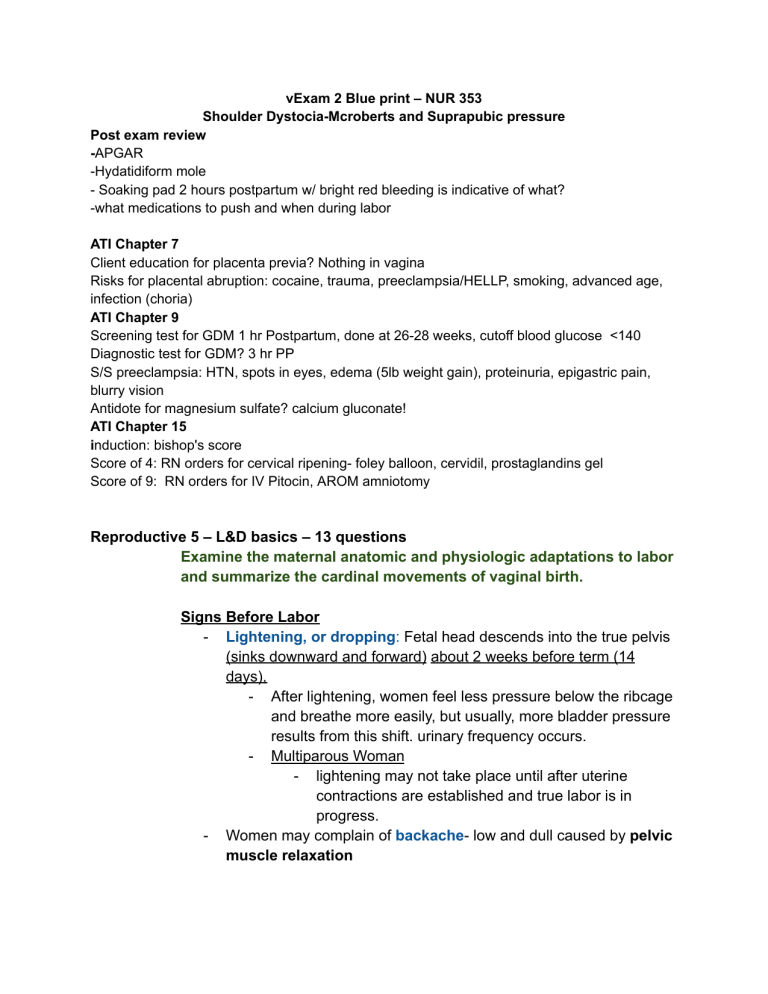
vExam 2 Blue print – NUR 353 Shoulder Dystocia-Mcroberts and Suprapubic pressure Post exam review -APGAR -Hydatidiform mole - Soaking pad 2 hours postpartum w/ bright red bleeding is indicative of what? -what medications to push and when during labor ATI Chapter 7 Client education for placenta previa? Nothing in vagina Risks for placental abruption: cocaine, trauma, preeclampsia/HELLP, smoking, advanced age, infection (choria) ATI Chapter 9 Screening test for GDM 1 hr Postpartum, done at 26-28 weeks, cutoff blood glucose <140 Diagnostic test for GDM? 3 hr PP S/S preeclampsia: HTN, spots in eyes, edema (5lb weight gain), proteinuria, epigastric pain, blurry vision Antidote for magnesium sulfate? calcium gluconate! ATI Chapter 15 induction: bishop's score Score of 4: RN orders for cervical ripening- foley balloon, cervidil, prostaglandins gel Score of 9: RN orders for IV Pitocin, AROM amniotomy Reproductive 5 – L&D basics – 13 questions Examine the maternal anatomic and physiologic adaptations to labor and summarize the cardinal movements of vaginal birth. Signs Before Labor - Lightening, or dropping: Fetal head descends into the true pelvis (sinks downward and forward) about 2 weeks before term (14 days), - After lightening, women feel less pressure below the ribcage and breathe more easily, but usually, more bladder pressure results from this shift. urinary frequency occurs. - Multiparous Woman - lightening may not take place until after uterine contractions are established and true labor is in progress. - Women may complain of backache- low and dull caused by pelvic muscle relaxation - Rupture of Membranes- spontaneous rupture of membranes can initiate labor or can occur anytime during labor most commonly in the transition phase - Labor occurs within 24 hours of rupture of membrane - Prolonged rupture of membranes greater than 24 hours before the delivery of fetus can lead to an infection - A nurse should assess the FHR for abrupt decelerationscan be indicative of fetal distress to rule out umbilical cord prolapse - Strong frequent irregular uterine (Braxton Hicks) contractions - Vaginal mucus becomes more profuse in response to extreme congestion of the vaginal mucous membranes. - Bloody Show: brownish or blood-tinged cervical mucus may be passed - Cervical Ripening: Cervix becomes soft (ripens), partially effaced, may begin to dilate - Weight loss of 0.5 to 1.5 kg (1-3 ½ lbs) - Surge of energy- sometimes referred to as “nesting” response Stages of Labor - Starts with uterine contraction leading to cervical changes - Prelabor what triggers onset of labor - Bloody show - Water breaking - True contractions cause the cervix to dilate and efface First stage of labor 1) Latent (early) phase of labor a) Usually lasts up to 20 hrs or until cervix dilated to 3 cm b) Irregular Contractions are every 20-30 minutes and last 30 seconds c) Effacement 30% 2) Active phase of labor a) Regular contractions occur, every 3-5 minutes and last up to 1 minute b) Cervix dilates from 3 cm to 6 cm c) Effacement 80% 3) Transitional phase a) Cervix dilates from 6-10 cm b) 100% effacement c) Contractions intense, 1-1.5 minutes each, every 0.5 to 2 minutes d) Amniotic sac ruptures at this point if it hasn’t already Second Stage of Labor (Pushing Stage) - - Critical thing is for the baby's head to navigate through the maternal pelvis - Depends on the Five Ps - Power: Forceful contractions - Passenger: Fetus - Passage: Route through bony pelvis - Position - Psychological changes - Factors that determine how easy the passage will be for the fetus - Fetal size: size of fetal head - Fetal attitude: way the fetal body is flexed, normally fetus is fully flexed w/ chin on chest and rounded back, flexed arms and legs - Fetal Lie - Longitudinal (ideal) - Transverse (perpendicular to moms spine) - Oblique (slight angel) - Fetal Presentation - Cephalic (Head first) - Vertex: complete flexion of head - Breech (butt first) - Shoulder Cardinal Movements - Engagement: When the biparietal diameter of the head passes the pelvic inlet, the head is said to be engaged in the pelvic inlet. Typically occurs before the onset of active labor - Decent: downward movement of fetus into pelvic inlet - Degree of descent is called the fetal station (pelvic inlet -5, ischial spine= 0 (engagement), - depends on at least four forces: (1) pressure exerted by the amniotic fluid (2) direct pressure exerted by the contracting fundus on the fetus (3) force of the contraction of the maternal diaphragm and abdominal muscles in the][ second stage of labor (4) extension and straightening of the fetal body - Flexion: fetal chin presses against chest as its head meets resistance against pelvic floor. - - - Internal rotation: Fetal shoulders internally rotate 45 degrees so widest part of shoulders meet widest part of pelvic inlet (fetus faces posteriorly) Extension: occurs at +4 station fetal head will change from flexion to extension, Moves to +5 and emerges from vagina Restitution and external rotation: +5 station Head externally rotates so shoulders can pass through pelvic outlet and under symphysis pubis Expulsion: anterior shoulder slips under symphysis pubis followed by post shoulder then followed by rest of body - After birth of the shoulders, the head and shoulders are lifted up toward the mother's pubic bone, and the trunk of the baby is born by flexing it laterally in the direction of the symphysis pubis. Third Stage of labor (Delivery of Placenta) - Uterus contracts firmly and placenta begins to descend into uterine wall Explain the five major factors that affect the labor process and describe the ongoing assessment of maternal progress during the first, second, third and fourth stages of labor. The Five Ps - Powers: how far apart, how strong, how long does it last - Passenger: refers to the baby and the position they are in (issues that may cause labor issues. breech baby, the cervix - Passage: Refers to the baby and the position the are in (issues that may cause labor issues: breech baby, the cervix - Position: Position of mother, best thing to do is make the mother stay upright and moving, frequent position change helps with L&D by using to help the baby descend into the birth canal. - Psychological state: Anxiety and fear can help impede the labor process, clear the delivery room of distractions or or factors that may induce anxiety Assessment of maternal progress during labor stages Prior to admission - - Assess clients labor status, conduct admission hx, review of antepartum care, birth plan - Obtain laboratory reports - Monitor baseline fetal heart tones and uterine contraction patterns for 20-30 minutes - Obtain maternal vital signs - Check status of amniotic membranes Maternal and fetal assessments should take place throughout labor process and immediately after birth Cervical dilation is the single most important indicator of the progress of labor Progress if labor is affected by fetal head size, fetal presentation, fetal lie, fetal attitude, and fetal position First Stage Assessment - Perform Leopold maneuvers - Perform a vaginal examination (if no evidence of progress) - Encourage client to take slow deep breaths prior to vaginal exam - Monitor cervical dilation and effacement - Monitor station and fetal presentation - Prepare for impending delivery as presenting part moves into positive stations and begins to push against pelvic floor (crowning) - Perform bladder palpation on regular basis to prevent bladder distention - Perform temperature assessment every 4 hr (2 hr for membrane rupture) Nursing Actions - During Active phase - Provide client/fetal monitoring - Encourage frequent position changes - Encourage voiding at least every 2 hrs - Encourage deep cleansing breaths before and after modified paced breathing - Encourage relaxation - Provide nonpharm comfort measures - Provide pharmacological pain relief as prescribed - During Transition Phase - Encourage voiding every 2 hours - Continue to monitor and support the client and fetus - Encourage rapid pant-pant-blow breathing pattern Discourage pushing efforts until the cervix Listen for client statements expressing need to have bowel movement Prepare client for birth Observe for perineal bulging or crowning Encourage client to begin bearing down with contractions once cervix is dilated fully Second Stage Assessment - Blood pressure, pulse, and respirations every 5 to 30 minutes - Uterine contractions - Pushing efforts by client - Increase in bloody show - Shaking of extremities - FHR every 5 to 15 minutes (depending on fetal risk status) and immediately following birth - Assessment of perineal lacerations, usually occur as fetal head is expulsed Third Stage Assessment - BP, pulse and respiration measurement every 15 min - Clinical findings of placental separation from the uterus as indicated by - Fundus firmly contracting - Swift gush of dark blood from introitus - Umbilical cord appears to lengthen as placenta descends - Assignment of 1 and 5 min APGAR scores to the neonate Fourth Stage Assessment - Maternal vital signs - Fundus - Lochia - Urinary Output - Baby-friendly activities of family Assessments related to possible rupture of membranes - FIRST assess FHR to ensure there is no fetal distress from potential umbilical cord prolapse - Verify presence of alkaline amniotic fluid using nitrazine paper Expected findings of amniotic fluid are clear, color of water, free of odor Abnormal finding include: meconium Identify signs of developing complications during labor and birth. Prolapsed Umbilical Cord Risk Factors - Rupture of amniotic membranes - Abnormal fetal presentation (any presentation other than vertex) - Transverse lie: presenting part not engaged, which leaves room for cord to descend - Small-for-gestational age fetus - Unusually long umbilical cord - Multifetal pregnancy - Unengaged presenting part - Hydramnios or polyhydramnios Expected findings - Client reports that feel something coming through the vagina - visualization for palpation of the umbilical cord protruding from the introitus - By FHR Monitoring shows variable or prolonged deceleration - Excessive fetal activity followed by sensation of movement, suggestive of severe fetal hypoxia Meconium-Stained amniotic fluid - Meconium passage in the amniotic fluid during the antepartum period prior to the start of Labor is typically not associated with an unfavorable fetal outcome - Fetus has had an episode of loss of sphincter control, allowing meconium to pass into amniotic fluid Assessment/SIGNS - Amniotic fluid can vary in color: Black to Greenish, or yellow, through meconium-stained amniotic fluid is often green. Consistency can be thick - Criteria for evaluation of meconium-stained amniotic fluid - Often present in breech presentation, and might not indicate fetal hypoxia - Present with no changes in FHR - Stained fluid accompanied by variable or late decelerations in FHR (ominous finding) Fetal Distress - FHR is below 110/min or above 160/min - FHR shows decreased or no variability - There is fetal hyperactivity or no fetal activity Dystochia - Dysfunctional labor is a difficult or abnormal labor related to the 5 P's of Labor - abnormal uterine contraction patterns prevent the normal process of Labor and its progression Expected findings - lack of progress and dilation, effacement, or fetal descent during labor - a hypotonic uterus is easily indent-able even at the peak of contraction - Hypertonic uterus cannot be indented in, even between contractions - client is ineffective in pushing with no voluntary urge to Bear Down - persistent occiput posterior presentation is when the fetal occiput is directed towards the posterior maternal pelvis rather than the anterior pelvis - Persistent occiput posterior position prolongs labor and the client reports greater back pain as fetus presses against the maternal sacrum Uterine Rupture - Rupture involves the uterine wall, peritoneal cavity, and/or broad ligament. internal bleeding is present - Incomplete rupture occurs with dehiscence at the sight of a prior scar - Client reports sensation of ripping / tearing or Sharp pain - Client reports abdominal pain and uterine tenderness Precipitous Labor - Precipitous Labor is defined as a labor that last 3 hours or less from the onset of contractions to the time of the delivery During Labor - low backache - abdominal pressure and cramping - increase or bloody vaginal discharge - palpable uterine contractions - progress of cervical dilation and effacement Diarrhea fetal presentation, station, and position Status of amniotic membranes Post-birth - assess maternal perineal area for indications of trauma or lacerations - assess neonates color and for indications of hypoxia - assess for indications of trauma to presenting part of neonate, especially on cephalic presentation Describe the role and responsibilities of the nurse during labor and childbirth. First Stage Assessment - Perform Leopold maneuvers - Perform a vaginal examination (if no evidence of progress) - Encourage client to take slow deep breaths prior to vaginal exam - Monitor cervical dilation and effacement - Monitor station and fetal presentation - Prepare for impending delivery as presenting part moves into positive stations and begins to push against pelvic floor (crowning) - Perform bladder palpation on regular basis to prevent bladder distention - Perform temperature assessment every 4 hr (2 hr for membrane rupture) Nursing Actions - During Active phase - Provide client/fetal monitoring - Encourage frequent position changes - Encourage voiding at least every 2 hrs - Encourage deep cleansing breaths before and after modified paced breathing - Encourage relaxation - Provide non pharm comfort measures - Provide pharmacological pain relief as prescribed - During Transition Phase - Encourage voiding every 2 hours - Continue to monitor and support the client and fetus Encourage rapid pant-pant-blow breathing pattern Discourage pushing efforts until the cervix Listen for client statements expressing need to have bowel movement Prepare client for birth Observe for perineal bulging or crowning Encourage client to begin bearing down with contractions once cervix is dilated fully Second Stage Nursing Actions - Continue to monitor the client/ fetus - Assist in positioning of the client for effective pushing - Assistant partner involvement with pushing efforts and an encouraging bearing down efforts during contraction - promote rest between contractions - provide Comfort measures such as cold compresses - Cleanse clients perineum as needed if fecal material is expelled during pushing - prepare for a episiotomy if needed - provide feedback on labor progress to the client - prepare for care of the neonate - check O2 flow and tank on warmer - preheat radiant warmer - layout newborn stethoscope and bulb syringe - have resuscitation equipment in working order - check suction apparatus Third Stage Nursing Actions - Instruct the client to push once findings of placental separation is present - keep client/parents informed of progress of placental expulsion and perennial repair if appropriate - Administer oxytocics as prescribed to stimulate the uterus to contract and prevent hemorrhage - administer analgesics - clean the perineal area with warm water and apply perineal pad or ice pack to Premium - promote baby friendly activities between the family and newborn stimulating release of oxytocin Fourth Stage Nursing Actions - Assess maternal blood pressure and pulse every 15 minutes for the first two hours and determine the temperature at the beginning of the recovery., Then assess every 4 hours for the first 8 hours after birth at least every 8 hours - assess fundus and Lochia every 15 minutes for the first hour and then according to family protocol every 15 minutes for the first hour and then according to family protocol - Massage of uterine fundus and or administer oxytocics to maintain uterine tone and prevent hemorrhage - encourage voiding to prevent bladder distention - Assess episiotomy or laceration repair for erythema - Promote an opportunity for parents on newborn bonding Compare nonpharmacologic and pharmacologic methods used to enhance relaxation and relieve pain in different stages of labor and for vaginal and cesarean birth. First Stage Pain causes - dilation, effacement, and stretching of cervix - distention of the lower segment of the uterus - contractions of the uterus with resultant uterine ischemia Second Stage Pain causes - pressure and distention of the vagina and the perineum, describe by the client as burning, splitting, and tearing - pressure and pulling in the pelvic structures - lacerations of soft tissue Third stage Pain causes - Uterine contractions - Pressure and pulling of pelvic structures Fourth Stage Pain causes - Distention and stretching of the vagina and perineum incurred during the second stage with a splitting, burning, and tearing sensation Pharmacologic 1. Systemic analgesia: Crosses the blood-brain barrier & placental barrier; can affect the fetus - Opioid Agonist/Antagonists - Opioid Agonists Stadol or Nubain 2. Anesthesia: Does not cross the blood-brain barrier; less effect on fetus - Epidural - Intrathecal (not as common) - Spinal - Local blocks (pudental, etc.) - General anesthesia - Nitrous oxide 3. Opioid Analgesics Nonpharmacological: Cognitive Strategies - Childbirth education - Childbirth preparation methods (Lamaze, patterned breathing, exercises) promotes relaxation and pain management - Hypnosis - Biofeedback Sensory stimulation strategies - Aromatherapy - Breathing techniques - Imagery - Music - Use of focal points - Subdued lighting Cutaneous stimulation strategies - Therapeutic touch and massage: back rubs and massage - Walking - Rocking - Effleurage - Sacral counterpressure - Application of heat or cold - Transcutaneous electrical nerve stimulation (TENS) therapy - Hydrotherapy - Acupressure - Frequent maternal Position changes promote relaxation and pain relief Reproductive 6: Pregnancy Complications – 7-9 questions Provide education about screening and diagnostic testing in pregnancy to women with perinatal risk factors. Cervical Insufficiency Diagnostic and therapeutic procedures - Ultrasound showing short cervix less than 25 mm in length - Prophylactic cervical cerclage Hyperemesis Gravidarum Diagnostic and therapeutic procedures - Urinalysis - Chemistry profile - Thyroid test - CBC Iron Deficiency Anemia Diagnostic and therapeutic procedures - Hgb less than 11 mg/dL in first and third trimester - Hct less than 33% - Blood ferritin less than 12 mcg/L in presence of low Hgb Gestational Diabetes Mellitus Diagnostic and therapeutic procedures - Glucola Screening test/1 hr glucose tolerance test - - 1 hour Oral glucose tolerance test @ 24-28 weeks >140 = abnormal 3 hr glucose tolerance test. Begins with fasting blood glucose then client follows unrestricted glucose diet and glucose is recorded at 1 hr, 2 hr, 3 hr Presence of ketones in the urine Biophysical profile to ascertain fetal well-being if nonstress test is nonreactive Amniocentesis w/ amniotic fluid phosphatidylglycerol measured to determine fetal lung maturity Nonstress test to assess fetal well-being Gestational Hypertension - Liver enzymes - Blood creatinine, BUN, uric acid - CBC - Clotting studies - Chemistry profile - Diagnostic Procedures: - Dipstick testing or urine proteinuria - 24 hr urine collection for protein and creatinine clearance - Nonstress test, contraction stress test, biophysical profile, serial ultrasounds to address fetal status - Doppler blood flow analysis to assess fetal well-being - Daily kick counts Develop a plan of care for the woman with pre-gestational diabetes or gestational diabetes. https://www.youtube.com/watch?v=mYvOwipZKXI Monitor clients blood glucose Monitor fetus Describe the etiologic theories and pathophysiology of preeclampsia. https://www.youtube.com/watch?v=pnGyENcL2j0 Gestational Hypertension: begins after the 20th week of pregnancy, hypertensive disorders of pregnancy whereby client has an elevated blood pressure at 140/90 mm Hg or greater recorded on 4 different occasions, 4 hours apart. BP should return to baseline 12 weeks postpartum Preeclampsia: Form of GH with proteinuria greater than or equal to +1. Client reports transient headaches and episodes of irritability may occur. Edema can be present ● Severe Preeclampsia: BP that is 160/110 mm Hg or greater, proteinuria greater than 3+, olguria, elevated blood creatine (greater than 1.1 mg/dL), cerebral or visual disturbances (headache or blurred vision), hyperreflexia with possible as ankle clonus, pulmonary or cardiac involvement, extensive peripheral edema, hepatic dysfunction, epigastric and RUQ pain, thrombocytopenia Eclampsia: Severe preeclampsia manifestations with the onset of seizure activity or coma. Preceded by headache, severe epigastric pain, hyperreflexia, and hemoconcentrators HELLP syndrome: variant of GH where hematologic conditions coexist w/ severe preeclampsia involving hepatic dysfunction. Diagnosed by the following Lab tests - H:hemolysis resulting in anemia and jaundice - EL: elevated liver enzymes - LP: low platelet count Risk factors for GH Disorders - Maternal age younger than 19 or older than 40 years - First pregnancy - Extreme obesity - Multifetal pregnancy - Chronic renal disease - Chronic hypertension - Familiar hx of preeclampsia - DM - RA - Systemic lupus erythematosus Expected Findings - Severe continuous headache - Nausea - Blurring of vision - Flashes of lights or dots before the eyes Physical Assessment Findings - HT, proteinuria, facial/hand/periorbital/abdominal edema, pitting edema of lower extremities, vomiting, olguria, hyperreflexia, Scotoma, EG pain, RUQ pain, Dyspnea, diminished BS, seizures, jaundice, worsening liver involvement, kidney failure, worsening HT, cerebral involvement Lab Findings - Elevated Liver Enzymes - Inc. creatinine, plasma uric acid - Thrombocytopenia - Hgb (decreased in HELLP, increased in preeclampsia) - Hyperbilirubinemia Diagnostic Procedures - Dipstick testing (protein proteinuria) - 24 hr urine collection for protein and creatinine clearance - Nonstress test, contraction stress test, biophysical profile, serial ultrasounds for fetal status, doppler blood flow analysis for fetal well being, daily kick counts Discuss the preconception, antepartum, intrapartum and postpartum management of the women with hypertensive disorders in pregnancy. Preconception Management - Take a basic history of the client/look at the recorded maternal history - Ask about headache, visual disturbances, epigastric pain (liver involvement with preeclampsia) - vasoconstriction of cerebral vessels can lead to headache/visual changes - Uric acid: use dipstick test - 24 hr urine collection for protein and creatinine clearance - Chemistry profile - Obtain a full CBC - Refer to HELLP - H: hemolysis resulting in anemia and jaundice (RBCs) - EL: elevated liver enzymes (BUN) - LP: low platelet count Look for risk factors including: - Maternal age (younger than 19 or older than 40) - First pregnancy - Extreme obesity - Multifetal gestation - Chronic renal disease - Chronic HTN - Family history of preeclampsia - DM - RA - Systemic lupus eryhtematosus Antepartum Management - Nonstress test, contraction stress test, biophysical profile, serial ultrasounds to address fetal status - Doppler blood flow analysis to assess fetal well-being - Daily kick counts - Assess LOC - Obtain pulse Ox - Monitor UO - Obtain daily weights - Monitor vitals - Encourage lateral positioning - Instruct client to monitor I&Os Intrapartum Management - Doppler blood flow analysis to assess fetal well-being - Assess LOC - Obtain pulse Ox - Monitor vitals - Look out for findings - Severe headache - Nausea - The blurring of vision, flashes of lights or dots before the eyes - Physical assessment findings - HTN, proteinuria, facial/hand/periorbital/abdominal edema, pitting edema of lower extremities, vomiting, oliguria, hyperreflexia, Scotoma, EG pain, RUQ pain, Dyspnea, diminished BS, seizures, jaundice, worsening liver involvement, kidney failure, worsening HT, cerebral involvement Postpartum Management - Client education - Remain on bed rest in a side-lying position - Perform diversional activities - Avoid high sodium foods - Avoid alcohol, tobacco, limit caffeine intake - Drink 6-8 oz glasses of water/day Differentiate among causes, signs and symptoms, possible complications and management of miscarriage, ectopic pregnancy, cervical insufficiency and hydatidiform mole. https://www.youtube.com/watch?v=JcRBZ4c-vHM Miscarriage Causes: Signs and symptoms: Complications: Management: Ectopic pregnancy Causes: Abrupt unilateral lower qua Signs and symptoms: Complications: Management: Cervical Insufficiency Causes: thought to be related to tissue changes and alterations in the length of the cervix. Risk factors include: hx of cervical trauma, short labors, preg loss in early gest, advanced cervical dilation, congenital structural defects of the uterus of cervix Signs and symptoms: - Pink stained vaginal discharge/bleeding - A possible gush of fluid (rupture of membranes) - Uterine contractions w/ expulsion of the fetus Complications: - Prophylactic cervical cerclage Management: - Evaluate client support systems and assistance if on bed rest - Assess vaginal discharge - Monitor client reports of pressure and contractions - Check vitals Hydatidiform mole Causes: Signs and symptoms: Complications: Management: Compare and contrast placenta previa and placental abruption in relation to signs and symptoms, complications, and management. https://www.youtube.com/watch?v=FDRSPppWe2k Placenta Previa - If the placenta bursts the blood is bright red - May fix itself but C section may be required Placental Abruption - Blood will be dark red because it will be old Reproductive 7: L&D complications – 7-9 questions Analyze current interventions to prevent preterm labor and birth, including the use of tocolytic and antenatal glucocorticoid medications. - Activity restriction, modified bed rest w/bathroom privileges Left lateral position to increase blood flow Avoid sexual intercourse Nifedipine- calcium channel blocker used to suppress contractions Magnesium sulfate- Tocolytic that is a CNS depressant and relaxes the smooth muscle which inhibits uterine activity by suppressing contractions Define and describe indications and medications for cervical ripening and labor induction and augmentation. Terbutaline- beta-adrenergic agonist that is used as tocolytic and relaxes smooth muscles and inhibits the uterine activity Betamethasone- Glucocorticoid administered IM in 2 injections 24 hrs apart and takes 24 hours to be effective. Therapeutic action is to enhance fetal lung maturity and surfactant production in fetuses between 24 to 34 weeks Pitocin: Increases the frequency and strength of contractions Summarize nursing care for a woman experiencing a trial of labor, induction or augmentation of labor, a forceps- or vacuum-assisted birth, a cesarean birth, or vaginal birth after a cesarean birth (VBAC). MECHANICAL AND PHYSICAL METHODS - Balloon catheter is inserted into the intracervical canal to dilate the cervix. - NURSING ACTIONS - - Assessing for - Urinary retention - Rupture of membranes - Uterine tenderness or pain - Contractions - Vaginal bleeding - Fetal distress INTERVENTIONS - Obtain baseline data on fetal and maternal well-being. - Assist the client to void prior to the procedure. - The client should remain in a side-lying position. - Monitor FHR and uterine activity after administration of cervical-ripening agents. - Notify the provider if uterine tachysystole or fetal distress is noted. - Monitor for potential adverse effects (nausea, vomiting, diarrhea, fever, uterine tachysystole). INDUCTION OF LABOR - The deliberate initiation of uterine contractions to stimulate labor before spontaneous onset to bring about the birth by chemical or mechanical means. - CLIENT PREPARATION - If cervical-ripening agents are used, baseline data on fetal and maternal well-being should be obtained. - Monitor FHR and uterine activity after administration of cervical-ripening agents. - Notify the provider of uterine tachysystole or fetal distress. - Assess fluid intake and urinary output. - A Bishop score rating should be obtained prior to starting any labor induction protocol. AMNIOTOMY - The artificial rupture of the amniotic membranes (AROM) by the provider using a hook, clamp, or other sharp instrument. - ONGOING CARE - Ensure that the presenting part of the fetus is engaged prior to an amniotomy to prevent cord prolapse. - Monitor FHR prior to and immediately following AROM to assess for cord prolapse as evidenced by variable or late decelerations. - Assess and document characteristics of amniotic fluid including color, odor, and consistency. AMNIOINFUSION - Normal saline or lactated Ringer’s is instilled into the amniotic cavity through a transcervical catheter introduced into the uterus to supplement the amount of amniotic fluid. - INTERVENTIONS - Warm fluid using a blood warmer prior to infusion. Fluid should be room temperature. - Perform nursing measures to maintain comfort and dryness because the infused fluid will leak continuously. - Monitor the client to prevent uterine overdistention and increased uterine tone, which can initiate, accelerate, or intensify uterine contractions and cause nonreassuring FHR changes. - Continually assess intensity and frequency of uterine contractions. - Continually monitor FHR. - Monitor fluid output from vagina to prevent uterine overdistention. VACUUM-ASSISTED DELIVERY - Involves use of a cuplike suction device that is attached to the fetal head. Traction is applied during contractions to assist in the descent and birth of the head, after which, the vacuum cup is released and removed preceding delivery of the fetal body. - PREPARATION OF THE CLIENT - Provide the client and their partner with support and education regarding the procedure. - Assist the client into the lithotomy position to allow for sufficient traction of the vacuum cup when it is applied to the fetal head. - Assess and record FHR before and during vacuum assistance. - Assess for bladder distention, and catheterize if necessary. - INTERVENTIONS - Observe the neonate for lacerations, cephalohematomas, or subdural hematomas after delivery. - Check the neonate for caput succedaneum. FORCEPS-ASSISTED BIRTH - Consists of using an instrument with two curved spoon-like blades to assist in the delivery of the fetal head. Traction is applied during contractions. - CONSIDERATIONS - PREPARATION OF THE CLIENT - Explain the procedure to the client and their partner. - Assist the client into the lithotomy position. - Assess to ensure that the client’s bladder is empty, and catheterize if necessary. - Assess to ensure that the fetus is engaged and that membranes have ruptured. - INTERVENTIONS - Assess and record FHR before, during, and after forceps assistance. - If a FHR decrease occurs, the forceps are removed and reapplied. - Observe the neonate for bruising and abrasions at the site of forceps application after birth. Assess for facial palsy. - Check the client for any possible injuries after birth. - Vaginal or cervical lacerations indicated by bleeding in spite of contracted uterus - Urine retention resulting from bladder or urethral injuries - Hematoma formation in the pelvic soft tissues resulting from blood vessel damage CESAREAN BIRTH - NURSING ACTIONS - Assess and record FHR and vital signs. - Position the client in a supine position with a wedge under one hip to prevent compression of the vena cava. - - Insert an indwelling urinary catheter. - INTRA PROCEDURE - Assist in positioning the client on the operating table. - Continue to monitor FHR. - Continue to monitor vital signs, IV fluids, and urinary output. - Conduct instrument and sponge counts per protocol. POSTPROCEDURE - Monitor for evidence of infection and excessive bleeding at the incision site. - Assess the uterine fundus for firmness or tenderness. - Assess the lochia for amount and characteristics. - Monitor I&O. - Monitor vital signs per protocol. - Provide pain relief and antiemetics as prescribed. - Encourage splinting of the incision with pillows. - Encourage ambulation to prevent thrombus formation. VAGINAL BIRTH AFTER CESAREAN (VBAC) - INTRA PROCEDURE - Assess and record FHR during the labor. - Assess and record contraction patterns for strength, duration, and frequency of contractions. - Promote relaxation and breathing techniques during labor. - Provide analgesia as prescribed and requested. BISHOP SCORE - Used to determine maternal readiness for labor by evaluating whether the cervix is favorable by rating the following. - - Cervical dilation - Cervical effacement - Cervical consistency (firm, medium, or soft) - Cervical position (posterior, midposition, or anterior) - Station of presenting part Five factors are assigned a numerical value of 0 to 3, and the total score is calculated. - A Bishop score for a client at 39 weeks of gestation should be a score of 8 or more, which is indicative of a successful induction. CERVICAL RIPENING Increases cervical readiness for labor through promotion of cervical softening, dilation, and effacement. Can eliminate the need for oxytocin administration to induce labor, lower the dosage of oxytocin needed, and promote a more successful induction. Discuss obstetric emergencies and their appropriate management. Prolapsed umbilical cord - Nursing actions - Call for assistance immediately. - Do not leave the client. - Notify the provider. - Using a sterile-gloved hand, insert two fingers into the vagina, and apply finger pressure on either side of the cord to the fetal presenting part to elevate it off of the cord. Stay in this position until the delivery of the baby. - Reposition the client in a knee-chest, Trendelenburg, or a side-lying position with a rolled towel under the client’s right or left hip to relieve pressure on the cord. - Apply a warm, sterile, saline-soaked towel to the visible cord to prevent drying and to maintain blood flow. Provide continuous electronic monitoring of FHR for variable decelerations, which indicate fetal asphyxia and hypoxia. Administer oxygen at 8 to 10 L/min via a face mask to improve fetal oxygenation. Initiate IV access, and administer IV fluid bolus. Prepare for an immediate vaginal birth if cervix is fully dilated or cesarean section if it is not. Inform and educate the client and their partner about the interventions Reproductive 8: Postpartum care and complications – 7-9 questions Describe the anatomic and physiologic changes that occur during the postpartum period, including lochial flow and uterine involution characteristics. Recognize signs of potential complications in the postpartum woman. Physical Changes: - Uterine involution, cervical involution, decrease in vaginal distension, aleration in ovarian function/menstration, CV, UT, breast and GI tract changes - lochia flow: - Three stages: - Lochia rubra= dark red color 1-3 days post delivery - Lochia serosa= pinkish brown color 4-10 days - Lochia alba= yellowish white creamy color, 10 days- 8 weeks - Breastfeeding stimulates endogenous oxytocin which helps improve quality of uterine contractions and a firm contracted uterus - After delivery estrogen and progesterone decrease. - Decreased estrogen= breast engorgement, diaphoresis, diuresis - Decreased progesterone=increase in muscle tone Formulate a care plan for a woman in the postpartum period. Postpartum Assessment: “BUBBLE-LE” Breasts Uterus Bowel Bladder Lochia Episiotomy/Laceration Legs (thrombosis) Emotions Describe ways in which nurses can assist with parent-infant attachment and parental postpartum adjustment. Identify causes, signs and symptoms, possible complications, and nursing management of postpartum hemorrhage, postpartum infection, postpartum thromboembolic disorders, and postpartum psychological complications. Reproductive 9: Newborn care and nutrition – 7-9 questions Discuss the physiologic and behavioral adaptations that the neonate must make during the period of transition from the intrauterine to the extrauterine environment. Thermal Regulation: Chemical Thermogenesis: Glucose is needed for the thermogenic process. The hypothalamus releases norepinephrine, triggering production of glucose within the mitochondria of the brown fat → Heat is released in the form of ATP. Takes about 12 hours to establish thermal balance Risk related to thin subcutaneous fat, blood vessels closer to surface, larger body surface area - Limited ability to shiver Heat produced - metabolism of brown fat Heat produced - voluntary muscle activity: flexion of extremities, restlessness, and crying 4 causes of heat loss: Evaporation: Heat loss as water evaporates from the skin Prevention: heat lamps, warmer, dry the baby, warm blankets, delay first bath Convection: transfer of body heat to surrounding air ( cold del. Room), heat loss due to air currents in the room Conduction: transfer of heat to surface the newborn is lying on Prevention: covering/avoiding cold surfaces Radiation: loss of heat through the air to a cooler surface (not in direct contact with the neonate), baby being near something that’s cold Prevention: keep baby away from cold objects/areas - If baby is really cold, it will use its oxygen leading to metabolic acidosis’ - They will also use all their glucose causing hypoglycemia Pulmonary changes: - Vaginal delivery - thorax squeezed & fluid forced out - Mucus and meconium can be inhaled but small amount of fluid in lungs is absorbed - With first breath of air – increase in alveolar PO2 with relaxation of pulmonary arteries & pulmonary vascular resistance decreases allowing increased pulmonary vascular flow - First breath helps close ductus arteriosus, birth helps expand baby's chest though that compression and release (think bulb suction) Nasal breathers - in adults if nasal passage obstructed, adults will open mouth this reflex is not present until 3 weeks of age important to keep clear First heart rate assessment is assessed by grasping between fingers the base of the umbilical cord - Murmur may be present due to closures, no concern unless other physical signs (next semester) Apical heart rate obtained at the PMI which is located at the 4th intercostal space at the left midclavicular line - Blood volume varies due to length of time cord clamping, may vary as much as 100 ml What are the effects of cold stress on a newborn? See illustration in your textbook. - Newborns will use glucose and oxygen in an attempt to thermoregulate. Excessive glucose production/use from brown fat (subcutaneous) can result in hypoglycemia. Further the newborn will also rapidly use oxygen which can cause metabolic acidosis - Newborns do not shiver, instead they use a chemical process to maintain heat - Newborns may be at risk for poor growth/development when they are using all their calories to maintain their heat rather than to grow Explain newborn hyperbilirubinemia and describe related nursing assessments and interventions, including phototherapy. - - - - Newborns have a higher concentration of RBCs, Hemoglobin, and hematocrit at birth When RBC’s reach the end of their life span, their membranes rupture and hemoglobin is released Shorter neonatal RBC life span increases bilirubin production The liver helps break down the substance so it can be removed from the body in the stool. Normally, the liver filters bilirubin from the bloodstream and releases it into the intestinal tract. Before birth, a mother's liver removes bilirubin from the baby's blood. The liver of a newborn is immature and often can't remove bilirubin quickly enough, causing an excess of bilirubin. Jaundice due to these normal newborn conditions is called physiologic jaundice, and it typically appears on the second or third day of life. Because fetal circulation is less efficient at oxygen exchange than the lungs, the fetus needs additional RBC’s for transport of oxygen in utero. Therefore, at birth - - the average levels of RBC’s, hemoglobin, and hematocrit are higher and they fall slowly over the first month. Bilirubin is the substance that causes the yellow color of jaundice. It's a normal part of the waste produced when "used" red blood cells are broken down. RBC have short life span, when they die they release hematocrit, hematocrit is filtered by the liver, babies liver is not developed, liver cant filter fast enough causing jaundice Physiologic vs. Pathologic is usually depends primarily on time it appears and on the serum bilirubin levels. “Breastmilk Jaundice” - a term you may hear: Breastfeeding does not cause jaundice; lack of effective breastfeeding is what contributes to the hyperbilirubinemia Less caloric and fluid intake and possibly dehydration Hepatic clearance of bilirubin is reduced Fewer stools leading to bilirubin reabsorption from the intestine back into the bloodstream that must be conjugated again in order to be excreted Describe how to perform a physical assessment on a newborn, including the APGAR score. Jaundice is a yellow discoloration of the skin and eyes caused by hyperbilirubinemia (elevated serum bilirubin concentration). The serum bilirubin level required to cause jaundice varies with skin tone and body region, but jaundice usually becomes visible on the sclera at a level of 2 to 3 mg/dL (34 to 51μmol/L) and on the face at about 4 to 5 mg/dL (68 to 86 μmol/L). With increasing bilirubin levels, jaundice seems to advance in a head-to-foot direction, appearing at the umbilicus at about 15 mg/dL (258 μmol/L) and at the feet at about 20 mg/dL (340 μmol/L). This is not a reliable way to assess jaundice therefore TcB and TSB need to be assessed per protocol. Provide nursing care to assist with the newborn adaptation and to teach caregivers about newborn care. Describe nutritional needs of infants, anatomic and physiologic aspects of breastfeeding, newborn feeding-readiness cues, and maternal & infant indicators of effective breastfeeding. Infants should be breastfed as soon as possible after birth and at least 8 to 12 times per day thereafter Specific, measurable indicators show that the infant is breastfeeding effectively: 6-8 wet diapers & ≥3 stools every 24 hours (after day 4)