Skin and Body Membranes
advertisement
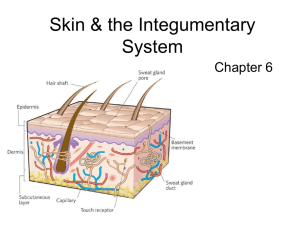
Body Membranes Cover surfaces, line body cavities, and form protective (and often lubricating) sheets around organs Two main categories: Epithelial membranes – includes cutaneous, mucous, and serous membranes Connective tissue membranes – synovial membranes Epithelial Membranes Although they contain an epithelial sheet, it is always combined with an underlying layer of connective tissue actually “simple organs” Cutaneous membrane (skin) Mucous membrane (mucosa) Serous membrane (serosa) Cutaneous membrane The skin Superficial epidermis composed of a keratinizing stratified squamous epithelium Underlying dermis is mostly dense (fibrous) connective tissue Exposed to air dry membrane Mucous Membrane Mucosa Composed of epithelium resting on a loose connective tissue membrane called a lamina propria Lines all body cavities that open to exterior, such as those of the hollow organs of the respiratory, digestive, urinary, and reproductive tracts Most contain stratified squamous epithelium or simple columnar epithelium Adapted for absorption or secretion A “wet” membrane Serous Membrane Serosa Composed of a layer of simple squamous epithelium resting on a thin layer of areolar connective tissue Line body cavities that are closed to exterior except for dorsal body cavity and joint cavities Membranes occur in pairs parietal layer lines a specific portion of the wall of the ventral body cavity and folds in on itself to form the visceral layer, which covers the outside of the organs in that cavity Layers are separated by serous fluid, which is secreted by both membranes allows organs to slide easily without friction Serous Membrane Names depend on location in the body Peritoneum – serosa lining abdominal cavity and covering its organs Pleura – serosa surrounding the lungs Pericardium – serosa surrounding the heart Synovial Membrane Composed of soft areolar connective tissue; contain no epithelial cells at all Line the fibrous capsules surrounding joints, providing a smooth surface and secreting a lubricating fluid Line small sacs of connective tissue called bursae and the tube-like tendon sheaths cushion organs moving against each other during muscle activity Skin Also called integument, which means “covering” Insulates, cushions, keeps water and organs inside body, protects against UV radiation and bacteria Contains many capillaries and sweat glands that play important role in regulating heat loss Synthesizes vitamin D Contains receptors that detect touch, pressure, temperature, and pain Epidermis Outer layer of skin Made up of stratified squamous epithelium that is capable of keratinizing, or hardening Avascular Epidermis Five layers (strata) from inside to outside: stratum basale, spinosum, granulosum, lucidum, and corneum Most cells are keratinocytes, which produce keratin, the fibrous protein that makes the epidermis a tough protective layer Stratum basale lies closest to dermis and contains the only epidermal cells that receive adequate nourishment via diffusion and produce new cells Daughter cells are pushed upward and away Epidermis Stratum lucidum is only found where the skin is hairless and thick, such as the palms of hands or soles of feet Stratum corneum is outer most layer, 20-30 layers thick ¾ of all epidermal thickness Melanin = pigment that ranges from yellow to brown to black, produced by melanocytes in stratum basale Exposure to sunlight stimulates melanin production tanning Freckles and moles form where melanin is concentrated in one spot Dermis Directly below epidermis Made up of dense connective tissue Usually firmly connected to epidermis, but sometimes they separate could result in blister Dermis Leather goods = dermis of animals Two major regions – papillary and reticular Papillary = upper dermal region, uneven with fingerlike projections called dermal papillae Dermal papillae contain capillary loops, pain receptors, and touch receptors form fingerprints and footprints Reticular = deepest skin layer, contains blood vessels, sweat and oil glands, phagocytes, and deep pressure receptors Dermis Collagen and elastic fibers are found throughout dermis Collagen attracts and binds to water Elastic fibers give young skin elasticity As we age, number of these fibers decreases wrinkles and saggy skin http://www.youtube.com/watch?v=f46SpiboAew Hypodermis Aka “subcutaneous tissue” Essentially adipose tissue Helps anchor skin to underlying organs Serves as shock absorber and insulation Skin Color Three pigments contribute to skin color: The amount and kind (yellow, reddish brown, or black) of melanin in the epidermis The amount of carotene (orange-yellow pigment found in orange, yellow, or leafy green veggies) deposited in the stratum corneum and subcutaneous tissue The amount of oxygen bound to hemoglobin in the dermal blood vessels Lots of melanin = darker skin Oxygen-rich hemoglobin is easier to see in people with lighter skin Skin Color Indications Cyanosis = skin appears blue when hemoglobin is poorly oxygenated Skin Color Indications Erythema = Reddened skin, may indicate embarrassment, fever, hypertension, inflammation, or allergy Skin Color Indications Pallor (blanching) = pale skin, may indicate emotional stress, anemia, low blood pressure, or impaired blood flow Skin Color Indications Jaundice = yellow skin, usually signifies liver disorder in which bile pigments are absorbed into blood and deposited in body tissues Skin Color Indications Bruising = black-and-blue marks, reveal sites where blood has escaped from circulation and clotted in tissue spaces hematomas. Excessive bruising can be a sign of vitamin D deficiency or hemophilia, among other things Skin appendages Cutaneous glands = exocrine glands (release secretions to skin surface), fall into two groups Sebacious (oil) glands = found all over skin except for palms of hands and soles of feet, ducts usually empty into a hair follicle, produce sebum, a mix of oily substances and fragmented cells. Sebum keeps the skin lubricated, moist, and soft and helps kill bacteria. Blocked sebacious glands result in acne (whiteheads and blackheads) Sweat glands = also called sudoriferous glands, two main kinds: eccrine and apocrine Sweat glands Eccrine glands = more numerous, found all over body, produce sweat, a clear secretion that is primarily water plus salts, vitamin C, metabolic wastes, and lactic acid and is usually acidic. Sweat reaches skin through ducts called pores (not to be confused with outlets for hair follicles) Apocrine glands = generally confined to axillary and genital areas of body, usually larger in size with ducts that empty into hair follicles. The secretion contains fatty acids and proteins in addition to substances found in eccrine gland secretions. The secretion is odorless on its own, but when bacteria use its nutrients for growth, it takes on a “musky” odor. These glands are activated during puberty. Hair and Hair Follicles Serve a few minor protective functions, such as guarding the head against bumps, shielding the eyes (eyelashes and eyebrows), and keeping foreign particles out of respiratory tract (nose hairs) Previously provided insulation Hair is produced by a hair follicle The part of the hair that is enclosed in the follicle is the root The part projecting from the surface is the shaft Hair and Hair Follicles Hair is formed by the division of the well-nourished stratum basale epithelial cells in the growth zone, or hair bulb matrix, at the inferior end of the follicle. As the daughter cells are pushed farther away from the growing region, they become keratinized and die, thus making the bulk of the hair shaft dead material (almost entirely protein) Each hair consists of a central core called the medulla, which is surrounded by a bulky cortex layer, which is enclosed by a cuticle layer. The cuticle is a single layer of cells that overlap one another like shingles on a roof. Hair and Hair Follicles Hair pigment is made by melanocytes in hair bulb Hair follicles are actually compound structures. The inner epidermal sheath is composed of epithelial tissue and forms the hair. The outer dermal sheath is actually dermal connective tissue, which supplies blood vessels to the epidermal portion and reinforces it. Arrector pili = small bands of smooth muscle cells that connect each side of the hair follicle to the dermal tissue. When they contract, the hair is pulled upright “goose bumps” Nails Scalelike modification of the epidermis that corresponds to the hoof or claw of other animals Each nail has a free edge, a body (visible attached portion), and a root (embedded in skin) Borders of nail are overlapped by skin folds, called nail folds Cuticle = thick proximal nail fold Stratum basale extends beneath nail as nail bed Nail matrix = thickened nail bed responsible for nail growth nail cells become heavily keratinized and die Nails are transparent and nearly colorless, but look pink due to rich blood supply in underlying dermis Lunula = white crescent shape at end of nail Infections and Allergies Athlete’s foot = itchy, red, peeling condition of the skin between the toes, resulting from fungal infection Boils and carbuncles = inflammation of hair follicles and sebaceous glands, common on the dorsal neck. Carbuncles are composite boils typically caused by bacterial infection. Infections and Allergies Cold sores = small fluid-filled blisters that itch and sting, caused by a herpes simplex infection. The virus remains in a cutaneous nerve until it is activated by emotional upset, fever, or UV radiation. Usually found around lips or oral mucosa of mouth. Contact dermatitis = itching, redness, and swelling of skin, progressing to blistering, caused by exposure to chemicals that provoke an allergic reaction. Infections and Allergies Impetigo = pink, water-filled, raised lesions, usually around mouth and nose, that develop a yellow crust and eventually rupture. Caused by a highly contagious staph infection, common in elementary school students. Psoriasis = chronic condition characterized by reddened epidermal lesions covered with dry, silvery scales, potentially disfiguring, cause unknown. Burns Burn = tissue damage and cell death caused by intense heat, electricity, UV radiation, or certain chemicals Damage to skin can affect nearly every body system, altering metabolism, immune system, and cardiovascular system. Body loses supply of fluids, dehydration, electrolyte imbalance Rule of nines = helps determine how much fluid is lost, divides body into 11 areas, each accounting for 9% of total body surface area, plus additional area surrounding genitals representing 1%. Burns Burned skin is sterile for ~24 hours After that, pathogens such as bacteria and fungi invade areas where skin has been destroyed and multiply in the nutrient-rich environment Patient’s immune system becomes depressed within one to two days after severe burn injury Burns Classified by severity 1st degree burns = only epidermis is damaged, area becomes red and swollen, usually heals in 2-3 days 2nd degree burns = damage to epidermis and upper layer f dermis, skin is red and painful, blisters appear, regeneration of epithelium can occur, no scars if care is taken to prevent infection 3rd degree burns = destroy entire thickness of skin, burned area appears blanched (grey-white) or blackened, nerve endings destroyed burned area is not painful, regeneration is not possible, skin grafts required Burns Considered critical if: 1. Over 25% of the body has second-degree burns 2. Over 10% of the body has third-degree burns 3. There are third-degree burns of the face, hands, or feet Facial burns are dangerous because of the possibility of burned respiratory passageways, which can swell and cause suffocation Severe burns at joints can result in scar tissue that limits joint mobility Skin Cancer Most skin tumors are benign and do not metastasize to other areas (ex. warts), but some are malignant http://video.about.com/dermatology/SkinCancer.htm Basal cell carcinoma = least malignant and most common skin cancer, cells of stratum basale proliferate and invade dermis and subcutaneous tissue, appear as shiny, dome shaped nodules which develop central ulcers with “pearly” beaded edges. Because it is so noticeable and slow-growing, metastasis rarely occurs. When removed surgically, there is a 99% chance for a full cure. Skin Cancer Squamous cell carcinoma = arises from cells in stratum spinosum, lesion appears as a scaly, reddened papule that gradually forms a shallow ulcer with a firm, raised border, usually found on scalp, ears, hands, and lower lip. Grows rapidly and metastasizes to adjacent lymph nodes if not removed, believed to be sun-induced. If caught early and removed, chance of complete cure is good. Skin Cancer Malignant melanoma = cancer of melanocytes, accounts for only 5% of skin cancers, often deadly, can begin anywhere there is pigment, most appear spontaneously, but some develop from moles. Usually appears as spreading brown to black patch that metastasizes rapidly to surrounding lymph and blood vessels, ~50% survival rate, early detection helps, ABCD rule: Asymmetry – two sides of pigmented mole do not match Border irregularity – borders are not smooth, but show indentations Color – pigmented spot contains areas of different colors Diameter – spot is larger than 6 mm in diameter (pencil eraser) Developmental Aspects of Skin and Body Membranes Lanugo = downy type of hair that covers infants during 5th and 6th months of fetal development, usually shed by birth Vernix caseosa = white, cheesy-looking substance, produced by sebaceous glands, protects baby’s skin while it is floating in water-filled sac inside mother Milia = small white spots on baby caused by accumulations in the sebaceous glands, normally disappear by third week after birth Developmental Aspects of Skin and Body Membranes In adolescence, the skin and hair become more oily as sebaceous glands are activated acne. This usually subsides by adulthood Skin begins to visibly change around the 30s as it is constantly exposed to abrasion, chemicals, wind, sun, pollutants, bacteria, etc. causing pores to clog and skin to be irritated pimples, scales, dermatitis Developmental Aspects of Skin and Body Membranes Aging subcutaneous tissue decreases, skin becomes drier, collagen and elastic fibers decrease, skin gets thinner Hair loses its luster, by age 50 the number of hair follicles has dropped by 1/3, resulting in hair thinning or baldness Male pattern baldness – hair follicles have become colorless and tiny Greying hair = usually genetically controlled, amount of melanin deposited decreases or becomes entirely absent, can be caused by stressful events, protein-deficient diets, chemotherapy, etc. http://www.youtube.com/watch?v=lLgagxUKWaA&fe ature=related http://www.youtube.com/watch?v=NRAYccnyfkY&fea ture=related http://www.iteachbio.com/Anatomy-Physiology/anatphys.html