Ready for Review
advertisement

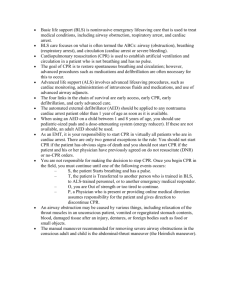
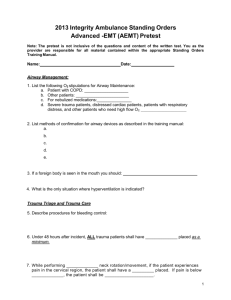
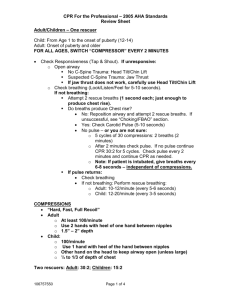
Ready for Review The circulatory system transports oxygenated blood from the lungs to the rest of the body. Each beat of the heart produces a pulse, which can be felt at various sites on the body, such as the inside of the wrist (radial), the neck (carotid), the inside of the upper arm (brachial), and the groin (femoral). Cardiac arrest occurs when the heart stops contracting and no blood is pumped through the blood vessels. Brain damage begins within 4 to 6 minutes after the patient has experienced cardiac arrest. Within 8 to 10 minutes, the damage to the brain may become irreversible. The chain of survival—early access to care, early CPR, early defibrillation, and early advanced cardiac life support (ACLS)—includes steps essential to successful emergency cardiac care. When you arrive at an emergency scene, you must fi rst assess the area for potential safety hazards. If the scene is unsafe, make it as safe as possible for yourself and the patient. As you approach the patient, look for possible causes of illness or injury. Next, assess the patient by checking responsiveness and the ABCs: – Airway – Breathing – Circulation Open the airway and look, listen, and feel for breathing. If the patient is not breathing, you must breathe for him or her. Check for a pulse. If it is absent, begin CPR. Basic life support for adults and children follows the same general steps: Check responsiveness, airway, breathing, and circulation. Intervene at any point where the patient’s airway is obstructed, the patient is not breathing, or the patient has no circulation. Use the jaw-thrust maneuver to open the airway if you suspect a spinal injury and the head tilt–chin lift maneuver if you do not suspect a spinal injury. Rescue breathing should be performed at a rate of one breath every 5 to 6 seconds (10 to 12 breaths per minute) for adults and one breath every 3 to 5 seconds (12 to 20 breaths per minute) for children and infants. Chest compressions should be performed at a rate of 100 compressions per minute for adults and children. Perform 30 compressions and two breaths for adults and for all one-rescuer CPR. Perform 15 compressions and two breaths for two-rescuer child CPR. Basic life support for infants is similar to that provided for adults and children. The techniques may vary somewhat, but the same general steps apply: check responsiveness, airway, breathing, and circulation. Intervene at any point if the infant’s airway is obstructed, and/or if the infant is not breathing. Open an infant’s airway by using the head tilt–chin lift maneuver if you do not suspect a spinal injury. Be careful not to hyperextend the neck; this could obstruct the airway. If the infant is not breathing, provide two initial breaths. If these breaths produce visible chest rise, check for a brachial pulse. If there is no pulse, or if the pulse rate is less than 60 beats per minute with poor perfusion (circulation), begin CPR. If you are alone, use two fingers to compress the chest 30 times, at a rate of 100 compressions per minute, to a depth equal to one half to one third the depth of the chest. After 30 compressions, give two breaths. If two rescuers are present, use the two-thumb technique with the hands encircling the chest and provide 15 compressions to two breaths. The single most important cardiac arrest survival f actor is early defibrillation. The indications for using an automated external defibrillator (AED) are that the patient is unresponsive, not breathing, and pulseless. If the patient’s cardiac arrest was witnessed by you, begin CPR and apply the AED as soon as possible. However, if the cardiac arrest was not witnessed by you, perform five cycles (about 2 minutes) of CPR before applying the AED. Once turned on and attached to the patient’s bare chest, the AED will analyze the heart rhythm and advise whether a shock is indicated. If a shock is advised, ensure that no one is touching the patient, deliver the shock, and immediately perform CPR for 2 minutes before reanalyzing the patient’s rhythm. If no shock is advised, perform CPR for 2 minutes and then reanalyze the patient’s rhythm. Continue CPR and rhythm analysis until advanced life support personnel arrive.