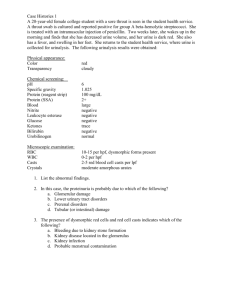
Body Fluid Analysis: Clinical Chemistry Lecture Notes
advertisement

DIAGNOSTIC IN CLINICAL CHEMISTRY I MKEB 2404 EXAMINATION OF BODY FLUIDS Type of body fluids: Urine Seminal fluid Amniotic fluid Cerebrospinal fluid Synovial fluids Pleural, pericardial and peritoneal fluid Fecal analysis First morning urine collection: Voids before going to bed Formed elements are more stable Unsuitable for cytology studies Collection of midstream urine for avoid contamination (let the first urine throw first and only take the middle urine) Urine container: Wide mouth (4 - 5 cm) Sufficient volume (50 ml preferred) Glass or plastic with no additives Leak-proof Sterile, if specimen is stored for a period of time before testing The importance of urinalysis: as an indicator of health or disease, especially with metabolic and renal disorders Potential changes in unpreserved urine: Physical changes Bilirubin - biliverdin Color Hemoglobin - methemoglobin Urobilinogen - urobilin Clarity Decreased due to bacterial proliferation,solute precipitation Odour Increased due to bacterial proliferation and decomposition Chemical changes pH Increased or decreased 1|Page Glucose Ketones Bilirubin Urobilinogen Nitrite RBC, WBC, casts Bacteria Others decreased decreased decreased decreased Increased or decreased Microscopic changes Decreased due to disintegration especially in alkaline urine RBC decreased after 6 hours WBC decreased 50% within 3 hours Hyaline and granular casts decreased after 2 hours Increased due to bacterial proliferation Precipitation of uric acid, calcium phosphate and calcium oxalate Yeast cells develop pseudo-mycelia Spermatozoa become immobile Trichomonas become immobile, maybe counted as WBC Contamination by air borne particles Urine examination: Most preservatives prevent bacterial growth and loss of glucose (eg. Stabilur, formalin) No preservatives can prevent destruction of bilirubin, urobilinogen or occult blood. Use of preservatives may increase SG, minor effects on pH and may inhibit leukocyte esterase reaction. No single urine preservative is available Urine FEME: Color Physical examination Urochrome, urobilin, uroerythrin Normal color range from straw, pale yellow, to amber. Abnormal color: Red - RBCs Beer-brown - bilirubin Orange, blue, green - drug, dye or food Colorless - dilute urine - fluid ingestion: polyuria Light yellow and yellow - normal Urine Amber - concentrated urine - dehydration, fever Amber – urobilin - no yellow foam Dark amber – bilirubin - yellow foam Dark amber – biliverdin - imparts green blue 2|Page Orange – bilirubin - yellow foam if sufficient bilirubin Orange – urobilin - no yellow foam Orange – medication Red - hemoglobin, red blood cell Red – myoglobin - muscle injury Red - porphyrins Red – beets - genetic Red - fuscin, analine dye - food, candy Pink – hemoglobin, porphyrins Brown – hemoglobin, myoglobin, methemoglobin (muscle), homogentisic acid (acid pH), melanin Black – melanin (upon standing), homogentisic acid (upon standing : alkaline urine) Green blue – indican (infections of small intestines), chlorophyl (breath deodorizers), pseudomonas infection, dyes and medication Color changes due to oxidation: RBC oxidizers (brown) → methemoglobin (black) Urobilinogen (colorless) → urobilin (orange – brown) Porphobilinogen (colorless) → oxidizers to porphobilin (red / purple) Bilirubin (amber) → oxdizers to biliverdin (greenish) Urine color changes with commonly used drugs: Alcohol, ethyl – pale, diuresis Anthraquinone laxatives – reddish – alkalinr, yellow brown – acid Chlorzoxazone (muscle relaxant) – red Deferoxamine mesylate (desferal) – red Furazolidone (an antibacterial, anti protozoal pitrofuran) – brown Indigo carmine dye (renal function, cytoscopy) – blue Iron sorbital (jectofer) – brown on standing Leyodona (parkinsonism) – red then brown, alkaline Alcohol – pale Desferal and paraflex (muscle relaxant) – red L – Dopa (parkinsonism) – red then brown Flagyl – reddish brown Nitrofurantoin – brown – yellow Riboflavin – bright - yellow Clear, slightly cloudy, cloudy, turbid Turbidity or cloudy urine: Amorphous salts – non pathologic Bacteria, blood cells - pathologic Clarity and Odour 3|Page Causes of turbidity (pathologic): RBC, WBC Bacteria, yeast, trichomonas Renal epithelial cells Fat (lipids, chy;e) Abnormal crystals, calculi and pus Causes of turbidity non pathologic: Normal crystals like urates and phosphates Radiographic media Mucus, mucin, squamous epithelial cells Sperm, posthatic fluid Salves, lotions, cream Powders, talc Chemical examination Volume - average of 1.0 to 1.5L of urine excreted per day Amount excreted is an indicator for diuretic disorder Urinalysis Polyuria: More than 2000ml urine/day Oliguria: Less than 500ml urine/day Anuria : Less than 200ml urine/day Dysuria: No urinary excretion Example is Bayer – ames multistix Manual – subjective Dipstick Machine – standardized reflectance photometer that methods measures scattered or reflected light, have multiple channels and compensator pad Store in original container Dipstick Do not expose to light, heat and moisture methods – care If there is any colour change, discard and storage Do not use pass expiration date. Store at manufacturer recommended temperatures Well-mixed uncentrifuged urine sample Dip strip into urine briefly Dipstick – testing Remove excess urine procedure Read colour development according to manufacturer’s (manual) instruction Read in a well lit area Aware of false positive and false negative results Reaction: Pseudoperoxidase action of Hgb myoglobin catalyzes Blood the oxidation of chromogens to produce a color change False negatives: 4|Page Formalin, excess nitrites (2.2 mmol/l), elevated SG, ph <5.1, captopril, ascorbic acid False positive: Oxidizing detergents, microbial peroxidase (UTI), dehydration, exercise, hemoglobinuria, myoglobinuria, menstrual contaminants, proteinuria (5 g/l) Hematuria: Presence of an abnormal number of blood cells in urine as microhematuria or gross hematuria (0.5ml or 2500 RBC/µl) Occurs with disease or trauma anywhere in the kidneys or urinary tract Can be seen in healthy persons undertaking excessive exercise (marathon runners) in whom bleeding emanates from the bladder mucosa. Repeat urinalysis after 48 – 72 hours should be negative Causes: cancer, trauma, stones, infections, obstructions, viral infections, inflammation of kidneys, benign prostate enlargement, and warfarin therapy Calculi – ca oxalate (60%), uric acid (25%) phosphate (20%) Tumors – painless hematuria Glomerulonephritis – hematuria with proteinuria Urinary tract infection Separate sales: Green dots (intact RBC) Homogenous green color scale (for lysed RBC) Reaction: Bilirubin in the urine couples with a diazonium salt in an acid medium False negative: Samples exposed to light, excess levels of ascorbic acid.and nitrite, selenium, chlorpromazine False positives: Highly colored metabolites of drugs eg pyridium _____________________________________________________ Breakdown product of hemoglobin formed in the in the RES, liver, and bone marrow carried in the blood by protein Normal adult urine contains 1 mg/dL and this is not detected by usual tests. Reaction: Bilirubin Glucose 5|Page Double sequential enzyme reaction of glucose oxidase and peroxidase-reacts with a chromogen to produce the final color. False negative: Elevated specific gravity, uric acid, ascorbic acid False positives: presence of oxidizing agents, ketones, levodopa _____________________________________________________ May appear in the urine and is influenced by: o Blood glucose levels o Glomerular blood flow o Tubular reabsorption rate Often regarded as a hallmark of disease and requires a patient to receive a workup for diabetes mellitus. Reaction (Legal or rpthera’s test): Reaction with nitroprusside or sodium nitroferricyanide and glycine to produce a color change. -hydroxybutyerate 78%, acetoacetate 20%,acetone 2% False negative: Delay in examination False positives: Highly pigmented urines; some drug metabolites, acidic urine, elevated SG _____________________________________________________ Products of incomplete fat metabolism Presence is indicative of acidosis Low carbohydrate diet for weight reduction will produce ketonuria Exposure to cold and severe exercise Reaction : Leukocyte esterase, present in granulocytes, catalyzes the reaction of the chromogens to produce a color change. False negative: Cephalexin and gentamicin concentrations; elevated SG, glucose, ketone and protein concentrations, ascobic acid False positives: Vaginal contaminants, drugs or foods that color the urine red Reaction : Nitrates in the urine are converted to nitrites by the Ketones Leukocytes Nitrites 6|Page pH Protein action of gram-negative bacteria. These nitrites then react to form a diazonium salt which in turn reacts with a chromogen to produce the final color. False negative: Elevated SG, urobilinogen, pH <6.0, excess ascorbic acid False positives: Presence of red dyes or other chromogens, contamination Reaction: Double indicator system detects the amount of hydrogen ions in the urine to produce a color change. Interferences: If excess urine is left on the reagent strip, a phenomenon known as “runover” may occur. The urine from one reagent area carries reagent onto the pH test area and changes the result erroneously. Reflection of the ability of the kidney to maintain normal hydrogen ion concentration in plasma and extracellular fluid Normal adult: 4.6 - 8.0 pH o Hypertonic urine < 6.0 - crenated RBC o Hypotonic urine > 7.5 - Lysis of cells Acid urine: diet high in meat protein Alkaline urine: diet high in citrate or vegetables RTA type I (renal tubular acidosis) o Serum is acidic, urine is alkaline RTA type II o Urine initailly alkaline but becomes more acidic due to decrease in bicarbonate load Useful in diagnosis and management of UTI and calculi o Alkaline urine in UTI suggests presence of urea-splitting organisms o Magnesium-ammonium phosphate crystals can form staghorn calculi o Uric acid calculi associated with acidic urine Reaction : Based on “protein error of indicators” - because protein carries a charge at physiologic pH, their presence will elicit a pH change False negative: Acidic or diluted urine, primary protein is not 7|Page albumin False positives: Alkaline or concentrated urine, quaternary ammonia compounds High levels in urine indicates renal disease: o Glomerular disease o Tubular disease Functional proteinuria o After strenuous exercise Other methods of detection: Heat Acid (SSA- sulfosalicylic acid precipitation test) Sensitivity: 5-10 mg/dL of protein Reaction : ionic specific gravity Based on the change of an indicator color in the presence of high concentrations of various ions. False negative: Highly alkaline urine False positives: Proteinuria, Dextran solutions,IV radiopaque dyes, Specific gravity Urobilinogen Random SG - 1.015 - 1.025 SG< 1.010 indicates relative hydration SG > 1.020 indicates relative dehydration SG - 1.000 should be checked SG - 1.040 physiologically impossible Other methods: urinometer and refractometer Correlates with urine osmolality Insight to patient’s hydration status Reflects concentration ability of the kidneys Reaction : ionic specific gravity Urobilinogen reacts with a chromogen to form an azo dye which appears as various shades of pink or purple. False negative: Excess nitrites; presence of formalin False positives: Presence phenazopyridine; very warm urine, elevated nitrite levels Elevated urobilinogen found in hemolysis and hepatocellular diseases 8|Page Test strip sieve technique Sediment examination Microscopic components in urine sediment Methods for examining urine sediment Red blood cells Dysmorphic RBCs Leukocytes Decrese robilinogen levels can be due to antibiotic use and bile duct obstruction Leucocyte RBC Protein Nitrite pH 7.0 Microscopic examination Most common laboratory procedure utilized for the detection of renal and/or urinary tract disease Numerous morphologic entities o Blood cells, epithelial cells, organisms Correlate with the biochemical results o Dipsticks o Clinical condition of the patient Cells o Blood cells; RBCs and WBCs o Epithelial cells; renal, transitional, squamous Casts o Hyaline o Waxy o Inclusion casts; Granular, Fatty o Cellular; RBC, WBC, and Epithelial casts Bacteria, Fungi, and Parasites Crystals Bright field Microscopy of unstained urine and w/ Supravital staining Phase Contrast Microscopy Polarized Microscopy Interference Contrast Microscopy Cytodiagnostic Urinalysis Quantitative and Differential Counts Appear as pale discs Can be confused with yeast cells Yeast cells do not stain and are not lysed by the addition of acetic acid Increased numbers in conjunction with RBC cast bleeding assumed to be renal in origin Absence of casts and protein - bleeding assumed to be non-renal Increased numbers are seen: o Renal diseases o Urinary tract infection 9|Page Squamous epithelial cells Transitional epithelial cells Renal tubular epithelial cells Casts Hyaline cast Waxy cast Granular casts Fatty casts When accompanied by casts: o Renal in origin Line the distal 1/3 of the urethra Large numbers in women maybe a source of contamination Line the urinary tract from the renal pelvis to the proximal 2/3 of the urethra few are present in normal urine Small numbers maybe seen in normal urine o Sloughing of aging cells Increased numbers are seen: o Acute tubular necrosis o Certain drug or heavy metal toxicity Formed when an increased numbers of proteins enter the tubules. Formation increases with: o Lower pH o Increased ionic concentration Tamm-Horsfall (TH) protein forms the matrix of all casts o Glycoprotein secreted by cells in the ascending loop of Henle If cast contain 3 or more cells e.g. RBC, WBC, then it is RBC cast, WBC cast If it contains 1/3 or more granules - granular cast If a cast is about 60 µm or more - broad cast, RBC 7-8 µm, WBC 8-22 µm Translucent with brightfield microscopy Increased numbers: o Pyelonephritis, chronic renal disease o Transiently with exercise o May be a normal finding Associated with tubular inflammation and degeneration Observed frequently with chronic renal failure Appear with glomerular and tubular diseases Accompany: o Pyelonephritis o Viral infections o Chronic lead poisoning Commonly seen when there is heavy proteinuria A feature of nephrotic syndrome Hypothyroidism 10 | P a g e Diagnostic of glomerular disease Glomerular damage allows RBCs to escape into the tubules WBCs enter the tubular lumen through and between White blood cells tubular epithelial cells casts Associated with pyelonephritis and tubulointerstitial disease To differentiate from leukocyte cast, supravital Epithelial cells staining and phase -contrast microscopy are helpful. casts Associated with: tubular necrosis, viral disease (CMV), heavy metal ingestion Other component that also found is bacteria, fungi, and parasites and also clue cells Limited clinical significance Phosphates, urates, and oxalates are common and occur in normal urine Alkalization and refrigeration promotes crystals formation Few crystals are important: Crystals o Cystine o Tyrosine o Leucine o Bilirubin - hepatic and biliary tract diseases o Cholesterol - nephrotic syndrome Cysteine, leucine and tyrosine is due to inherited metabolic disorders Amorphous urates / phosphates Crystals found in Calcium oxalates normal urine Uric acid Triple phosphates Cysteine Crystals found in Bilirubin abnormal urine Tyrosine Cholesterol Procedure for Sample collection → centrifugation → decantation → slide urine microscopy preparation → microscopy → writing report Centrifuge or not to centrifuge: “After a 5 min centrifugation of the urine at 3500rpm, only 48% Quantitative ME of RBC and 40% of WBC found to be present could still be detected (microscopic under the microscope” examination) To report in µl or LPF or HPF To stain or not to stain Neubauer See picture below: Red blood cells casts 11 | P a g e counting chamber Analysis volume of Neubauer is half of Fuch Rosenthal o Concentration of urine formed elements is very Fuch Rosenthal low compared with those of hematology. vs Neubauer for o For urinalysis, the more volume, the better quantitatve urine results microscopy: Some urine formed elements are large (ie casts), these Advantages of might clog the chamber Fuch Rosenthal o The deeper the depth, the better over Neubauser: Cells /uL = total cells counted / [mm2 counted (how many mm squares were conted) x 0.1 mm (neubauer chamber) or 0.2mm (fuch rosenthal chamber)] Depends on: Real View ( Diameter ) Magnification# ( x10 or x40 ) HPF LPF or µl Original Urine Volume before Centrifugation conversion Sediment Volume after Centrifugation Loaded Sediment Volume on the Slide Area of Cover Slip Low power microscopy: Ensure uniform distribution of urine sediment If uneven distribution, make a new preparation Reduce light intensity Scan whole area. Note: sediments tend to gather along sides of cover-slip Procedure for High power microscopy: microscopic Examine 20 - 30 fields (optimal) but not less than 10 examination fields Microscopic with staining sediment to stain 4:1 Types of stain: 1. Sternheimer-Malbin Stain (SM Stain) 2. Sterheimer Stain (S Stain) 3. 0.5% Toluidine Blue 4. Sudan III and Oil Red O Blood cells: Less than 1cell/HPF Procedure for 1 - 4 cells/HPF microscopic 5 - 9 cells/HPF examination 10 - 19 cells/HPF reporting format: 20 - 29 cells/HPF 30 - 49 cells/HPF 12 | P a g e Casts: + ++ +++ ++++ 50 - 99 cells/HPF Numerous -100 cells and more :0 : 1 cast/100LPF : 1 cast/LPF : 10 casts/LPF : 100 casts/LPF or 1 cast/WF or 100 casts/WF or 1,000 casts/WF or 10,000 casts/WF or 6 casts/HPF Bacteria and yeast: :0 +/- : scatter in several fields + : seen in each foeld ++ : many or scatter in cluster +++ : numerous Crystals and amorphous materials: :0 + : 1 ~ 4/HPF ++ : 5 ~ 9/HPF +++: 10 ~ /HPF 3 mm 1 mm W W W W 13 | P a g e