: 1) Ventricular fibrillation (80%) 2) Asystole (20%) 3) Pulse less electrical activity PEA (0,5%) Diagnosis: 1) Absent central pulses (take long to detect) 2) Unconscious patient with no breathing: Start compressions immediately. ( New approach) C: CHEST COMPRESSIONS (CIRCULATION) • FEEL FOR PULSE: (<10 seconds) ADULT: CAROTID PULSE CHILD: BRACHIAL PULSE IF PRESENT: CONTINUE WITH AIRWAY, BREATING AND RESCUE BREATHS: ADULT: 10/min CHILD: 12-20/min IF ABSENT: IMMEDIATELY START WITH 30 CLOSED CHEST COMPRESSIONS (+/-18 - 20 Seconds, rate 100/min) CIRCULATION CIRCULATION (method) • • • • • • • • • • • • • Kneel by the side of the victim Place the heel of one hand in the centre of the chest (2 fingers above xiphysternum, or line connecting the nipples) Place the heel of the other hand on top of the first hand. Lock fingers above the chest wall Position of arms (Elbows locked in extension) Position of rescuer (Vertically above patient) Depth of compression: 1/3 of thickness of chest (5-6cm in adult) Rate: 100-120/min Push hard, fast, ensure full chest recoil between compressions, minimize interruptions Do 30 COMPRESSIONS (18-20 seconds), THEN OPEN AIRWAY AND CHECK FOR BREATHING. Give 2 RESCUE BREATHS in absence of breathing CPR RATIOS: 30 compressions : 2 ventilations Perform 5 cycles / 2 minutes of CPR, then re evalute the patient. CIRCULATION Two-finger chest compression technique in infant (1 rescuer). Berg M D et al. Circulation 2010;122:S862-S875 Copyright © American Heart Association Two thumb-encircling hands chest compression in infant (2 rescuers). Berg M D et al. Circulation 2010;122:S862-S875 Copyright © American Heart Association A: AIRWAY • • • • • Assesses and open the airway. Open mouth – inspect for foreign objects, vomitus & secretions Remove any FOREIGN OBJECTS with FINGER SWEEP & suction. HEAD TILT, CHIN LIFT JAW THRUST with neck stabilization in case of ? neck injury. B: BREATHING • LOOK, LISTEN AND FEEL for adequate breathing (<10 seconds) • If in doubt, act if person is not breathing BREATHING • If there is adequate breathing, put patient in RECOVERY position • Get help from ambulance service • Continue to assess and monitor breathing. BREATHING • If there is no breathing, give 2 rescue breaths delivering each breath over 1 second • Making sure that the patient’s chest rises with each breath. • Allow 1 second for exhalation between breaths BREATHING (METHOD) • Open airway with head tilt, chin lift / jaw thrust • Pinch person’s nose, using index finger & thumb of hand on forehead • Allow mouth to open, but maintain chin lift • Take deep breath, place your lips around the person’s mouth, ensure a good seal • Blow steadily into person’s mouth, while watching for the chest to rise. Take about 1 second to make the chest rise as in normal breathing. This is an effective rescue breath. • Maintain head tilt / chin lift, take your mouth away from the person’s mouth and watch for the chest to fall back as air flows out. • Repeat above actions for a 2nd time. • The 2 breaths all together should not take more than 5 seconds. • Ambubag, Mask, Oropharyngeal airway can also be used instead. D: DEFIBRILLATION • IN CASE OF WHITNESSED COLLAPSE: CONNECT DEFIBRILLATOR / AED IMMEDIATELY IF AVAILABLE AND PROCEED WITH DEFIBRILLATION IF THE DIAGNOSIS IS VF OR VT • IF TIME FROM COLLAPSE > 5 MINUTES, FIRST DO 2 MINUTES (5 cycles) CPR, STARTING WITH CHEST COMPRESSIONS, BEFORE ANALYZING THE RHYTHM AND PERFORMING OTHER INTERVENTIONS • DEFIBRILLATION: SEE SEPARATE LECTURE. WHEN TO STOP OR WITHHOLD CPR • • • • • • • • Restoration of effective spontaneous circulation & ventilation Transfer of care to other medical personnel The rescuer is physically unable to continue resuscitation Recognition of reliable criteria for determination of death Presentation of a VALID no-CPR order to the rescuers Failure to restore circulation despite adequate CPR for >30 minutes The patient has a terminal condition which will not benefit from CPR Deterioration in an inpatients condition despite maximum therapy • GOOD SAMARITAN laws generally provide that persons who render aid at the scene of an emergency will not be liable for civil damages, if they act in good faith and not for any remuneration.