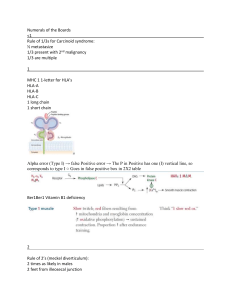
Lyteratura: Egzamin? Immunologia? Immune system exists in order to defend our organism from infections, mostly... but it also performs other functions. It’s devided into three parts. First, physical barriers like skin, tissue, mucus, the outer layer. Second, innate immunity: Universal immunity against pathogenes, Adaptive immunity: Needs to interact with outside world to function, adapts to certain pathogenes. We are our surrroundings and our evironment is us, both metaphysically, physically, and mentally. We can’t have any tough barriers (But ego). Skin is the toughest of our barriers, of multiple layers. Three big parts of skin. Epidermis Dermis Subcatanous Tissue Epidermis is covered by keratinocytes, on the bottom, on the basemet membrane. Only one layer of keratinocytes can divide (around the 3rd layer). Those that can’t fit in the layer, when they divide, will be differentiated into skin cells -> SKeratinocytes die and move to the outside of the skin and then they are peeled out. Maturing of Keratinocytes are connected with big amount production of Keratins, or Cytokeratins Ck (specific proteins abundant in mature Keratinocytes - Kc) In Dermis We have glands, Fat Glands that produce and secrete fatty acids onto the epidermis surface. Sebaceous gland (fat gland) → fat acids outside secretion (Epidermis surface); Sweat glands → thermoregulation; sweat also contains anti bac that will help to protect skin (Cationic proteins Lysosynes) Other glands are sweat glands, Sweat glands are supp osed not only to termoregulate. Sweat contains lyzozyme, like saliva. Subcotaneus tissue is vasculated and nervated. Immune cells are present within this layer. Cytokeratins are insoluble in water. Mature of Kc kills them; moving to the outside and eventually peel out Skin is occupied bu our own bacterial flora and so other bacteria can’t survive. Low pH comes from fat acids produced by Sebaceous gland; ~5.0 or above, commensal bacteria (normal skin flora), they create an environment that prevent other pathogens Ck protects non polar (against water) peeling out skin processes pH Liquid soap > Bar soap. Skin works for as long as it’s intact. Epithelia covers all other surfaces that aren’t covered by skin. Example respiratory tract, digestive... It’s easy for pathogenes to cross the epithelia. (not so great barrier) Food (w probable pathogens) → stomach (acid) → duodeno (alkaline) here some pathogens that eventually survived can goes to intestine (that makes peeling out – defense against pathogens), and full of comensal bacteria that take this ecological niche and occupies Long time antibiotic problems to use → disturb comensal bacteria in the tracts Respiratory tract: not so well protected; barrier: special epithelia (cilia) that moves expelling / pushing to the outside Sneezing and coughing as mechanisms of resp tract; Epithelial cells products mucous that moves alongside cilia; Some body fluids (antibacteria proteins, Lysosyme cationic protein that directly kills bacterias; Saliva and tears → Lactoferrin*) *Lactf was discovered in milk (binds Iron ions; this quenching cause the lack of Iron available for pathogens, bacteriostatic action). Innate Immunity Human immune system is dispersed among many places in organims. Lymph Nodes Spleen - Graveyard Bone Marrow Appendix doesn’t work in humans. Thymus Peyer’s Patches Lymphatic Vesicle Tonsils and adenoids -> Migdałki. Two central organs Immune system → Bone Marrow; Thymus Peripheral organs → different lymphonodes; spleen (some cell maturing and recycling of immune system cells) Tonsil* where parents check it Soluble compounds are dissolved in plasma; Immune system is not only in blood but migrate to other tissues; Other cells are penetrating tissues. White blood cells aren’t limited to blood. Bone marrow -> Blood production. Hematopoietic stem cells. Stem cells SC divide in different way. Stem cell division will produce one stem cell and one progenitor cell. Cell division of all stem cells, not only Hematopoietic ones, is like that. What they will differentiate into, will depend on the activated genes that are a response to various signals which you see above. Stromal cells are responsible for secretion. Hematopoietic division of the Stem cells are regulated by stromal cells located in the Bone Marrow (covered by stromal cells from insed, that receive signals for the organisms, activate SC to divide, signal are secreted by stromal cells in which direction will differentiate); i.e. Myeloid SC or progenitor; Lymphoid SC Most of all of Innate immune system cells are descendent of Myeloid stem cells; later division give rises to Basophyle progenitor → Basophyle; Mast cells; Eosinophyles progenitor → Eosinophyles; Myeloid SC (precursor of erythrocytes and platelets) Don’t bother remembering the signals (Yet) but focus on the Myeloid Stem Cell and Lymphoid Stem cell and what they can differentiate into. Lymphoid SC → B / Lymphocytes; Natural Killers Phagocytes. Peripherial blood -> Monocyte If monocyte enters a tissue, it turns into a macrophage, but the phenotype of macrophage differs on the tissue that it enters. Slide above. Here my internet broke. Something something, phagocytosis. Ilya Ilych Mechnikov (Ukraine, 1845, France 1916) Nobel 1908 discovery of phagocytosis See also: Mechanisms for Phagolysosomes degradation -Oxygen dependent degradation -Oxygen independent degradation Phagocytosis can be generally divided into 7 steps (1) chemotaxis … Acidic conditions inside of the phagosome is a trigger for different enzymes that are inside of Lysosomes; Phago Lysosome → activate digestive enzymes; activates ROs and RNs, all activated ones helps digestion; transport of elements from cell → cytosol (indigestible particles) Phagocytes are covered with many receptors, screening for both pathogenes and other cells. It needs to recognise it’s surroundings. Here’s a list of groups of receptors. Bacteria recognision: CD14 recognises LPS, LPS is present only on bacterial cell wall surfaces. Those are responsible for most of the damn recognition. Jeal Hoffman - Fruit flues - 1996 -> Flies die too fast -> covered with ‘fur’ which was fungi -> Toll like receptor knocked out. Toll like receptors are present on different cells. Outsie parts can regognise a variety of patterns. External parts of TLRs are very diverse in their detection. The inside parts are, on the other hand very similar, because they all are supposed to produce the same response. TLRs are present both in Endosomes and on the plasma membranes. Oxygen dependant phagocytic degradation nad Oxygen independent Binding with TLR estimulate phagocytosis (PM receptros) and enhance the immune system defense (inner endosome receptors) Oxygen dependant depend on Radicals and enzymes like catalases and oxydases. Oxygen – independend: i.e. lysozimes (Lactoferrin) dissolves cell wall of gram positive bacteria; acid hydrolases – digest bacteria cell L.2 Immunology, pt 1 MHC complex aka HLA Nobel prizes: Baruj Benacerraf – IR genes (Argentina); Jean Dausset – HLA genes; George D. Snel – H 2 genes Novel discoveries was followed by: - the development of surgery practices – old times there was no anesthetics; - antiseptic (importance of sterilization during practices) With the development of surgery, transplants interventions were more successful; insights in why there was rejection by the transplanted patient? Mechanisms of rejection of transplants → Nobel prize’s group worked in this investigation inbred strains: reproduction of related partners (in animals you mate siblings only… after 20 generation or so, we can be sure that 99% of them animals will be homozygous; each allele carries same gene for any of them animals). Insights: Which genes must be identical in order to not occur rejection → H-2 genes G. D Snell MHC I Within these new identified genes groups, are MHC I and MHC II; peptide binding cleft (or antigen binding groove) FUNCTION: MHC I and II – peptide clefts, comes out within protein degradation Proteosome: ubiquitinated proteins goes to proteosome (20 min of the recorded lecture) Source of peptide that are loaded in MHC class one molecules; For example, viral infection 1st: Virus enter cell cycle and replicates within the cell contex 2nd: Viral and normal cell mRNA somewhere ended into proteosome and are cleaved into small fragment of peptide 3rd: Peptides enters ER, and inside are loaded into peptide-binding grooves (clefts) of MHC-I molecules 4th: As every protein in cell, MHC I molecules goes to Golgi to maturate 5th: After maturation, is load in exosomes vesicles, eventually merging with cell PM In this way, the MHC is presented to the surface of the cell. Inside of ER step - alpha chain of MHC complex is unstable as long as not attached with beta2 microglobulin - calnexin (chaperon) attach MHC – I alpha chain; - b 2 microglobulin is attached - calnexin is replaced by big complex of proteins (TAP channel) - all peptides that comes out of proteosome, travel through TAP channel - since MHC-I is directly attached to TAP, the peptides will bond within the peptide-binding grooves (clefts) - now the complex is very stable - moves to Golgi → exocytic vesicles → PM The composition of the peptide-binding grooves (clefts) can be distinct among MHC-I molecules, therefore not all peptides will be able to bind it MHC-II peptides comes from lysosomal degradation Lysosomal: Endocytosis or phagocytosis or autophagy (endosomes → lysosome); acidification takes place and activate enzymes MHC-II antigen presentation - loading of peptides in peptide-binding grooves (clefts) occurs in different places than MHC-I - ER step is similar - matures in Golgi without the peptides - goes to exocytic vesicles → binds to vesicle that contains chaperones (HLA – DM vesicles) - formed complex will bind then to lysosome - peptides after lysosomes will be loaded to peptide-binding grooves (clefts) - such a complex will be stable, detach from HLA-DM chaperon - then merge with PM Detailed mechanism below The presentation of peptides here are from other than the ones that comes from proteosome; - Inside of ER → one protein chain is translated (Invariant chain) - Invariant chain blocks the peptide-binding grooves - this complex goes to Golgi - Invariant chains partially are digested - few pieces still remains at peptide-binding grooves - then merges with chaperon and lysosomes - when HLA-DM binds, the peptide-binding grooves changes conformation into open one - making cleaved peptides leave out, and lysosomes peptides goes in - the complex MHC-II + peptides becomes stable, and can be presented outside of the cell MHC-I every nucleated cell have MHC-I molecules MHC-II are found only in antigen-presenting cells (APCs) like macrophage, dentritic cells, B cell, thymus epitellia cells The result of presentation of peptides are different: MHC-I - cytosolic proteins are degraded in the cytosol (like virus) binds to MHC-I; are presented to CD8 T lymphocytes → killing cell that was presented the peptide-binding MHC_II - macrophage or dendritic → load peptides from endocyti vesicles to MHC-II → present to CD4 helper T cell → generation of proteins that activates phagocytosis, natural killers etc - B-cells → bind to proteins/peptides that are being recognized by antibody → endocytosis → degradation of peptides → loading into MHC-II → activation of helper T cells (proteins that activate B cells that will produce immunoglobulins / antibodies) L.2 Immunology, pt 2 Dendritic cell Bridge between Innate vs Adaptive systems Higher phagocytose and pinocytose capacity (more than macrophages) Are present in intestine, air tract, every place where pathogen can enters the body; Once they become activated, they phagocyte and migrate to lymphonodes → interact with B and T cell (acquired immune response). MHC molecules: every natural population, is diverse in terms of MHC genes / molecules; Mechanism that cause diversity: polimorfism (given locus many polymorphous variant of the genes can be present) Proteins of identical functions (MHC-I and II) are encoded by 3 separate sets of genes Polymorphism - affect mostly peptide-binding grooves (MHC-I peptide-binding grooves are only alpha chains; beta 2 microglobulin is identical for every MHC-I molecules; alpha chains = diversity) - in MHC-II the groove is formed by 2 protein chains (diversity is created by both alpha and beta genes; the variance is really high) ~8-10 minutes moment of the lecture record by classic genetics, 25% of the offspring can have identical set of genes as parents The MHC diversity was created by different selection forces: - different epidemics could be most important driving force for such diversity - not every peptide will fit well for peptide-binding groove - when vital infection, depending of the variety of MHC molceules, some peptides will binds nicely than others - individuals that can bind these peptides *presenting peptides) will be better protected, therefore will main likely survive Pathogen – co-evolution; better chances if heterozygotes; Inbrain strains (homozygous) are susceptible to epidemics; personal remark: have you ever consider Immunology vs The sin of incest? Incest is considered a terrible sin. My thoughts goes towards the decrease of variability, which may lead to auto immune diseases of inbrain strains The presentation of peptides through MHC-I is the most effective way of fighting viral infection; 1st barrier against virus → interferons 2nd barrier against viral → MHC-I antigen presentation (most efficient) 3rd mechanism will be described later There are 2 pathways that cytotoxic T lymphocyte can kill infected cells - granules (perforins) - Fas-dependent killing END L3 missing (pdf) MHC are genes, HLA are the proteins MCH I (HLA-A, HLA-B. HLA-C) *MHC class I binds peptides 8-10 peptides long (size) → hydrophobic peptide binding groove is highly hydrophilic CD8 T cells recognizes MHC I antigens TCR needs to be able to recognizes both MHC I complex + antigen The mutual recognition triggers change of conformation and action thought CD3 allowing for the T cell response; MCH II (HLA-DR, HLA-DP, HLA-DQ) binding cleft here is wider than MHC I (larger antigens allowed) CD4 T cells will recognizes here (instructions further for dendritic and other phagocytic) Invariant chain role* Ix8=8 II x 4 = 8 Trick to ID which T cell will presentation L3 (see notes) CD 34 STEM CELL MARKER (see other markers above) CD14 – receptor for liposacharide TCR – detect MHC molecules (I and II), presented in the binding groove; TCR inside part (tail) is too short to transmit signal But, attached to the CD3 complex, it does transmit signal (below) TCR recognition signals for CD3 phosphorylation (ITAMs) , that will follow ewith the cascade Lymphocytes that carry CD8 = cytotoxic T cell or CD 8 T cell CD4 T cells or Helper T cells T helper cells APC* … usually, interleukenes, growth factors, cytokenes… they are different secreted proteins originated from T cell signaling, which is incredibly complex (many pathways – activation of TCR on Helper cells) record 33’ (“difficult part”) Major mechanism of diversity (T cell) 1 α Constant to 2 β Constant Constant to 2 β to Constant to 2 β 2 Constant to 2 β β Constant to 2 β Constant Constant to 2 β Dozens Constant to 2 β αβ Constant to 2 β possibilities Constant to 2 β for Constant to 2 β Variable Constant to 2 β → Constant to 2 β β Constant to 2 β segment Constant to 2 β is Constant to 2 β more Constant to 2 β diverse Constant to 2 β (VDJ) Constant to 2 β than Constant to 2 β α Constant to 2 β part Constant to 2 β (VJ) DNA Constant to 2 β rearrange Constant to 2 β (Thymus) Constant to 2 β – Constant to 2 β occurs Constant to 2 β randomly Constant to 2 β WHAT’S ADD DIVERSITY HERE (VARIABLE CHAIN) IS THE DNA REARRENGEMENT NOT FURTHER SPLICING 12-23 rule RAG1 and RAG2 genes are silenced in all cells, except is in Thymus (differentiation of T cells) and Bone marrow (differentiating B cells) Thus, Hetamop Stem Cells and Lymphocyte progenitors don’t have Rag1 and Rag 2 proteins; only when they enter Thymus these proteins are produced. These proteins detect the segments (VDJ) and attach them together 1) activity: joint 1 and 2 2) activity: endonuclease – start cut V segment from the part that won’t be necessary in further stages 3) activity: joint unnecessary DNA making them circular, which is a sign for degradation Rag sites are known as RSS (recombination signal sequences) ...”remember about there are 2 types of recombination signals sequences; since these sequences are recognized by different Rags, regulates proper assembly of segments” 1st. Tdt – Terminal deoxynucleotidyl transferase (randomly add nulceotides to the end of theses segments (VJD) 2nd. Pairing strands; by finding complementary, is still possible to find not complementar pair of bases, which can be dumped 3rd . Umpaired are removed, the gaps are filled with DNA syhnthesis and joint by DNA ligase Why Allelic exclusion? - Only allele (one variant) of the TCR is expressed on the T lymphocyte. The receptors from 2 alleles should not be expressed. Combinational diversity (Rag 1 and Rag2) Junctional diversity (Tdt): endonucleases, ligases segments Notch receptor – Notch ligand Receptor and transcription factor at once (Notch is cleaved and the interior part goes to the nucleus acting as TF – this will imply in production of TCR (αβ) and CD3; ...”if happens that a TCR is not able to properly bind with MHC molecules, Tymocite won't get the positive signal and will die within 3 days” http://www.bio.davidson.edu/courses/immunology/flash/main.html “Those able to survive – passing the selection processes – reaches the Thymus medula region” T cell recognition of foreign peptide antigen and tolerance to self peptides is key to the proper function of the immune system. Usually, in the thymus T cells that recognize self MHC + self peptides are deleted and those with the potential to recognize self MHC + foreign peptides are selected to mature L4 Lymphoid Stem Cell → B cell pathway to differentiate is like default pathway (for all that do not enter into the Thymus) Bone Marrow (central organ where B differentiate) Lymphonodes (peripheral where B differentiate) B cell receptors -BCR similarly TCR are needed CD3 complex; BCR requires Igb, Iga, slg BCR belongs to APC (Which are the APCs?) mature BCR markers: CD19, CD20, CD22 Types of Ig - examples of 2 Transcription Factors that goes after activation of BCR signaling: NFT (nuclear factor of activated T cells); NFkB “most complicated part in immunology” ~ 23’ (recordings) In comparison with T cell variable region diversity, Ig variable chain diversity is bit more complex because we have only ONE gene that encodes for the Ig heavy chain, but we have TWO separate genes encoding for light chains (λ Constant to 2 β and Constant to 2 β κ)) DNA Constant to 2 β rearrangement All Constant to 2 β life Constant to 2 β of Constant to 2 β B Constant to 2 β cell Constant to 2 β the Constant to 2 β 1st Constant to 2 β rearrangement Constant to 2 β occurs Constant to 2 β in Constant to 2 β heavy Constant to 2 β chain Constant to 2 β of Constant to 2 β Ig Heavy chain has many segments that encodes constant parts of Ig – different classes and subclasses of Ig with different constant terminus, therefore, primary RNA transcripts encoding heavy chain contains all possibles classes and sub of Ig When Constant to 2 β RNA Constant to 2 β transcripts Constant to 2 β are Constant to 2 β being Constant to 2 β produced, Constant to 2 β creates Constant to 2 β primary Constant to 2 β RNA Constant to 2 β later Constant to 2 β processed Constant to 2 β by Constant to 2 β splicing splicing Constant to 2 β process Constant to 2 β which Constant to 2 β constant Constant to 2 β regions Constant to 2 β will Constant to 2 β be Constant to 2 β translated Constant to 2 β in Constant to 2 β the Constant to 2 β proteins - Constant to 2 β heavy Constant to 2 β chain Constant to 2 β is Constant to 2 β similar Constant to 2 β to Constant to 2 β beta Constant to 2 β chain Constant to 2 β of Constant to 2 β the Constant to 2 β T Constant to 2 β cell Constant to 2 β receptor - Constant to 2 β made Constant to 2 β out Constant to 2 β of Constant to 2 β 3 Constant to 2 β types Constant to 2 β of Constant to 2 β segments: Constant to 2 β V, Constant to 2 β D, Constant to 2 β J Constant to 2 β at Constant to 2 β the Constant to 2 β beginning - Constant to 2 β random Constant to 2 β V Constant to 2 β is Constant to 2 β rearranged Constant to 2 β with Constant to 2 β J - Constant to 2 β random Constant to 2 β D Constant to 2 β with Constant to 2 β D Constant to 2 β J Constant to 2 β segments Light chains 2 alternative genes - 1st chain to be rearrenged ins K chain - random J segment attached to random V segment - after rearrangement, the only one constant chain is being attached - light chain is ready for transcription - RNA is processed and ready for translation If K fails, λ chain is processed - RAG1 and RAG2 acts similarly in case of TCR The action of sequential cleavage, create a signal joint produces a circular DNA that will be later degrated important ...”RAG1 RAG2 binds two different types of signaling sequences and only two different types can be put together.” - Tdt 1st. Tdt – Terminal deoxynucleotidyl transferase (randomly add nulceotides to the end of theses segments (VJD) 2nd. Pairing strands; by finding complementary, is still possible to find not complementar pair of bases, which can be dumped 3rd . Umpaired are removed, the gaps are filled with DNA syhnthesis and joint by DNA ligase * Majority of the cases, these segments don’t form coding regions, triplets, therefore will be removed / degraded - Allelic exclusion (Wikipedia) Allelic exclusion is a process by which only one allele of a gene is expressed while the other allele is silenced.[1] This phenomenon is most notable for playing a role in the development of B lymphocytes, where allelic exclusion allows for each mature B lymphocyte to express only one type of immunoglobulin. This subsequently results in each B lymphocyte being able to recognize only one antigen.[2] This is significant as the co-expression of both alleles in B lymphocytes is associated with autoimmunity and the production of autoantibodies.[3] Many regulatory processes can lead to allelic exclusion. In one instance, one allele of the gene can become transcriptionally silent, resulting in the transcription and expression of only the other allele.[2] This could be caused in part by decreased methylation of the expressed allele.[4] Conversely, allelic exclusion can also be regulated through asynchronous allelic rearrangement.[5] In this case, both alleles are transcribed but only one becomes a functional protein.[2] In Igκ and Igλ light chain genes The allelic exclusion of light chain genes Igκ and Igλ is a process that is controlled by the monoallelic initiation of V(D)J recombination. While little is known about the mechanism leading to the allelic exclusion of Igλ genes, the Igκ locus is generally inactivated by RAG-mediated deletion of the exon Cκ. The V(D)J recombination step is a random and non-specific process that occurs one allele at a time where segments V, (D) and J are rearranged to encode the variable region, resulting in a fraction of functional genes with a productive V(D)J region.[11] Allelic exclusion is then enforced via feedback inhibition where the functional Ig gene inhibits V(D)J rearrangement of the second allele. While this feedback mechanism is mainly achieved through inhibition of the juxtaposition of V and D-J segments, the downregulation of transcription and suppression of RAG accessibility also plays a role. [12] - estimated total diversity of human Ig and TCR molecules are quite similar ~ 10E12 B cell maturation Bone Marrow At this point, Heavy chain is being rearranged; gene start to be transcribed, RNA is being produced, spliced in such a way that class M is being produced (transmembrane class M); This heavy chain IgM is being attached to µ chain; When IgM is present in the surface, it sends a signal to the cell to alternatively splice heavy chain mRNA, afterwards, IgD is being produce in parallel B cells that have both classes IgD and IgM can exit Bone Marrow and go to bloodstream. JUMP FORWARD >>> Removal of potentially self reactive immature lymphocytes by clonal deletion - 1st selection of B cells at Bone Marrow High signal of self antigens are marked to apoptosis and do not exit Bone Marrow. * only 10% of all B cells leave Bone Marrow and enter the lymphonodes - 2nd Lymphonodes Germinal center B cells that proliferate in the dark zone are allowed to mutate. Only in the variable region of Ig genes (all other places and situations biological mechanism preventing gene mutation by correcting etc). Only when the affinity antigen and Ig are appropriate, B cells move to the Light zone. All mutations that produce worse Ig (non functional) undergo apoptosis Better the mutation bigger chance B cell to survived. - Here, Helper T cells interaction recognizes antigen brought via Dendritic cells; - Tip! The presence of Helper T cells recognizing antigen brought from Dendritic cells automatically means that this antigen is not a self antigen (T cells that recognizes self antigen are not selected in the Thymus [medula cortex] therefore don’t exit the organ). - If B cells presents an antigen that is recognized by Helper T cell, it’s a confirmation that the Ig produced by this B cell is not dangerous (final signal for B cell keep alive) - All B cells that don’t get this signal from Helper T cells will eventually die. - Signal from T helper cell leads to 2 different events 1) proliferate and become Plasma cells (final step of B cell differentiation) - short lifespan (few weeks) but produces many types of Abs (class switching) that are secreted; 2) little fraction become Memory B cell - in contrast live longer (dozen years) - highest affinity with the antigen - express a lot of antiapoptotic Bcl-2 protein (associated with the longer life of memory B cells) * some can live more than 65 years ~ 3% of B cells generated in Bone Marrow survives and eventually produce Antibody JUMP FORWARD >>> … the contact with Helper T cells decides the remaining classes of Ig (after IgM, IgD) Remember: This contact*: is processed during RNA splicing of Heavy chain * Primary contact with the antigen → results in Primary response Classes and Subclasses Ig - IgM No subclass; Humoral response (production of Ig); strongly activate complement system; do not fit antigen very well (early Ab); IgM create pentamers; The monomoreic igM can only exist in plasma membrane, while secreted always pentamer - IgD No subclass; present on developing B cells (they need to be present in the plasma membrane in order to let B cells exit Bone Marrow) - IgG (The most important in function in our immune system) - IgA 2 subclasses: IgA1, IgA2 (secreted by mucous membranes) - IgE (healthy person level is very low – parasites or allergy cases increases) Attention to Fc receptors → B cells can bind antigen by BCR and also bind Ig by Fc receptors (Fig) B cell x T cell review - Constant to 2 β β chain T cell and Heavy chain B cell are akin - Light chain B cell and α chain T cell are akin Goals for B cell dev: - Diverse antigen - eliminate self reactive - promote maturation Heavy chain (3 genes segments): V (variable), D (diversity) and J (joining) Light chain: V, J - surrogate light chain - Large Pre B/T stage: Heavy chains (B) / β chains (T) are being tested to check if further matching, Light / α chains, will have affinity to binding; Genetic Mechanism of Diversity 1. Inherit multiple V, D and J regions 2. Recombine the segments 3. Recombinational inaccuracy – TdT 4. Random assortment of chains 5. Somatic Hypermutation Selection for T cell: + for MHC; - for self-antigen Selection for B cell: - Isotype switching (is a permanent change) – producing only one type of Ig forever (CD40 / CD40 ligand → AID enzyme) L5 Inflammation V D J Complement System Mode of action (“Classical Pathway”) - starts with Ig - Antigen binds Ab (opsinizing) ~ Fc region of Ig (sticking ends) - Fc receptors mainly responds to Ig; another is C1 (element 1 complement system); preferentially IgM binds to C1 (IgM pentamer when secreted) - binding changes the conformation of C1 – proteolytic activation - proteolysis of C2 and C4 (each elements is cut into 2 pieces) - new complex formed accelerate hydrolysis of C3 - C3 intrinsic proteolytic activity - C3 is also cutted - C3b will activate proteolysis of C5 - C5 is cutted in two (a and b) - change of conformation; C5b complexes with C6, 7, 8 - They attach to the plasma membrane of the cell wall of the microbe - This complex build in the cell wall and creates an environment for further oligomerization - oligomerization brings several of C9 molecules - forming a pore in the cell wall FIG below C1 can also binds Lectins Mode of action: “Alternative Pathway” Based on the permanent proteolytic activity of C3 - C3 is cutted into C3b C3b in given body will be inhibit, but in a foreigner surface will lead to proteolysis C3 hydrolysis * Often the very first answer to pathogens is by activatin the Complement system I summary, if there’s no Antibody, Alternative pathway. If in one hand, lysed fragments of the C elements have their bigger fragments using the letter b, i.e., C4b, C3b, in another hand, the smaller a fragments play an important role in inflammation responses - dilatation of blood vesses - release of histamine from mast cells - chemotaxis of phagocytes C3b and opsonization, meaning covering all Rhinovirus and inflammation - What is the role of ICAM-1 Mediators of inflammation - Performed mediators (fast released) - Lipid mediators (slower released) plasma membrane phospholipids, processed by enzyme phospholipase A2 → enzyme is activated by stimulus; cuts arachdonic acid from phospholipids of PM … COXs → prostaglanding - Late mediators (hours to be generated) Cytokines, chemokines, growth factor, proteins produced by basophiles and mast cells; after transcription of their actived genes; recruit of immune cells, tissue repair, vascular permeability Endothelium (2 inner layers) - blood vessel in stationary state (no inflammation): tight junctions, adhesion, basement membrane, cytoskeleton fibers 1) Leukocyte capture chemokines (aka chemotactic cytokines) - Chemokines from the tissue (basement) are engulfed and transported escaping lysosomal degradation, and presented to inner surface of the endothelium, where there are sugar groups (glycocalix) - When this happen, Leukocytes that have chemokines receptors start to attach to these chemokines - This attachment is usually not so strong 2) Rolling selectins proteins (binds sugar moieties) present both in Leukocytes and endothelial cells; Also this sugar moiety is present in both type of mentioned cells - Sugar selectins interactions, Leukocytes slow down and are marginalized selectins (Fig) 3) Slow rolling and Firm adhesion Integrins - αβ heterodimer ~24 types identified - change of conformation cause the intracell domain to reorganize actin cytoskeleton of the Leukocyte (making it flat and more favorable for migrate) - Transmigration - Reorganization of surface leucocytes proteins (expression of adhesion and tight junctions proteins on the Leukocyte surface, allowing physical migration - This leads to proteases that helps migrating and degrade basement membrane, reaching extracellular matrix in the tissue “Whatever cell that attracted via chemokines may migrate like these” - fibroblast, keratynocyte… all leaded after wounding process for the repair - when the area is cleared, mediators of inflammation stopped to be produced, no longer Leukocytes are attracted ans so forth FIG Cytokine release syndrome (CRS) or Cytokine storm syndrome (CSS) - exaggeration production of inflammatory cytokines *Influenza can cause CSS (spanish flu 1917-1918) L6 COX1, COX2 * inhibition of them – salicylic acid (Salix alba) see precise enzyme inhibition here COX1 (see alternative notes) - Preferential COX2 inhibitor i.e. Diclofenac - Selective COX2 inhibitor (coxibes) i.e. Celecoxib Steroids Why? (see notes) Cortisol (notes are very complete this L6) Lipocortin: protein blocks PLA2 (phopholipase A2) ...there are many genes activated via transcription factors by lipocorticoids (i.e. Lipocortin) … lipocorticoids acts as TF and antigens L7 Vaccines (alternative notes) PS. read slides here only L8 (folder L7) ...”Not killed but inactivated virus” Polio Salk vaccine HB (slides + alternative notes) Understanding of mRNA vaccines every muscle cell injected with mRNA vax mRNA → proteosome MHC class I part will become memory T cell Techniques for succeeded mRNA vaccine: - stabilization of mRNA (ψ) - codon optimization (Toll-like receptors normally detect viral RNA) - proline substitution - addition of signal peptide (i.e., covid Pfizer tech ~ in addition to MCH-I, also little bit of the spike protein goes out of the cell so B lymphocytes can detect and generate Antibody) Covid Inactivated vaccines Attenuated vaccines Protein vaccines (similar to Hepatitis B) Adjuvants L9 (folder 8) Immunology transplants - Blood transfusions Today’s nomenclature During 1st World War, Ludwik H on Serbia (first aid war stuff) found the diversity of blood composition among races (fig below) ...II Wolrd War context: Ludwik escaped Warsaw as he was been kept hostage due to be Jewish to Wrocław. Up to this day there’s (famous) Immuno Institute with his name in Wrocław. ABO system Anti-A and anti-B are IgM Rh system - Anti-Rh (D) are IgG - they are not produced in people that have not contact with Rh (-) - after the contact of a negative Rh will begin to produce Ab against Rh Organ transplant - Skin - Cornea transplant does not involves MHC class molecules - Cyclosporine In general, MHC class molecules are The responsible for rejection mainly. - Autograf, Isograft, Allograft, Xenograft Rejection 1 - Induction phase 2 - Effector phase - Foreigners antigens trigger faster responses - Direct allorecognition vs Indirect allorecognition - Mice without Thymus do not reject transplants (B lymphocyte are not enough for rejection) Bone Marrow transplant - Auto: usually people who have had or still have cancer - Allo: needed in different situations; (allogeneic) HSC - they all possess CD34 - column antiCD34 Coming back to Cyclosporine - Inhibit signal from T cell receptor to nucleus → TCR cannot be activated - Cytotoxic T cells do not responds Tacrolimus (FK-506) and Rapamycin (sirolimus) - Inhibit activation by TCR or Interleukin-2 (IL-2) → cytokine important for activation of * inaudible Azathioprine - sometimes used as anti-cancer - block any proliferation of cells (cytotoxic nucleotides into DNA) Methotrexate - blocks pathways of nucleotide production +OKT3 (Antibody) – responsible for signal transduction of TCR (cytotoxic T cells and Helper cells); T cells dies from apoptosis IL-2 blockers Summary of nowadays drugs for transplants (immunomodulating drugs) L9. Immuno of reproduction trophoblast* MHC molecules could trarget baby cells (transplanting like) Why embryo is not rejected? * nucleited cells → MHC molecules (but does not produce classical MHC; but are rich in non-classical MHC class molecules; the most important G type classical : Types A, B → The fact that trophoblast carry the type G (MHC non classical one) makes the cytotoxic T lymphocyte (CD8 cells) do not recognize them as foreigner → HLA G Why NK cells are not cytotoxic? The other mechanism is: IDO IDO – catalyze Tryptophan (disrupt) Insuficiency of Trp Another mechanism: Progesterone Balance between TH1 TH2 (T helper cells): normally in humans half / half Pregnant women: Immuno defesne is more by antibodies than cytotoxic cells Fas ligand mechanism activated T cells and NK cells they have Fas ligand Trophoblast is capable of induce apoptosis → Because T cells also have Fas receptors → Mom basically produces Ag that protect the baby → Autoimmune or clotting disorder: for example, Antiphospholipid syndrome Fetus B lymphocytes start to produce first Ag (IgM) before the delivery - with six months 100% lvl of production is only IgM In terms of Ag a newbor is very helpless transfer of Ag from mom to baby → the moment the baby is delivered, IgG mom’s Ag decreases - Neonatal Fc receptors (FcRn) Only class G is transported mom→ baby (via FcRn) active transported - Hemolytic disease of the newborn (HDN) * erytrocytes do not cross placenta, only Ig’s IgD is responsible for Rh +/- recognition (mom – fetus) - anti-D IgD → lysis of kid’s erythrocytes (bilirubin) phototherapy (degrades bilirrubin) Breast Milk → Colostrum: first milk (yellowish) - Similar with trophoblast, the Intestine of the newborn also contains FcRn receptors; - Binds Ig from human milk - When baby is fed → IgG active transported to the blood stream of newborn * Avoidance of Breast milk when HIV; TB; antibiotics “ mainly IgA’s surround the pathogens inhibiting they to bind with healthy tissues thus limiting their power of action” L10 Poly / Monoclonal Ag → production → IVIG (intravenous immunoglobulins) contain mix of IgG from healthy donors Monoclonal: - principles 1, 2, 3 TK / HGPRT - The HAMA response (human anti-mouse antibody) side-effects in humans … to take fully Hybridomas from mouse to isolate gene; cut the variable region; clone into human gene; replace variable region from human Ig for mouse variable → chimeric … to clone only this part of the variable region Humanized mAb are different story; they do not undergo Animal immunization for instance HAHA (human anti-humanized antibody) … after opsonization, complement system will take place (ADCMC) … then destroy the cells … cytotoxic T cells also - we must remember: IgG last longer; IgM very efficient (when? Inaudible) … IgM ELISA (~1hour – record) Western blot (~1h6’) differences between them in antigen antibody assays SDS-PAGE - transfer semi-dry - transfer wet Mad cow diseases Immunoenzymatic pregnancy tests: Lateral Flow Immunoassay (cheap; accurate in most cases) One flowing line of Ab; One mAb recognize Ag. - example: immunoenzymatic pregnancy tests (most tests look for the presence of Beta subunit of hCG or human chorionic gonadotropin both hormones in blood or urine. (very accurate test – high affinity Ab) Covid IgM/IgG rapid test Flow Cytometry (experiment / diagnosis) - Forward scatter signal intensity is ~ proportional to cell csize - Side scatter signal intensity is proportional to cell granularity - choose the plorophore prior to experiment / diagnostics PS. In case she asks alternative test than Antigen (rapid test) for Covid : Using Flow Cytometry to Detect COVID-19 New research has suggested an alternative flow cytometry-based method of testing for the SARS-CoV-2 virus. Flow cytometry is a method that is used across different fields of science to analyze single cells or particles. (source: https://www.news-medical.net/life-sciences/Applications-of-FlowCytometry-to-COVID-19.aspx) Fluorescense Activated Cell Sorting (FACS) – slower than FC L11 Immunodeficiencies - primary (genetic treats) -acquired IgG cross placenta to the kid; ~ 4-6 months this isn't enough anymore (meaning kid has to produce Abs) - XLA disease (lack of antibodies) – treatment: IVIG (intravenous Human immunoglobulins) shots of mixed IgG - SCID (severe combined immunodeficiency) most problematic one 1h11’ records (L11) L12 Immunology of cancer “The Ras protein is a small G protein that is activated when guanosine triphosphate is phosphorylated, which in turn leads to the activation of downstream pathways that play an important role in cellular differentiation, proliferation, and motility and together can act synergistically to promote tumorigenesis.” - Oncogene (dominant genes – 1 allele is enough) General oncogene activation (picture above) - suppressor gene (recessive gene – 2 alleles must be affected for presenting phenotype) “first barrier protecting us: DNA repair” “second barrier is antigen presentation by MHC I” *See viral infections - tumor-specific antigen / tumor-associated antigens → Cytotoxic T cells kilsss target cell in 2 different ways (recap): Perforindependent killing; Fas-dependent Killing “Tumor cells can escape this barrier by downregulating MHC I” “3rd barrier is NK cells” 2 mechanisms of NK (exact same as Cytotoxic T cells) - see table: cancer incidence in immunosuppressed patients “Again, some tumor cells can escape cell killing by Tc and NK, which use Fas ligand” cancer cells quite often express Fas ligand on their cell suface (killing Cytotoic T cells); and production of soluble Fas ligand Another mechanism: PD PD receptor – ligand: protect our body from “auto-aggression”? (non audible) Tumor-associated Macrophages (TAMs) → at a first glance, these macrophage present standard genes, however, the tumor environment promote signals that make them TAM playing in tumor favor The father of immunotherapy (William Coley) try Google this: “why coley’s toxins was not successful?” The role of Interleukin 2 in cancer - mAb anti CD20 activate Complement system and Cytotoxic T cells which will kill cells overexpressing CD20 - tumor often stop producing key cytokines leading to angiogenic factors (production of blood vessels); anti VEGF - mAb anti HER2 – Herceptin L13 Paul Ehrlich (1854-1915) Immune tolerance Regulatory T cells (suppressor T cells) Transcription factor FOXp3 (TF of Regulatory T cells) → Regulatory T cells are attracted by TAMs to the tumor environment and cytotoxic T cells cannot kill cancer cells due to this IPEX syndrome – FOXP3 mutations - females are usually carriers - CD25 and FOXP3 are essential for T regulatory cells Autoimmune diseases - systemic - local → Thyrotoxicosis (often fever; high blood pressure; nervous; “crazy big eyes”) treatment: remove pituary gland; beta blockers; radioiodine → Exophtalmos treatment: corticosteroids see diagram in the picture below → Diabetes type 1 immune autoagression autoimmunes destruction of insulin producing beta cells of the pancreas lack of insulin leads to increased blood and urine glucose - effector t cell recognizes peptides from a beta cell specific protein and kill the beta cellular treatment: insulin (porcine or recombinant) / pancreas or islet cell transplantation see slide diagram of islet cells → Systemic Lupus Erythematosus (SLE) - very severe, attack virtually all tissues; difficult to diagnosis; - 9 females to 1 male ratio - cased by ANA (Anti-nuclear Antibodies against various DNA, histons, RNA and others) - patient’s serum reacts with nuclei treatment: nonsteroidal anti-inflammatory drugs; corticosteroids; anti-malarial drugs; immunosuppressants; avoid sunslight; diet; exercise; vaccinations * AS Antiphospholid syndrome is often associated with SLE (check what’s the thing with AS) L14 Inflammation Type I - IgE mediated release of histamine and other mediators from Mast cells and basophils (lots of Fc receptors that recognize with IgEs...) - Allergy belongs to Type I * B cells will secret IgEs, remember B cell processes - When IgE binds to e.g. Mast cell… 1) 1) B cells leads to granulation (produces granules) 2) Plasma membrane starts to react with Fc receptors and signaling - phospholipase A2 processes phospholipids from the plasma membranes - this processing results in Arachdonic acid, which are substrate for production of prostaglandin, Leukotrienes (INTERMEDIATES OF INFLAMMATION or MEMBRANE DERIVED) 3) transcription of genes that encodes cytokines that are respponsible for inflammation - if bacteria is responsible for inflammation, IS NOT IgE → Acute response - Histamine - Leukotrienes → Anaphylactic Shock and Acute Allergic reaction treatment: EpiPen / EpiPen Jr → Late response Asthma General lines: - Allergy is a Type I Hypersensitivity (there are 4 types of hypersensitivity) - so called allergen stimulate the overproduction of IgE - When we talk about Allergy it has to be IgE involved In case of edema, there are no IgE (usually cytotoxic t cells are involved) testing Skin puncture – positive control = histamine segative = saline solution blood IgE level Hygiene hypothesis Anti-histamine (blocks symptons) - block binding of histamine to H1 receptors (claritine, zyrtec, alertec, etc – sideeffects exists) Corticosteroids (we can give It locally, e.g., asthma – no side-effects) Cromones or Mast cell stabilizers