Malaria Lecture Notes: Causes, Life Cycle, Global Impact
advertisement

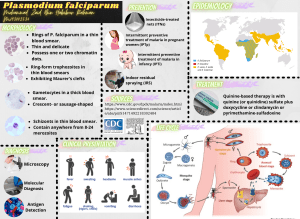
COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno MALARIA Malaria is a mosquito-borne infectious disease caused by a eukaryotic protist of the genus Plasmodium Mal (Bad) + Aria (Air) = Malaria (Bad Air) o This “bad air” was believed to be the cause of the fever that often developed in those who spent time around the swamps. o In fact, the illness, now known as malaria, was due to certain protozoon present in the mosquitoes that bred around these swamps, and which caused recurring feverish symptoms in those they bit Picture Above: Estimated cases and deaths in Asia (2010) This just shows that here in the Philippines there is a decreasing number of case and deaths due to malaria (as compared to other countries) Picture Above: Distribution map of malaria We always say that malaria is a disease of the tropics. Tropics areas between the tropical belts of Capricorn and Cancer, with the equator in the middle. At the map, all the areas encompassed by tropics of Cancer and Capricorn are all tropical countries (they are different from the temperate countries that are outside the tropical belt). In tropical countries, there are diseases inherent to them because of the humidity and temperature making some diseases conducive for its inhabitance Malaria: OVERVIEW Most important parasitic disease in humans globally. Causes a heavy burden among tropical countries. This is because the vector that carries malaria thrives in environments of tropical countries Poses a threat to non – endemic countries. Poses a danger to international and local travelers. Transmission of Culex us almost nil; Anopheles need large size of fresh water to survive Disease caused by protozoan parasites called Plasmodium. It is usually transmitted through the bite of an infected female Anopheles mosquito. Malaria may also be transmitted through the following: o Transfusing blood that is positive for malaria parasites This is because malaria parasites reside in the RBCs o o Sharing of IV needles (especially among IV drug users) Transplacental (transfer of malaria parasites from an infected mother to her unborn child) LIFE CYCLE Picture Above: Malaria Program Phases How is the Philippines faring in terms of contribution to global deaths due to malaria? Our country is shaded in light blue little by little the Philippines contributes less and less number of deaths secondary to malaria in terms of worldwide statistics. Even the countries around use like Thailand, Cambodia, Lao PDR, & Vietnam there is also decrease in malaria prevalence and death cases. However, there are countries a little bit far from us that have contributed highly to the global statistics of deaths due to malaria #GrindNation Strength in knowledge Page 1 of 9 COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno Explanation of the Life Cycle of Malaria Parasite: An infected mosquito will try to bite the human host. Remember that the mosquito should be an infected Anopheles. The human host will receive all the saliva coming from the mosquito the parasites received are called sporozoites. The sporozoites will go to the liver, and depending on the specie of the Plasmodium, they may reside in the liver for a longer time or the sporozoites may burst from the hepatocytes released into the blood circulation. Once the sporozoites are inside the liver, this is called extraerythrocytic life cycle of plasmodium. Eventually, the hepatocytes will burst parasites coming out are now called merozoites, they will attach themselves to the RBCs (depending on the specie, they attach to specific RBCs). The merozoites will go inside the RBCs to change its internal milieu so that it will be conducive for it to replicate. Once its replicates in the RBC this is now called the erythrocytic life cycle of plasmodium. One replication of merozoite in the RBC will be able to release hundreds of merozoites (this depends again in the specie of Plasmodium). The released merozoites will infect naïve or unaffected RBCs. Inside the RBC is what we called the gametocytes (merozoites become male or female gemetocytes). In the human blood, these gametocytes will not reproduce they will just be freely swimming in the circulation until a mosquito (infected or uninfected) bites the human host gametocytes are sucked by the mosquitoes. Inside the body of the mosquito, the gametocytes will reproduce and they will release the male & female gametes. The gametes will eventually mature to become sporozoites inside the mosquito gut. During the early stage of intraerythryocytic development, small “ring” of the different species s appear similar By the end of 48 intraerythrocytic stage (24 for knowlesi, 72 for malariae), the parasite has consumed two thirds of the hemoglobin and is now called a schizont Multiple nuclear division have taken place (schizogony or merogony) and the RBC then ruptures to release 6-30 merozoites, each can infect RBC The disease in humans is caused by direct effects of RBC invasion and destruction by the asexual parasite and the host’s reaction After a series of asexual cycles (p. falciparum), or immediately after release from the liver (vivax, ovale, malariae, knowlesi), some parasites develop into gametocytes that can transmit the malaria Male and female gametocytes form zygote in the insect’s midgut Zygote then matures into ookinete which encyst in the gut wall The resulting oocyst expands by asexual division until it bursts to liberate sporozoites which then migrate to the hemolymph to the salivary gland of the insect Sexual Life Cycle of Plasmodium it is inside the mosquito gut Asexual Life Cycle of Plasmodium it is inside the human host Definitive host of Plasmodium mosquitoes (because the sexual life cycle happens inside them) Summary of Plasmodium Life Cycle: Step 1: The mosquito takes a blood meal from an infective individual. Sporozoites (the sexual phase) occurs in the gut of the mosquito. Step 2: preerythrocytic stage. Asexually reproduce can be as many as 100,000 merozoites rupture of hepatic cell attach to RBC (erythrocytic stage) Step 3: erythrocytic stage. Asexual stage. 1 merozoite infects 1 RBC asexually reproduce then the RBC bursts Step 4: not reproduce sexually in humans. The female and male gametocytes need to be sucked by the mosquitoes Step 5: oocyst release several sporozoites in the abdomen ETIOLOGY AND PATHOGENESIS Human infection begins when a female anopheline mosquito inoculatrs plasmodial sporozoites from its salivary gland during a blood meal These motile forms of the malarial parasite are carried rapidly via the bloodstream to the liver, where they invade hepatic cells and begin asexual reproduction This amplification process is also known as intrahepatic or preerythrocytic schizogony or merogony Swollen infected hepatic cell eventually burts discharging motile merozoites into the bloodstream Merozoites invade the RBC and multiply within 48-72 hours When parasites reach density of 50/ul in the blood, symptomatic stage begin P. vivax and ovale – portion of intrahepatic forms do not divide immediately but remain dormant. This is the cause of relapses. The dormant form is called hypnozoites Merozoites enter the RBC and become trophozoites. P. vivax receptor is Daffy group antigen Fya or Fyb. West Africans have FyFy phenotype – makes it resistant to P. vivax malaria. #GrindNation Strength in knowledge Page 2 of 9 PLASMODIUM SPECIES There are 4 major species that causes malaria: 1. P. falciparum 2. P. vivax 3. P. malariae 4. P. ovale What are the common species of malaria parasites in the Philippines? o Plasmodium falciparum and Plasmodium vivax are the common species of malaria parasites in the Philippines o P. falciparum 60-70% o P. ovale 30-40% There are also P. malariae cases and contributes to about <1% of the total malaria cases. P. falciparum malaria, if not treated immediately, can lead to severe malaria, such as cerebral malaria. P. vivax malaria does NOT lead to cerebral malaria but it causes relapse if treatment was not completed. P. falciparum – in the Philippines P. ovale – in Africas P. falciparum – in Asia COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno Plasmodium knowlesi Molecularly, entomologically, epidemiologically, data, indicate that human infection with P. knowlesia is not newly emergent Primarily a zoonotic for reports of its emergence from monkeys Potentially fatal, but if detected early enough, infections in humans are readily treatable Isolated from Philippine macques (maccaca fasciculus) in 1961 Incriminated vector in Anopheles balabacerisis Published reports of human infection: o 1965, 2004 – Malaysia o 2004 – Thailand o 2006 – China o 2008 – Palawan (Philippines) ~2 cases Morphologically similar to P. falciparum and maybe mistake to be P. falciparum PCR is of value in diagnosis because P. knowlesi infection is easily misdiagnosed as less dangerous Plasmodium malariae infection with conventional microscopy Notes from Old Trans: P. falciparum: Has the shortest/ fastest hepatic phase; less than a week Has the biggest release per hepatocyte Attacks ALL type of RBC P. malariae: Has the longest duration of erythrocytic stage. Attack senescent cells (reason why it is benign senescent cells will die anyway) P. falciparum and P. knowlesi Species that have ring forms (reason why some P. knowlesi cases are are mistaken as P. falciparum) P. vivax and ovale Schuffer’s dots – the hypnozoital forms – the cause for the relapse of infection because duration in intrahepatic can be very long Incubation Period: P. falciparum (12 days) P. vivax (14 days) P. malariae (30 days) PARTS OF THE MOSQUITO Clinical Presentation: Morphologically similar to P. malariae or may be mistaken to be P. falciparum because of abundant ring stages In Rhesus monkey studies o High parasite densities is possible o No significant sequestration in microcirculation In humans o Reported in children and relatively older adults o May present as mild form of malaria easily responding to chloroquine but may also be severe and fatal Fever, headaches, intermittent chills, abdominal pain, sweating and malaise Characteristic Duration of intra – hepatic phase Number of merozoites released per infected erythrocyte Duration of erythrocytic cycle in hours P. falciparum P. vivax P. ovale P. malariae 5.5 8 9 15 30,000 10,000 15,000 15,000 48 RBC preference Young but can invade all cell ages Morphology Ring forms, banana shaped gametocytes Pigment color Black Ability to cause relapse No 48 Reticulocytes and cells up to 2 weeks old Irregular shaped large rings and trophozoites, enlarged RBC, schuffner’s dots Yellow brown Yes 50 72 Reticulocytes Older cells Infected eryhrocytes, enlarged and oval with tufted ends, schuffner’s dots Bands or rectangular forms of trophozoites Dark brown Brown black Yes No Lecture Discussion: Proboscis major structure of the mosquito head; mouthpart used for sucking Anopheles also called the tiger mosquito of Asia; shares similar traits and appearances with Aedes egypti; they are slender and has very long legs Culex usually found at home; stouter with shorter legs Abdomen it is where the sexual reproduction of the mosquito takes place What is the difference between Anopheles & Aedes? Time of the day when you were bitten Day biting Aedes Night biting Anopheles Do all Mosquitoes carry the Malaria Parasite? No, not all mosquitoes carry the malaria parasite. In the country, it is the adult female Anopheles mosquito that can become infective and therefore carries the malaria parasite after she bites a person infected with malaria. The malaria parasite undergoes several developmental stages inside the adult female mosquito until such time that the mosquito becomes infective with malaria parasites. This anopheles mosquito bites from dusk to dawn (night biting) and it breeds in clear, slow flowing streams that are found in mountainous/forested areas or in brackish water where salt and fresh water meet. This is usually found in coastal areas *Highlighted in yellow were discussed by Dr. Fortuno Can a person get malaria by drinking water in the streams with mosquito eggs? No it will not be possible. The malaria parasite has to undergo development inside the adult female mosquito; therefore one cannot get malaria from drinking water that has mosquito eggs in it. Another is that the gastrointestinal acids will destroy the eggs immediately #GrindNation Strength in knowledge Page 3 of 9 COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno Unstable Transmission: Erratic transmission Usually in hypoendemic areas Full protective immunity is not acquired MOSQUITO VECTORS IN THE PHILIPPINES Anopheles sp. o An. flavirostis o An. litoralis o An. maculatus o An. mangyanus o An. babacensis Statistics: P. falciparum and P. vivax – responsible for most new infections But because of the government’s effort to eradicate P. falciparum, P. vivax is now having an emergence. There is now more incidence of P. vivax than P. falciparum. But in terms of prevalence P. falciparum still is the highest Lecture Discussion: Anopheles is a picky kind of mosquito because it has to live in clean water they would not be able to live in urban areas due to contaminated water. They thrive more in rural areas due to presence of cleaner water P. FALCIPARUM RBC Changes: Once inside the cell, it consumes and degrades intracellular proteins (hemoglobin). Alteration in RBC properties more irregular in shape and less deformable. (less deformability)- disease the malleability P. falciparum – causes appearances of knobs on the cell surface. o Mediates attachment to the capillary and venular endothelium (cytoadherence) infected erythrocytes stick inside and eventually block capillaries and venules o Rosette formation – infected RBCs may adhere to uninfected RBC o Agglutination – infected RBC adhere to other parasitized RBC o Cytoadherence, rosette, agglutination are central to the pathogenesis of falciparum malaria, the result in the sequestration of RBC containing mature forms of the parasite in vital organs (esp. brain) where they interfere with microcirculatory flow and metabolism o Sequestered parasites: splenic processing and filtration only the younger ring forms of the asexual parasites are seen in the circulation o Other “benign” forms of malaria, sequestration does not occur o Very toxic to erythrocytic hemoglobin o P. falciuparum- change internal nuclear degeade to Hb to heme or hemosiderin o Falciparum prefer to survive in hemosiderin type o After invading RBC, malarial parasite degrade hemoglobin and is converted to inert hemozin (malaria pigment) WHO ARE AT RISK OF GETTING MALARIA? Children – because of immature immune system Pregnant women – immunocompromised Indigenous peoples Forest workers, miners, soldiers Persons who are not from a malaria endemic area but travel to this area Table Above: This table shows which provinces have high cases of malaria: Encircled in red are from Cagayan, Zambales, Rizal, Occidental Mindoro, Palawan, Davao Del Norte, Sulu EPIDEMIOLOGY Endemicity is defined as palpable spleen rates in children 2 – 9 years old: (You do Abdominal Exam) o <10% - hypoendemic o 11-50% - mesoendemic o 51 – 75% - hyperendemic (e.g. Cagayan, Zambales, Rizal) o >75% - holoendemic (almost 100% has/had malaria) Africa and New Guinea P. falciparum: Causes severe malaria. Principal Determinants are: Biting habits Density of the mosquito population Longevity of the anopheline mosquito o The lifecycle that takes place inside the mosquito is between 8 – 30 days. o Low temperatures are not conducive for sporogony to take place Stable Transmission: Constant year round transmission. (Infections can occur any time of the year) By adulthood would have achieved full immunity #GrindNation Strength in knowledge Page 4 of 9 Creates a high level of parasitemia and sequestration causing end organ damage. Sequestration is a specific property. Sequestration only seen in falciparum. Sequestration it is the spleen trying to save the uninfected RBCs in the circulation. The spleen will open up to get as much uninfected RBCs into its parenchyma (saving them from being infected). But in the process of sequestering the uninfected RBCs, what is left in the circulation would be less RBCs (because the spleen has already sequestered most uninfected RBCs) Usually seen in the smears are younger forms before sequestration takes place. COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno Sequestration: Contribute to mental changes and coma. End organs affected are: o CNS, lungs and kidneys. A combination of all these results in: o Interference with microcirculatory circulation metabolism especially in the brain and Other things noted in P. falciparum infection: Hypoglycemia This is due to reduction of hepatocytes. Remember that hepatocytes burst during the 1st phase of plasmodium infection. And the hepatocytes are where gluconeogenesis and glycogenesis take place. Lactic acidosis When the RBC burst, it will release acid contributing to lactic acidosis Picture Above: Symptoms of Malaria Severe anemia- CBC, ABG Can be explained by the decrease in RBC volume, either caused by destruction or sequestration of the spleen Multi - organ dysfunction secondary to hypoxia. Usually occurs in travelers without immunity or young children living in endemic areas. You have a rapidly rising fever with severe headache. Just by looking at the pattern of fever, you will already have an idea of what is causing it. If it is low-moderate grade (steady) bacterial If it is high grade (spiking) – from 40-42oC virus or parasite There will also be paroxysms with shaking chills because the patient would have some kind of dehydration already and hyponatremia. There will be profuse sweating after the fever Check for the spleen or liver splenomegaly or hepatomegaly There will also be myalgias (muscle pain) or orthostatic hypotension Typical Manifestations in Diagnosing Malaria Severe anemia – usually associated with P. falciparum infections. May be secondary to RBC infection and a loss of infected RBC. Uninfected RBCs are inappropriately cleared and bone marrow suppression may also be involved Innate Immunity: Depends on the host’s immunity. If we have been exposed to plasmodium during our childhood years it is possible. It is a hard earned immunity because you either DIE as a child or SURVIVE as an adult from it Renal Failure: Infected RBCs adhere to the microvasculature in the renal cortex. Oliguric renal failure ↓ blood sugar Usually reversible. Especially when patient is subjected to immediate dialysis P. falciparum usually results in death. Protective Genetic Factors: Sickle cell disease Hemoglobinopathies Polymorphisms in the host’s Tumor Necrosis Factor (TNF). CLINICAL MANIFESTATIONS Get a history of recent travel in those patients with high grade fever. Most patients will present with fever and (generalized) headache. o There is no neck stiffness or photophobia resembling meningitis. Check for nuchal rigidity to rule out meningitis Malaria free areas: o Aklan, Albay, Batangas, Benguet, Biliran, Bohol, Camiguin, Capiz, Catandauanes, Cavite, Cebu, Eastern Samar, Guimaras, Ilo-Ilo, Leyte, Marinduque, Masbate, Northern Samar, Siquijor, Sorsogon, Southern Leyte, Surigao del Norte, Western Samar Malaria areas in and near NCR: Fairview, Antipolo Malaria is a febrile illness characterized by fever and related symptoms. However, it is very important to remember that malaria is not a simple disease of fever, chills and rigors. In fact, in a malaria prone area, it can present with such varied and dramatic manifestations that malaria may have to be considered as a differential diagnosis for almost all the clinical problems. Malaria is a great imitator and trickster, particularly in areas where it is endemic. #GrindNation Strength in knowledge P. malariae can cause the nephrotic syndrome ↓ albumin levels Respiratory Symptoms: Metabolic acidosis leading to respiratory distress. Can develop pulmonary edema Due to decrease in the oxygen content going to the lungs, the lung would expand pulmonary edema Cerebral Malaria (CNS): Cerebral malaria – almost always due to P. falciparum infections. o Coma lasts more than 30 minutes. o Fever (febrile) seizure coma cascade Page 5 of 9 The brain needs to be highly perfused with blood and glucose. Plasmodium destroy the hepatocytes ↓ in glycogen storage patient may become hypoglycemic brain can go on coma (due to less perfusion & glucose) COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno P. VIVAX & P. OVALE Patient may relapse after long periods because of the hypnozoite stage in the liver. Can remain dormant for months to years before entering the blood stream to produce symptoms. Causes the benign form of tertian fever P. vivax & ovale o (P. malariae causes the quartan fever) Quartan fever means fever on the 1st and 2nd day but no fever on 3rd day o P. falciparum no pattern of fever PHYSICAL EXAMINATION Most patients will have splenomegaly. Test for: o CBC o Anemia o Thrombocytopenia o MARF - adult tubular necrosis secondary to hypovolemia, ischemia, intravascular coagulation o Parameters: <1 ml/kg/hr. Elevated creatinine DIAGNOSTIC PROCEDURE Since Charles Laveran first visualized the malaria parasite in blood in 1880, the main-stay of malaria diagnosis has been the microscopic examination of blood Malarial Smear: In this procedure, a film of blood is placed on a slide, stained, and examined microscopically. Peripheral smear examination for malarial parasite is the goldstandard in confirming the diagnosis of malaria Demonstration of the Parasite Must identify the asexual forms in the peripheral blood smear. Negative smears DO NOT rule out malaria if there is a high degree of suspicion. Repeat. parasite may be residing in the RBCs or in the liver cells Use the Giemsa stains at pH – 7.2 Thick blood smear provides better sensitivity. Thin blood smear provides better specificity and allows better identification of the species involved. Not so diagnostic in P. falciparum infections since sequestration removes the RBCs out of the peripheral circulation especially in the late stages. Hypnozoital (vivax and ovale) Diagnosis: visualization of blood smear Thick and thin smears done 12 to 24 hours apart during the fever The fever pattern of P. falciparum is never regular you will never know when the height of the fever. Before, blood collection is at the peak of fever. Now we do the think & thin smear at any time the patient is febrile THICK SMEAR More sensitive than thin smears. Can’t identify the species Parasitemia can be calculated based on the number of infected RBC. Quantitative test. Can concentrate the parasites increasing diagnostic sensitivity #GrindNation Strength in knowledge Alternative Tests: Quantitative buffy coat – as sensitive as a thick smear but must still do a thin smear. (PfHRP2) Histidine rich protein- 2 (the only approved rapid test in the US. Rapid Diagnostic Test (RDT): o This is a blood test for malaria. It can be conducted outside the laboratory and inside the field. o It gives a result within 10 to 15 minutes. o This is done to detect malarial parasite antigen in the blood. However, it does not detect whether the malarial infection is active or not. It also will not detect the specific kind of specie in the patient’s blood. It will only show if the patient HAD or currently HAVE malaria Additional Information from Old Trans: Diagnosis of malaria rests on the demonstration of asexual forms of the parasite in stained peripheral blood smears Giemsa stain Thick film has advantage of concentrating the parasites and thus increasing diagnostic sensitivity Both parasites and WBC are counted and the number of parasites per unit volume is calculated from the total leukocyte count Before a thick smear is judged as negative, 100-200 fields should be examined under oil immersion In high transmission areas, the presence up to 10,000 parasites/ul maybe tolerated without symptoms or signs in partially immune individuals Rapid simple sensitive and specific antibody based diagnostic stick detect falciparum specific histidine rich protein 2 (pfHRP2) or lactate dehydrogenase antigen Some of the rapid diagnostic test carry a second antibody which falciparum malaria to be distinguished from the less dangerous malaria. PfHRP2 maybe positive for several weeks after acute infection, disadvantage in high transmission areas but is of value in the diagnosis of severe malaria in patients who have taken antimalarial drugs and cleared peripheral parasitemia In general, >105 per ul is at risk of dying but non immune patients may die with much lower counts and partially immune patients may tolerate higher parasitemia levels In severe malaria, poor prognosis is indicated by presence of dominance of more mature P. falciparum (>20% of parasites with visible pigment) in the peripheral blood smear or by the presence of phagocytosed malarial pigment in >5% of neutrophils THIN SMEAR Less sensitive. Facilitate speciation Qualitative test Page 6 of 9 COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno MALARIA SUSPECT Patients with malaria like illness With thrombocytopenia Relative lymphocytopenia Atypical lymphocytes Elevated LDH Anemia Multidrug Resistant P. falciparum & Treatment Failure Ability of the parasite to survive and or multiply despite the administration and absorption of a drug given in the recommended or higher dose but within the limits of tolerance of the patient. Basis: o Recrudescence of asexual parasitemia from 48 hours after treatment If in the 2nd day the patient has still parasites in the blood despite maximum treatment treatment failure OBJECTIVES FOR TREATMENT Treat the malaria Prevent development and spread of antimalarial drug resistance 3 medical conditions associated with Plasmodium infection: 1. Uncomplicated 2. Treatment failure 3. Severe malaria Uncomplicated Malaria Febrile Parasites in blood Absence of severe malaria and multi drug resistant P. falciparum Severe headache, chills Thrombocytopenia For P. falciparum & vivax o Day 0 – 2 Co-Artem (Lumefantrine + Artemisinine) Given after high fat meals Contraindicated in pregnancy and lactation o Day 3 Primaquine falciparum – gametocidal vivax – hypnozoiticidal Discharged if asexual forms are not seen in Day 7 then monitor once a week for a month. How to Assess: Day 0, 3,7 do blood smear, if parasite not seen in day 7 it means the patient is getting well. If still present, label as treatment failure #GrindNation Strength in knowledge Other Plasmodium parasites and mixed infections: o P. malariae Chloroquine Primaquine Page 7 of 9 o No parasite clearance or reduction Despite of management of Co-Artem and Primaquine, on the 7th day the parasites are still there treatment failure Objectives: o Cure the infection o Prevent the development of severe malaria o Prevent spread of drug resistant forms of the parasite Severe Malaria Dysfunction of organ systems secondary to: o Effects of malaria toxins o Sequestration of infected RBC o Anemia Abnormal organ function tests Jaundice Hyperparasitemia (>2% parasitized RBC) Severe anemia Metabolic abnormalities Hemoglobinuria COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno o Severe malaria continued….. Conditions of a person with severe malaria: o Seizures Due to brain hypoxygenation & hypoglycemia o o o o o o o Artemisinin Approved in 2009. Cannot be used as monotherapy because of a high rate of resistance. Due to only a temporary stop in the growth of ring stage parasites (dormant forms) after exposure to artemisinin. Impaired consciousness Prostration/ weakness Poor urine output Signs of pulmonary edema Signs of DIC – already going into sepsis septic shock Abnormal spontaneous bleeding Chloroquine Phosphate Can be used for prophylaxis and treatment. Drug of choice for chloroquine sensitive malaria. Treatment of Severe Malaria: o US FDA and WHO: Artesunate IV o DOH: may give Co-Artem Quinine IV or Artesunate IV plus treatment: Quinine or artesunate + tetracycline + clindamycin Quinine Note: Tetracycline is not available in the market today due to its notorious side effect of yellowish discoloration of teeth (especially in children) So in severe malaria we give: Co-Artem + Quinine/Artesunate + Clindamycin Mefloquine Use of mefloquine for pregnant women in the second and third trimester is sanctioned by the WHO and the CDC allow the use of mefloquine even in the first trimester of pregnancy. Day 0 – 2 Chloroquine o No treatment failure reported yet Days 3 – 17 Primaquine Treatment Failure Falciparum malaria - Quinine and any of the three drugs: doxycycline, tetracycline, clindamycin (QUININE PLUS) Vivax – Co-Artem o If hypnozoites are suspected and fever recurs after 2 weeks Primaquine Primaquine Prevents drug resistant falciparum and vivax malaria in adults Contraindicated in pregnant patients or new born babies (x) G6PD deficiency hemolysis death Treatment Under Special Conditions Pregnant women: o Falciparum – oral quinine Insulin secreting drug monitor blood sugar levels Do not give Co-Artem o Vivax - chloroquine TREATMENT P. falciparum – resistant to chloroquine. P. vivax – not so resistant to chloroquine. P. ovale and P. malariae – sensitive to chloroquine. Primaquine - needed to treat the hypnozoites (liver phase). Artesunate IV anti – malarial now used in the US for severe complicated malaria. Reduced mortality among children in African countries compared with quinine. Patients have less symptoms of coma, seizures, post – treatment hypoglycemia. Water soluble derivative from artemisinin. Drug of choice for severe falciparum malaria. Recommendations for malaria treatment: #GrindNation Strength in knowledge No role in prophylaxis Used with second agent in drug – resistant falciparum infections. Used in pregnant women Fansidar Pyrimethamine –sulfadoxine. Can also be used for treatment . Not anymore considered as a first line drug for prophylaxis because of adverse drug reactions. Falciparum + either vivax or malariae Co-Artem (falciparum) and Primaquine (vivax) P. vivax P. falciparum malaria: Quinine plus doxycycline or clindamycin or pyrimethamine – sulfadoxine. Alternative treatment: Artemether – lumefantrine, or mefloquine Page 8 of 9 SUPPORTIVE MANAGEMENT Cerebral malaria o Unarousable coma not attributed to any other cause and persists for > 30 minutes after a seizure o Treatment: fluid balance, hyperpyexia, control seizures o No mannitol, osmotic diuretics, steroids o Put ice bag on the head (brain cannot be subject to ↑ temperature) Pulmonary edema o Increased pulmonary capillary permeability Hypoglycemia Circulatory collapse/ shock: o Do not give dopamine, dobutamine, epinephrine o Give norepinephrine (dilate BV without affecting the patient’s heart) COMMUNICABLE DISEASES (IM) Topic: Malaria Lecture by: Dr. Fortuno BASIS FOR CHEMOPROPHYLAXIS Each species has a specific incubation period. P. falciparum infection typically develops within a month of exposure. Rare cases have been reported up to a year later. Hypnozoite form – P. vivax and P. ovale. o Parasite stays in the liver for months before inducing initial infection. Chemoprophylaxis: Doxycycline 100 mg daily for 2 – 3 days before going to an endemic area, continue while in the endemic area and continue for 4 more weeks after leaving the endemic area Lecture Discussion: Why do you have to take it for 1 more month (4 weeks) even if you already left the endemic area? It’s because you might have harbored the hypnozoites in the endemic area we are trying to kill it so you have to take it for 1 more month PERSONAL PROTECTION Reduce the frequency of mosquito bites. o Avoid the mosquito’s peak feeding hours. o DEET containing lotions (e.g., off lotion) and picaridin DEET has no teratogenic effect safe for pregnants o Insecticide impregnated mosquito nets. PREVENTION AND CONTROL Malaria case should be reported. A thorough screening of all infected person’s from mosquitoes is important. Mosquito breeding places must be destroyed. Homes should be sprayed with effective insecticides which have residual actions on the wall. Mosquito nets should be used especially when in infected areas. Insecticide Treated Bed Nets (ITN’s) have emerged as a very important tool in malaria control in endemic areas. Insect repellents must be applied to the exposed portion of the body. o Permethrin o DEET (N,N-diethyl-m-toluamide) o IR3535 (3-[N-acetyl-N-butyl]-aminopropionic acid ethyl ester) o Bayrepel (1-piperidinecarboxylic acid, 2-(2hydroxyethyl)-, 1-methylpropylester) Blood donors should be properly screened. MALARIA SITUATION IN THE PHILIPPINES Malaria is a rural disease one of the important mosquito-borne diseases affecting far-flung barangays of the country Out of the 79 provinces nationwide, 57 are malaria endemic Malaria Control Program: Vision: malaria-free Philippines by 2020 Strategies: 1. Early diagnosis and prompt treatment 2. Vector control – insecticide-treated mosquito net as main vector control strategy, complemented by indoor residual spraying 3. Early management and disease surveillance 4. Monitoring and evaluation #GrindNation Strength in knowledge Page 9 of 9