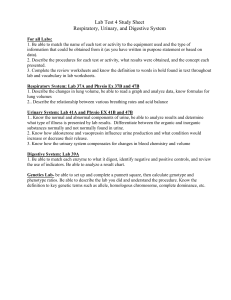
Chapter 06: Values, Ethics, and Advocacy Advocacy--protection and support of another's rights Autonomy--self-determination; being independent and self-governing Beneficence--principle of doing good care-based approach--approach to bioethics that directs attention to the specific situations of individual patients viewed within the context of their life narrative code of ethics--principles that reflect the primary goals, values, & obligations of the profession Conscientious objection--the refusal to participate in certain types of treatment and care based on the fact that these activities violate the nurse’s personal and professional ethical beliefs and standards. ethics--systematic inquiry into principles of right and wrong conduct, virtue & vice, and good & evil as they relate to conduct ethical dilemma--situation that arises when attempted adherence to basic ethical principles results in two conflicting courses of action feminist ethics--type of ethical approach that aims to critique existing patterns of oppression and domination in society, especially as these affect women and the poor fidelity--keeping promises and commitments made to others justice--process that distributes benefits, risks, and costs fairly morals--like ethics, concerned with what constitutes right and wrong; more informal and personal than ethics Moral agency--the capacity to be ethical and to do the ethically right thing for the right reasons. Moral distress--occurs when you know the right thing to do, but either personal or institutional factors make it difficult to follow the correct course of action. moral injury--occurring when there has been: (1) a betrayal of what is right, (2) by someone who holds legitimate authority or by oneself, (3) in a high-stakes situation Moral resilience is the developed capacity to respond well to morally distressing experiences and to emerge strong. nonmaleficence--principle of avoiding evil nursing ethics--a subset of bioethics; formal study of ethical issues that arise in the practice of nursing and of the analysis used by nurses to make ethical judgments principle-based approach--a approach to bioethics that offers specific action guides value--beliefs that are meaningful in life and that influence relationships with others value system--organization of values ranked among a continuum of importance values clarification--process by which people come to understand their own values and value system Virtues--are human excellences, cultivated dispositions of character and conduct that motivate and enable us to be good human beings. Chapter 07: Legal Dimensions of Nursing Practice Accreditation--process by which an educational program is evaluated and then recognized as having met certain predetermined standards of education Assault--threat or attempt to make bodily contact with another person without that person's permission Battery--assault that is carried out Certification--process by which a person who has met certain criteria established by a nongovernmental association is granted recognition common law--law resulting from court decisions that is then followed when other cases involving similar circumstances and facts arise; common law is as binding as civil law credentialing--general term that refers to ways in which professional competence is maintained Crime--offense against people or property; the act is considered to be against the government, referred to in a lawsuit as "the people," and the accused is prosecuted by the state defamation of character--an intentional tort in which one party makes derogatory remarks about another that diminishes the other party's reputation defendant--the one being accused of a crime or tort expert witness--nurse who explains to the judge and jury what happened based on patient's record and who offers an opinion as to whether the nursing care met acceptable standards of practice fact witness--nurse who has knowledge of the actual incident prompting a legal case; bases testimony on firsthand knowledge of the incident and not on assumptions felony--crime punishable by imprisonment in a state or federal penitentiary for more than one year; crime of greater offense than a misdemeanor fraud--willful and purposeful misrepresentation that could cause, or has caused, loss or harm to people or property incident report--also called a variance or occurrence report, is used by health care facilities to document the occurrence of anything out of the ordinary that results in, or has the potential to result in, harm to a patient, employee, or visitor law--a standard or rule of conduct established and enforced by the government that is intended chiefly to protect the rights of the public. liability--legal responsibility for one's acts (and failure to act); includes responsibility for financial restitution of harms resulting from negligent acts licensure--to be given a license to practice nursing in a state or province after successfully meeting requirements litigation--process of lawsuit malpractice--act of negligence as applied to a professional person such as a physician, nurse, or dentist misdemeanor--crime of lesser offense than a felony and punishable by fines, imprisonment (usually less than a year), or both negligence--performing an act that a reasonably prudent person under similar circumstances would not do, or failing to perform an act that a reasonably prudent person under similar circumstances would do nurse practice act--protects the public by broadly defining the legal scope of nursing practice. plaintiff--person or government bringing a lawsuit against another Root cause analysis--involves digging progressively deeper into the event, repeatedly asking why the event occurred, and exploring the circumstances that led to it to determine where improvements can be made. Nurses play a critical role in responding to sentinel events. sentinel event--an unexpected occurrence involving death or serious physical or psychological injury, or the risk thereof statutory law--law enacted by a legislative body tort--wrong committed by a person against another person or his property whistle-blowing--term generally used to refer to employees who report their employers' violations of the law to appropriate enforcement agencies outside the employers' facilities Chapter 34: Activity Ergonomics is the practice of designing equipment and work tasks to conform to the capability of the worker and provides a means for adjusting the work environment and work practices to prevent injuries. safe patient handling and mobility (SPHM)--Ergonomics applied to activities associated with direct patient care. It is very important to incorporate safe patient handling and mobility interventions into nursing practice and patient care. Orthopedics --the correction or prevention of disorders of body structures used in locomotion. Tonus--the state of slight contraction—the usual state of skeletal muscles. Contractures--permanent contraction of a muscle The patient’s ability to move purposefully to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs) or self-care activities, and maintain their quality of life. Eating, bathing, dressing, and toileting are examples of ADLs. Housekeeping, meal preparation, management of finances, and transportation are examples of IADLs. Types of Exercise Exercise can be divided into two major types. One is based on the type of muscle contraction occurring during the exercise. The second is based on the type of body movement occurring and the health benefits achieved. Muscle Contraction--Exercise may be categorized according to the type of muscle contraction involved as being isotonic, isometric, or isokinetic Isotonic exercise involves muscle shortening and active movement. Examples include carrying out ADLs, independently performing range-of-motion exercises, and swimming, walking, jogging, and bicycling. Isometric exercise involves muscle contraction without shortening (i.e., there is no movement or only a minimum shortening of muscle fibers). Examples include contractions of the quadriceps and gluteal muscles, such as what occurs when holding a yoga pose. Isokinetic exercise involves muscle contractions with resistance. The resistance is provided at a constant rate by an external device, which has a capacity for variable resistance. Examples include rehabilitative exercises for knee and elbow injuries and lifting weights. range of motion--the maximum degree of movement of which a joint is normally capable. Body Movement--Exercise activities may also be categorized according to the type of body movement involved and the health benefits they produce. Types of exercise involving body movement include aerobic exercises, stretching exercises, strength and endurance exercises, and movement and ADLs. Aerobic exercise refers to sustained (often rhythmic) muscle movements that increase blood flow, heart rate, and metabolic demand for oxygen over time, promoting cardiovascular conditioning. Examples of aerobic activities include swimming, walking, jogging, cross-country skiing, aerobic dancing, bicycling, jumping rope, and racquetball. Stretching exercise involves movements that allow muscles and joints to be stretched gently through their full range of motion, increasing flexibility. Specific warm-up and cool-down exercises, Hatha yoga, and some forms of dance are examples. Strength and endurance exercises are components of a variety of muscle-building programs. Weight training, calisthenics, and specific isometric exercises can build both strength and endurance, increasing the power of the musculoskeletal system, and generally improving the whole body. Atrophy--decreased muscle size Flaccidity--Decreased tone, also known as hypotonicity, results from disuse or neurologic impairments and is described as a weakness of the involved area. Spasticity or hypertonicity, increased tone that interferes with movement, is also caused by neurologic impairments and is often described as a stiffness, tightness, or pulling of the muscle. Paresis--Impaired muscle strength or weakness. Paralysis--The absence of strength secondary to nervous impairment. Footdrop--In this position, the foot is unable to maintain itself in the perpendicular position, heel–toe gait is impossible, and the patient experiences extreme difficulty in walking. Need the use of a foot support. active exercise--the patient independently moves joints through their full range of motion (isotonic exercise). active-assistive exercise, the nurse may provide minimal support and assistance if the patient cannot do the exercise independently. passive exercise--the patient is unable to move independently, and the nurse moves the joint through its range of motion. Fracture--a complete or incomplete disruption in the continuity of the bone structure. Chapter 38 Urinary Elimination Urination, micturition, or voiding (void)--the process of emptying the bladder. Urine--the waste product excreted by the kidneys, contains organic, inorganic, and liquid wastes. autonomic bladder--bladders are no longer controlled by the brain because of injury or disease also void by reflex only. urinary incontinence—any involuntary loss of urine. Urinary retention--urine is produced normally but is not excreted completely from the bladder. Enuresis--Continued incontinence of urine past the age of toilet training. Nocturnal enuresis (nighttime bedwetting) usually subsides by age 6 years. Nocturia--the need to wake up at night in order to urinate. urge incontinence--the involuntary loss of urine that occurs soon after feeling an urgent need to void. Sedatives and tranquilizers may diminish awareness of the need to void. urinary tract infection (UTI)-- an infection in any part of the urinary system. The urinary system includes the kidneys, ureters, bladder and urethra. Most infections involve the lower urinary tract — the bladder and the urethra. Nephrotoxic--capable of causing kidney damage. Hematuria--blood in the urine. continent of urine—patients who have self-control over urination are continent of urine. Incontinent--Urinary incontinence is the involuntary or uncontrolled loss of urine from the bladder. Patients who experience involuntary or uncontrolled loss of urine are incontinent. Stoma--a surgically created opening on the body surface. TYPES OF URINARY INCONTINENCE Transient incontinence appears suddenly and is usually caused by an illness or temporary problem that is short-lived or treatable. Stress incontinence--occurs because of weak pelvic floor muscles and/or a deficient urethral sphincter, causing an involuntary loss of urine related to an increase in intra-abdominal pressure. This commonly occurs during coughing, sneezing, laughing, lifting, changing position, or exercising. Mixed incontinence is a combination of stress incontinence and urgency incontinence and is marked by involuntary leakage associated with urgency as well as with exertion, effort, sneezing, and coughing. Overflow incontinence, or chronic retention of urine, is the involuntary loss of urine associated with overdistention and overflow of the bladder. Functional incontinence is urine loss caused by the inability to reach the toilet because of environmental barriers, physical limitations, loss of memory, or disorientation. reflex incontinence--emptying of the bladder without the sensation of the need to void from damage to the nerves that normally signal the brain that the bladder is filling. Cause--Spinal cord injuries, multiple sclerosis or damage from surgery or radiation treatment. Total (continuous) incontinence is a continuous and unpredictable loss of urine, resulting from surgery, trauma, or physical malformation such as a urogenital fistula. Urination cannot be controlled. postvoid residual (PVR) urine--the amount of urine remaining in the bladder immediately after voiding. incontinence-associated dermatitis (IAD)-- inflammation of the skin--Excessive contact of the skin with urine or feces leads to a form of moisture-associated skin damage. condom-type urinary sheath, one type of external urine collection device for use on the penis. TYPES OF CATHETERS Intermittent urethral catheters, or straight catheters--are used to drain the bladder for short periods. Indwelling catheters--also called retention or Foley catheters--catheter is to remain in place for continuous drainage. suprapubic catheter--an indwelling urinary catheter used for long-term continuous drainage. This type of catheter is inserted surgically through a small incision above the pubic area. Bacteriuria--bacteria are present in the urine. Urinary Diversion--Obstructions or tumors in the urinary tract may require some patients to have urinary flow diverted surgically. ileal conduit (also known as a urostomy) is the most common type of incontinent cutaneous urinary diversion. An ileal conduit involves a surgical resection of the small intestine, with transplantation of the ureters to the isolated segment of small bowel. This separated section of the small intestine is then brought to the abdominal wall, where urine is excreted through a stoma, a surgically created opening on the body surface. Cutaneous ureterostomy is another type of incontinent cutaneous urinary diversion in which the ureters are directed through the abdominal wall and attached to an opening in the skin. These cutaneous diversions are usually permanent, and the patient wears an external appliance to collect the urine because elimination of the urine from the stoma cannot be controlled voluntarily. continent urinary diversion (CUD)--the ureters are diverted into a segment of ileum and cecum in an Indiana pouch. This is a surgical alternative that uses a section of the intestine to create an internal reservoir that holds urine, with the creation of a catheterizable stoma. The external stoma or outlet must be catheterized at regular intervals to drain the urine that has collected in this reservoir. Fenestrated-- having one or more openings or pores. Urine specific gravity (USG or UG) is the measure of the density of the urine solute compared to free water. Pubic symphysis--a joint sandwiched between your left pelvic bone and your right pelvic bone. It helps your pelvis absorb some of the weight from your upper body before it travels to your lower body. Chapter 39: Bowel Elimination Anus--the outlet of the GI tract. Feces--solid waste products that have reached the distal end of the colon and are ready for excretion. The sigmoid colon contains feces, Stool--Once excreted, feces are called stool. Hemorrhoids--The rectum is about 5 inches (12 cm) and includes the anal canal. In the rectum, three transverse folds of tissue are present that may help to hold the fecal material in the rectum temporarily. Vertical folds also are present, each of which contains an artery and a vein. If the veins become abnormally distended, hemorrhoids occur. Defecation--the process of bowel elimination; a bowel movement Peristalsis--Contractions of the circular and longitudinal muscles of the intestine, move waste products along the length of the intestine continuously. Flatus--intestinal gas. Valsalva maneuver--When a person bears down to defecate, the increased pressures in the abdominal and thoracic cavities result in decreased blood flow to the atria and ventricles, thus temporarily lowering cardiac output. Once bearing down ceases, the pressure is lessened, and a larger-than-normal amount of blood returns to the heart. This act may cause the heart rate to slow (vagal response) and result in syncope in some patients. Therefore, this action of bearing down, termed the Valsalva maneuver, may be contraindicated in people with cardiovascular problems and other illnesses. Diarrhea--an increase in frequency, and/or a change in consistency of stools. Constipation--dry,hard stool; infrequent difficult passage of stool; and/or the incomplete passage of stool. fecal impaction—prolonged retention or an accumulation of fecal material that forms a hardened mass in the rectum. Fecal incontinence--involuntary or inappropriate passing of stool or flatus. Laxatives--Medications that can promote peristalsis. paralytic ileus--Direct manipulation of the bowel during abdominal surgery inhibits peristalsis, causing a condition termed postoperative paralytic ileus. This temporary stoppage of peristalsis normally lasts 3 to 5 days. Many times, the patient is receiving opioids for pain relief, which can exacerbate the situation. Fissures--linear break on the margin of the anus. Occult blood--blood that is hidden in the specimen or cannot be seen on gross examination. Endoscopy--the direct visual examination of body organs or cavities. Flatulence--Formation of gases in the stomach or intestines is a result of normal breakdown of certain undigested foods in the large intestine or from swallowing of air when eating and drinking . Burping or belching is the way most swallowed air leaves the stomach. Some gas moves into the small intestine where it is partially absorbed, and a small amount travels into the large intestine for release through the rectum flatulence. Enema--the introduction of a solution into the large intestine, usually to remove feces. The instilled solution distends the intestine and irritates the intestinal mucosa, thus increasing peristalsis. can also be used to administer certain medications. Suppository--a conical or oval solid substance shaped for easy insertion into a body cavity and designed to melt at body temperature. Bowel incontinence or fecal incontinence is the loss of voluntary control of defecation, the inability of the anal sphincter to control the discharge of fecal and gaseous material. incontinence-associated dermatitis (IAD)—the prolonged contact of the skin with urine or feces leading to a form of moisture-associated skin damage (MASD). Erythema, maceration, denuding, and inflammation occur as a result of exposure to urine or stool and may affect the skin of the perineum, perianal area, buttocks, inner thighs, sacrum, and coccyx. bowel-training program--Patients with a history of chronic constipation and impaction and those who are incontinent of stool may benefit from a bowel-training program. The purpose is to manipulate factors within the person’s control (food and fluid intake, exercise, time for defecation) to produce the elimination of a soft, formed stool at regular intervals without a laxative. nasogastric (NG) tube--a pliable single- or double-lumen (inner open space) plastic tube that is hollow, allowing for the removal of gastric secretions and instillation of solutions such as medications or feedings into the stomach. Ostomy---a surgically formed opening in an organ of the body. Stoma--the part of the ostomy that is attached to the skin Ileostomy--allows liquid fecal content from the ileum of the small intestine to be eliminated through the stoma. Colostomy--permits formed feces in the colon to exit through the stoma. chap 25: Asepsis and Infection Control Host--living being where an infectious, parasitic, or pathogenic agent resides and receives sustenance. Antimicrobials--drugs that treat infections by killing or slowing the growth of microbes causing infection …. bacterial infections are treated with drugs called antibiotics. Infection is a disease state that results from the presence of pathogens (disease producing microorganisms) in or on the body. Bacteria, the most significant and most commonly observed infection-causing agents in health care institutions, can be categorized in various ways. They are categorized by shape: spherical (cocci), rod shaped (bacilli), or corkscrew shaped (spirochetes). Most bacteria require oxygen to live and grow and are, therefore, referred to as aerobic. Those that can live without oxygen are anaerobic bacteria. Virus is the smallest of all microorganisms, visible only with an electron microscope. Viruses cause many infections, including the common cold, hepatitis A, B, and C, and human immunodeficiency virus (HIV). Fungi, plantlike organisms (molds and yeasts) that also can cause infection, are present in the air, soil, and water. Some examples of infections caused by fungi include athlete’s foot, ringworm, and yeast infections. Parasites are organisms that live on or in a host and rely on it for nourishment. An organism’s potential to produce disease in a person depends on a variety of factors, including: Number of organisms Virulence of the organism, or its ability to cause disease Competence of the person’s immune system Length and intimacy (extent) of the contact between the person and the microorganism Endemic (occurs with predictability in one specific region or population) can appear in a different geographic location. Pandemics, like COVID-19, are global outbreaks of a novel (new or not previously identified) virus that did not initially not have a known immunization or treatment. The reservoir for growth and multiplication of microorganisms is the natural habitat of the organism. Possible reservoirs that support organisms pathogenic to humans include other people, animals, soil, food, water, milk, and inanimate objects. Direct contact requires close proximity between the susceptible host and an infected person or a carrier, and includes activities such as touching, kissing, and sexual intercourse. Indirect contact involves personal contact with either: (1) a vector, a living creature that transmits an infectious agent to a human, usually an insect; (2) an inanimate object, called a fomite, such as equipment or countertops. Airborne transmission --Microorganisms can also be spread through the airborne route when an infected host coughs, sneezes, or talks, or when the organism becomes attached to dust particles. Another means of transmission is through droplets. Droplet transmission is similar to airborne transmission. However, airborne particles are smaller than 5 μm (micrometer), and droplet particles are greater than 5 μm. Contact tracing-- involves identifying people with an infectious disease and locating individuals and groups with whom they have come into direct contact to interrupt actual or potential transmission of the infectious disease. Antigen --The foreign material is called an antigen. Antibody --the body commonly responds to the antigen by producing an antibody. Asepsis --The practice of asepsis includes all activities to prevent infection or break the chain of infection. The nurse uses aseptic techniques to halt the spread of microorganisms and minimize the threat of infection. There are two asepsis categories: medical asepsis and surgical asepsis. Medical asepsis, or clean technique, involves procedures and practices that reduce the number and transfer of pathogens. Medical asepsis procedures include performing hand hygiene and wearing gloves. Surgical asepsis, or sterile technique, includes practices used to render and keep objects and areas free from microorganisms. Surgical asepsis procedures include inserting an indwelling urinary catheter or inserting an IV catheter. Health care–associated infections (HAIs)--develops as a result of medical care and may occur in many health care settings including hospitals, rehabilitation facilities, outpatient settings, and dialysis centers. The source of an HAI may be either exogenous or endogenous. An infection is referred to as exogenous when the causative organism is acquired from other people. An endogenous infection occurs when the causative organism comes from microbial life harbored in the person. An infection is referred to as iatrogenic when it results from a treatment or diagnostic procedure. Disinfection destroys all pathogenic organisms except spores; Sterilization destroys all microorganisms, including spores/endospores. Personal protective equipment(PPE) includes gloves, gowns, masks, and protective eye gear. To minimize or prevent exposure to infectious material. Isolation--a protective procedure that limits the spread of infectious diseases among hospitalized patients, hospital personnel, and visitors. Bundles are typically three to five evidence-based practices that, when implemented together, improve patient outcomes. Chapter 33: Skin Integrity and Wound Care Epidermis --The top layer, or outermost portion. The epidermis is composed of layers of stratified epithelial cells. These cells fuse to form a protective, waterproof layer of keratin material. Epithelial cells have no blood vessels of their own and depend on underlying tissues for nourishment and waste removal. When well nourished, epithelium regenerates relatively easily and quickly. Dermis ---The second layer of skin, consists of a framework of elastic connective tissue comprised primarily of collagen. Nerves, hair follicles, glands, immune cells, and blood vessels are located in this layer (Norris, 2019). Each hair consists of the shaft, which projects through the dermis beyond the surface of the skin, and the hair follicle, which lies in the dermis. Subcutaneous tissue --the bottom layer that anchors the skin layers to the underlying tissues of the body. The subcutaneous tissue consists of adipose tissue, made up of lobules of fat cells, and connective tissue. This layer stores fat for energy, serves as a heat insulator for the body, and provides a cushioning effect for protection. This fatty tissue layer contains blood and lymph vessels, nerves, and fat cells. Wound is a break or disruption in the normal integrity of the skin and tissues. Exudate –(After a brief period of constriction during homeostasis) the blood vessels dilate and capillary permeability increases, allowing plasma and blood components to leak out into the area that is injured, forming a liquid called exudate. Ex: Serosanguinous exudate. Granulation tissue --The new tissue forms the foundation for scar tissue development. It is highly vascular, red, and bleeds easily. Scar (avascular collagen tissue that does not sweat, grow hair, or tan in sunlight) eventually becomes a flat, thin line. Scar tissue is less elastic than uninjured tissue. The strength of the scar tissue remains less (70% to 80%) than that of normal tissue, even many years following injury, and it is never fully restored. Wounds that heal by secondary intention take longer to remodel and form a scar smaller than the original wound. A variety of factors affect wound healing. Local factors, those occurring directly in the wound, include pressure, desiccation (dehydration), maceration (overhydration), trauma, edema, infection, excessive bleeding, necrosis (death of tissue), and the presence of biofilm (a thick grouping of microorganisms). Wound biofilms are the result of wound bacteria growing in clumps, embedded in a thick, self-made, protective, slimy barrier of sugars and proteins. This barrier contributes to decreased effectiveness of antibiotics against the bacteria (antibiotic resistance) and decreases the effectiveness of the normal immune response by the patient. Epithelialization --epithelial cells form a new surface layer. Eschar --Dead tissue present in the wound delays healing. Dead tissue appears as slough—moist, yellow, stringy tissue—and eschar appears as dry, black, leathery tissue. Hematoma --Internal hemorrhage causes the formation of a hematoma, a localized mass of usually clotted blood. Dehiscence and evisceration are the most serious postoperative wound complications. Dehiscence is the partial or total separation of wound layers as a result of excessive stress on wounds that are not healed. Evisceration is the most serious complication of dehiscence. It occurs primarily with abdominal incisions. In evisceration, the abdominal wound completely separates, with protrusion of viscera (internal organs) through the incisional area. Fistula is an abnormal passage from an internal organ or vessel to the outside of the body, or from one internal organ or vessel to another. Fistulas may be created purposefully; for example, an arteriovenous (AV) fistula is created surgically to provide circulatory access for kidney dialysis. Abscess --However, fistula formation is often the result of infection that has developed into an abscess, which is a collection of infected fluid that has not drained. Accumulated fluid applies pressure to surrounding tissues, leading to the formation of the unnatural passage between two visceral organs or an organ and the skin. Pressure injury is defined as localized damage to the skin and underlying tissue that usually occurs over a bony prominence or is related to the use of a (medical or other) device. The National Pressure Injury Advisory Panel recently updated their staging definitions, and the term Pressure ulcer was replaced by pressure injury to better-represent the early stages of pressure injury where there is not an actual ulcer or break in the skin. A pressure injury may be acute or chronic. Ischemia--deficiency of blood in a particular area. Hypoxia --inadequate amount of oxygen available to cells. Friction occurs when two surfaces rub against each other. The injury, which resembles an abrasion, can also damage superficial blood vessels directly under the skin. A patient who lies on wrinkled sheets is likely to sustain tissue damage as a result of friction. Shear results when one layer of tissue slides over another layer. Shear separates the skin from underlying tissues. Shear includes shear stress, the force, and shear strain, the “distortion or deformation of tissue” (NPIAP, 2019, p. 5) secondary to shear stress. The small blood vessels and capillaries in the area are stretched and possibly tear, resulting in decreased circulation to the tissue cells under the skin. Erythema--redness in lightly pigmented skin. DRAINAGE--The inflammatory response results in the formation of exudate which then drains from the wound. The exudate may contain fluid/serum, cellular debris, bacteria, and leukocytes. This exudate is called wound drainage and is described as serous, sanguineous, serosanguineous, or, if infected, purulent. • Serous drainage is composed primarily of the clear, serous portion of the blood and from serous membranes. Serous drainage is clear and watery. • Sanguineous drainage consists of large numbers of red blood cells and looks like blood. Bright-red sanguineous drainage is indicative of fresh bleeding, whereas darker drainage indicates older bleeding. • Serosanguineous drainage is a mixture of serum and red blood cells. It is light pink to blood tinged. • Purulent drainage is made up of white blood cells, liquefied dead tissue debris, and both dead and live bacteria. Purulent drainage is thick, often has a musty or foul odor, and varies in color (such as dark yellow or green), depending on the causative organism. Presence of any abnormal pathways in the wound, such as a sinus tract (a cavity or channel underneath the wound that has the potential for infection) or tunneling (a passageway or opening that may be visible at skin level, but with most of the tunnel under the surface of the skin). Dressing --protective coveringplaced over a wound. Debridement --removal of devitalized tissue and foreign material. Bandages are strips of cloth, gauze (e.g., roller gauze, Kerlix, Kling), or elasticized material (e.g., ACE bandages) used to wrap a body part. Negative pressure wound therapy (NPWT) promotes wound healing and wound closure through the application of uniform negative pressure on the wound bed, reduction in bacteria in the wound, and the removal of excess wound fluid, while providing a moist wound healing environment. Vasoconstriction --the constriction of blood vessels, which increases blood pressure. Vasodilation --the dilatation of blood vessels, which decreases blood pressure.