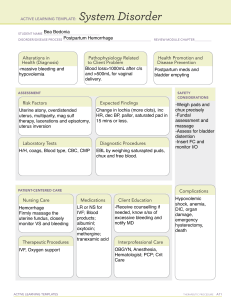
PostPartum haemorrhage By Dr. Oliver Chukwuemeka Onwube (mbbs,fwacs,afmcog,fics) Postpartum haemorrhage Outline 1. Introdcution 2. Definition 3. Causes 4. Managemen 5. The WHO PPH bundle 6. Conclusion Introduction Postpartum haemorrhage remains a leading cause of maternal mortality. In fact it contributes to 25-30% of maternal mortality The wife of the Shah Jahan of India, the Empress Mumtaz had 14 children and died after her last chidbirth of a postpartum haemorrhage in 1630. So great was the Shah Jahan’s love for his wife that he built the world’s most beautiful tomb in her memory- the TAJ MAHAL Today maternal mortality from postpartum haemorrhage is still ever present with us. We must find answers to this turn in the flesh Definition Postpartum haemorrhage is defined as loss of greater than 500mls of blood after a vaginal delivery or loss of greater than 1000mls of blood after a caesarean section…… WHO Or any bleeding after delivery leading to haemodynamic imbalance as evidenced by weakness, dizziness, tachycardia and hypotension. It is Primary postpartum haemorrhage if the bleeding occurs within 24hours of birth. Secondary postpartum haemorrhage is defined as any vaginal bleeding in excess of normal lochia occurring greater than 24 hours but less than 6weeks postpartum Aetiology Causes (The 4Ts) A. Atony (60-70%) 1.Uterine Overdistension(Multiparity, polyhydramnios,Macrosomia) 2. Uterine relaxants(Nifedipine,magnesium,betamimetics,indomethacin, Nitric oxide donors) 3. Rapid or prolonged labour 4. Oxytoxics to induce labour 5. Chorioamnionitis 6. Halogenated Anaesthesia 7. Fibroid Uterus B. Tissue(5-10%) 1.Retained placenta 2. Morbidly adherent placenta eg, placenta acreta/percreta/increta, succenturiate lobe 3. Prior Uterine Surgery eg, myomectomy, caesarean Section 4. Obstructed labour C. Trauma (20%) 1. Vulvovaginal injury 2. Episiotomy 3. Cervical tears D. Thrombin (1-2%) 1. HELLP syndrome 2. DIC (Eclampsia, IUFD, Septicemia, placenta Abruption, Amniotic fluid embolism) 3.Hereditary eg, Von Willebrand’s disease 4. Anticoagulant therapy This is not the time for time wasting history taking The key strategies in management are as follows: 1. Call for help 2. Resuscitation (A B C) 3. Secure a double i.v. access with a wide bore canula 4. Commence fluid replacement with crystallooids eg, n/s, Ringers lactate, Hartman solution or colloids eg, haemacele and Isoplasma 5. Urgently take blood for grouping and crossmatching 6. Insert an indwelling urethral catheter to commence monitoring of urine output. Management of PPH.. 6. A CVP can be inserted in centres with the capability to monitor and manage fluid replacement After these, the cause of the bleeding can be quickly assessed by examining the uterus for atony and a gentle and gradual genital tract examination for injuries or retained products Medical 1. Forty i.u. of oxytocin added to 500mls of N/s at 20dpm 2. Insert 1000micrograms of misoprostol rectally 3. IM ergot 0.5ml stat 4. IM/ I.V. Carbetocin 100mcg start 5. I.V. Tranexamic acid 1000mg start Management of PPH Surgical 1. Rubbing up uterine contraction 2. Repair of episiotomy (Episiorrhaphy) 3. Cervical tear repairs 4. Vaginal tear repairs 5. Uterine Tamponade(bimanual uterine compression, Bakri balloon, uterine packing, foley’s catheter, condom catheter, Sengstaken Blakemore tube) 6. B-lynch procedure 7. Hayman suture 8. Cho suture 9. Stepwise devascularization 10. Internal iliac artery ligation 11. Uterine artery embolization/ligation 12. Esike’s Procedure 13. Peripartum hysterectomy The WHO PPH care bundle Care bundles are described by the Institute for Healthcare Improvement (IHI) as a structured way of improving processes of care and patient outcomes (1). Care bundles typically consist of a set of evidence-based practices (generally three to five) that, when performed consistently, can improve outcomes. While the IHI definition does not mention a specific time frame to implement these practices, many care bundles are designed in such a manner that component interventions are meant to be initiated concurrently, collectively or otherwise rapidly. A care bundle approach might help improve PPH- related outcomes through one or more of the following pathways. • Help optimize the coverage of multiple effective interventions simultaneously. • Place an emphasis on collective, rather than sequential, use of interventions. This can shorten the time to initiating an intervention (such as a uterotonic or antifibrinolytic drug), which can optimize their effects. Reducing delays in treatment could prevent ensuing complications. • The concurrent use of multiple effective interventions may confer other synergistic effects. The use of a care bundle for PPH treatment is conceptually linked to the accurate diagnosis of PPH. The bundle includes early detection and trigger criteria (based on the measurement of blood loss using a calibrated blood loss collection drape, and assessment of clinical signs) and a first response PPH treatment package (uterine massage, oxytocic agents and uterotonics, tranexamic acid, intravenous fluid infusion and examination.