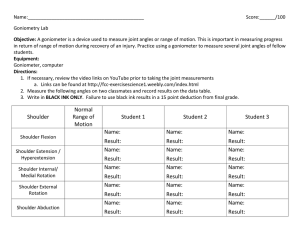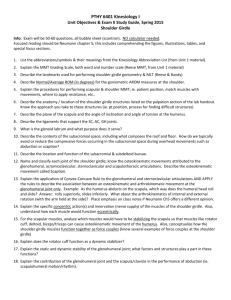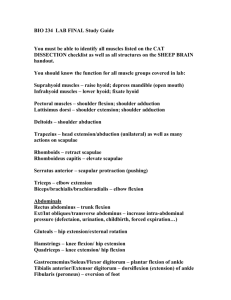
Muscle chart Comparing Myotomes- SCI vs Brachial Plexus Injury SCI With a SCI, the loss of motor and/or sensory function is due to damage to neural elements within the spinal canal. The ASIA Myotome Levels: The muscles were chosen because of their consistency for being innervated by the segments indicated and their ease of testing in the clinical situation, where testing in any position other than the supine position may be contraindicated. When using the ASIA, the motor examination is completed through the testing of key muscle functions corresponding to 10 paired myotomes (C5-T1 and L2-S1). It is recommended that each key muscle function should be examined in a rostral-caudal sequence, utilizing standard supine positioning and stabilization of the individual muscles being tested. Improper positioning and stabilization can lead to substitution by other muscles and will not accurately reflect the muscle function being graded. MYOTOMES • C5 – Elbow flexion • C6 – Wrist extension • C7 – Elbow extension • C8 – Finger flexion • T1 – Finger abduction • L2 – Hip flexion • L3 – Knee extension • L4 – Ankle dorsiflexion • L5 – Great toe extension • S1 – Ankle plantarflexion Brachial Plexus Injury With a brachial plexus lesion/injury it is the peripheral nerves outside the spinal cord that are being affected. The cervical and thoracic myotomes (C1-T12) are tested with the patient in a seated position. When testing for a brachial plexus lesion, you want to test movement(s) which have the strongest association with each myotome. Example: The primary muscles involved in the action of arm abduction include the supraspinatus, deltoid, trapezius, and serratus anterior. • Serratus Anterior, Deltoid- innervated by C5. • Cranial nerve XI innervates the motor function of the trapezius. • The supraspinatus muscle is supplied by the suprascapular nerve (C5 and C6) Technique for assessing C5 myotome with BPL C5- Shoulder abduction. Ask the patient to raise both their arms to the side of them simultaneously as strongly as then can while the examiner provides resistance to this movement. Compare the strength of each arm. MYOTOMES C5 – Shoulder abduction C6 – Elbow flexion Wrist extension C7 – Elbow extension C8 – Finger flexion T1 – Finger abduction L2 – Hip flexion L3 – Knee extension L4 – Ankle dorsiflexion L5 – Great toe extension S1 – Ankle plantarflexion Contractures A contracture is a limitation in active or passive range of motion that is caused by structural changes in the muscles, ligaments and/or tendons surrounding the involved joint. The primary cause of a contracture is loss of active motion due to another condition. Here is a partial list of conditions that can cause loss of active motion in all or portions of the upper extremities, leading to the possibility of contracture development: -CVA with hemiparesis -Traumatic brain injury The development of contractures leads to permanent loss of -Other chronic or progressive neurological conditions, such as multiple function, problems with hygiene and skin integrity, pain, and sclerosis, muscular dystrophy, amyotrophic lateral sclerosis, etc. difficulty with ADLs. Splinting is often used to help reduce -Alzheimer’s disease contractures. Please see the worksheet on splinting for these -Seizure disorder techniques. The treatment techniques listed below also help to -Cerebral palsy prevent contracture development and progression. Once an -Nerve lacerations effective contracture management program is developed for a -Brachial plexus injuries patient, the occupational therapist should educate caregivers on -Crush injuries the techniques required to continue the program daily. -Tendon and ligament injuries that do not receive timely or proper management -Dupuytren’s contracture -Burns Types of ROM Passive Range of Motion (PROM) – the amount of movement measured while the therapist moves the joint with no help from the patient. Active Range of Motion (AROM) – the amount of movement measured while the patient actively moves the joint. Active Assistive Range of Motion (AAROM) – the amount of movement measured while the patient actively moves the joint with gravity eliminated or with assistance from the therapist. Within Normal Limits (WNL) – range of motion is within the normal range of measurement for that specific joint. The therapist must measure the joint and compare it to the normative data. Within Functional Limits (WFL) – range of motion is functional for the particular tasks that the patient needs to complete. This can be different depending on the patient and what he or she needs to do. To determine that range is WFL, the therapist must observe functional movement and functional tasks, such as observing a patient getting dressed. Range of motion refers to the directions and limits of movement in each joint of the body. During evaluation, range of motion is measured using a full circle, half circle, or finger goniometer. To measure range of motion of a joint, the stationary arm of the goniometer is placed parallel to the longitudinal axis proximal to the joint, and the movable arm is placed parallel to the longitudinal axis distal to the joint. The goniometer must be placed in correct alignment with the joint for the measurement to be accurate. Measurements are always recorded in degrees of movement. Treatment Techniques to Increase Range of Motion Technique Description Example Photo/Video Passive The therapist moves the joint with no assistance from the patient. An occupational therapist A physical therapy The joint is moved until slight resistance is palpated and then the provides passive range position is held for several seconds before returning the joint to student of motion stretches to a demonstrates stretching the starting position. The patient may experience some mild discomfort at the end range during passive stretching if the joint is tight, but should not experience significant pain. patient who has left upper extremity hemiparesis resulting passive range of motion exercises. from a CVA. Active Range of Motion The patient actively moves the joint without assistance from the therapist. The patient may move the joint independently, or may move the joint during functional activities. Exercises/Ac tivities A patient reaches Demonstration of for cones placed activities that incorporate on a shelf to improve active -Tendon Gliding – specific AROM exercises that ensure adequate movement of the various tendons of the hand shoulder flexion. occupational therapy upper extremity active range of motion. A hand therapist demonstrates tendon within the structures of the hand. gliding exercises for patients to do at home. Active Assistive The patient actively participates in range of motion exercises with A patient pushes a towel A woman demonstrates Range of partial assistance from the therapist or with adaptations to the forward and back on a active assistive range of exercise set-up to eliminate gravity during the exercises. Active table top with both hands motion exercises, using Motion Exercises assistive range of motion exercises are completed when the patient has too much upper extremity weakness to allow for full active range of motion. to improve shoulder flexion. her stronger hand to help her weaker hand. Joint The therapist manually manipulates a joint to loosen the An occupational therapist Demonstration of mobilization ligaments holding the joint together to improve range of motion. applies joint mobilization The joint is stabilized on both sides. The joint is distracted by techniques to a patient’s joint mobilization to pulling the distal side away from the proximal side, then a small, index MP joint to improve the MP and IP gentle force is applied repeatedly in the direction of the desired index finger flexion. She joints. range. Joint mobilization is followed by passive stretching or follows joint mobilization with active range of motion exercises. active finger range of motion exercises. Scapula and Shoulder Movements The Shoulder Girdle The shoulder girdle, also called the pectoral girdle, is formed by: • the scapulae, posteriorly, • the clavicles anteriorly • manubrium of the sternum, anteriorly The girdle functions as the anchor that attaches the upper extremities to the axial skeleton. The glenohumeral joints/shoulder joints and the shoulder girdle work together in carrying out upper extremity activities. The shoulder girdle muscles – Stabilize the scapula so the shoulder joint will have a stable base from which to move the humerus – Contract to maintain the scapula in a relatively static position during shoulder joint actions – Contract to move the shoulder girdle and to enhance movement of upper extremity when the shoulder goes through extreme ranges of motion. Movements of the scapula The pectoral girdle or more specifically, the scapula movements includes: 1. Elevation: movement that allows the shoulder girdle to move upwards as in shrugging the shoulders. 2. Depression: the reverse of the elevation movement. The pectoral girdle and entire shoulder move downwards. 3. Scapular Abduction – also called scapular flexion or protraction. A movement where the scapula moves laterally away from the spinal column. 4. Scapular Adduction – also called scapular extension or retraction. This movement pulls the scapula back towards the rib cage. Pinching the shoulder blades together illustrates adduction of the shoulder girdle. 5. Downward rotation: rotating the lower scapula towards the rib cage as in moving the arm behind the back. Movements of the Shoulder 1. Forward Flexion – The anterior movement of the humerus or upper arm at the glenohumeral joint. 2. Extension – A posterior movement of the humerus at the glenohumeral joint. 3. Abduction– A movement of the arm away from the midsagittal plane of the trunk. This movement involves both glenohumeral joint motion and movement of the shoulder girdle. 4. Adduction – A movement of the arm toward the midsagittal plane of the trunk. 5. External Rotation – also called lateral or outward rotation. A movement around the long axis of the humerus at the glenohumeral joint . When the elbow joint is flexed to 90’ external rotation would cause the hand to move laterally or away from the midsagittal plane of the body. 6. Internal Rotation – also called medial or inward rotation. A movement around the long axis of the humerus causing the hand, with the elbow flexed to 90’ to move toward the midsagittal plane of the body. The Glenohumeral Joint The glenohumeral joint/shoulder joint allows a wide range of movements including flexion, extension, abduction, adduction, rotation (medial and lateral rotation), and circumduction. Instrumental Activities of Daily Living, or IADLs, are tasks that a person must complete to live independently in the community. Common IADL tasks include: • Meal preparation – includes tasks involved in preparing both cold and hot foods. • Household cleaning – includes sweeping, vacuuming, dusting, washing dishes, cleaning bathrooms, etc. • Yard work – includes mowing grass, raking leaves, pruning shrubs, and other tasks. • Clothing care/Laundry – includes washing, drying, folding and putting away clothing. • Time management – includes telling time, reading a calendar, following a schedule and making appointments. • Using communication devices – includes using a landline phone, cellphone, computer, intercom, and medical alert device. • Money management – includes counting and using money, managing bank accounts, and following a budget. • Community mobility – includes arranging for transportation, using public transportation, and locating various places in the community. • Shopping – includes identifying which stores sell specific goods, making shopping lists, and planning routes for shopping trips. • Managing medications – includes taking medications as prescribed, learning which medications treat which conditions, learning about possible side effects, and discussing medications with health care providers.