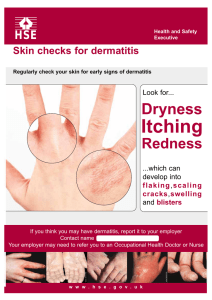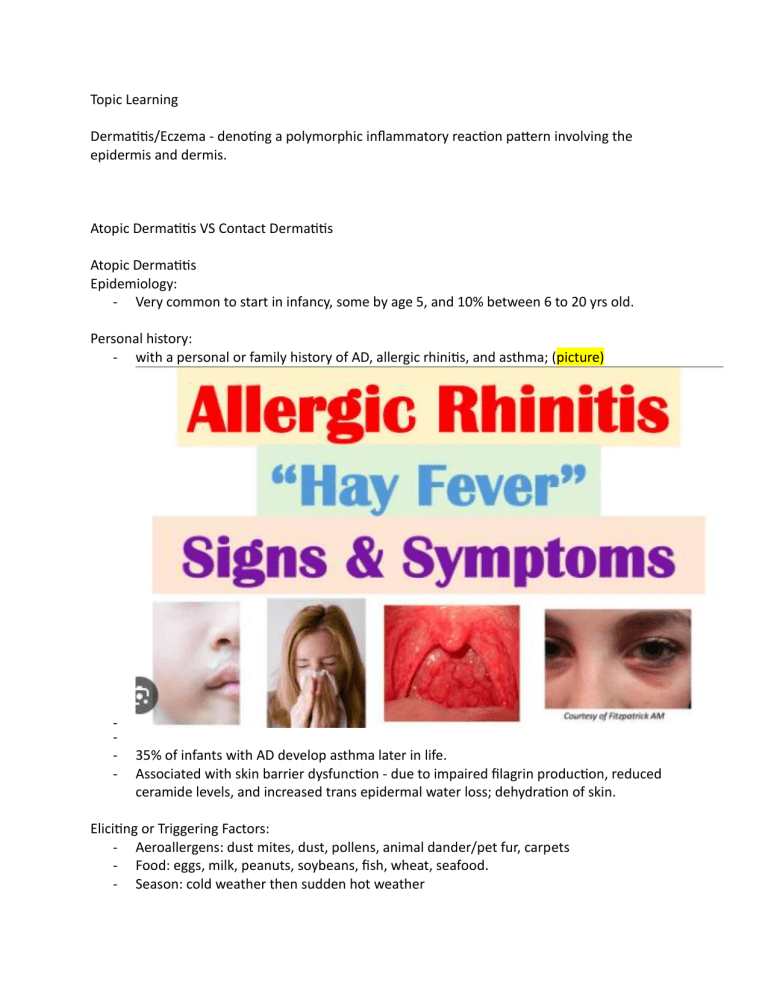
Topic Learning Dermatitis/Eczema - denoting a polymorphic inflammatory reaction pattern involving the epidermis and dermis. Atopic Dermatitis VS Contact Dermatitis Atopic Dermatitis Epidemiology: - Very common to start in infancy, some by age 5, and 10% between 6 to 20 yrs old. Personal history: - with a personal or family history of AD, allergic rhinitis, and asthma; (picture) - 35% of infants with AD develop asthma later in life. Associated with skin barrier dysfunction - due to impaired filagrin production, reduced ceramide levels, and increased trans epidermal water loss; dehydration of skin. Eliciting or Triggering Factors: - Aeroallergens: dust mites, dust, pollens, animal dander/pet fur, carpets - Food: eggs, milk, peanuts, soybeans, fish, wheat, seafood. - Season: cold weather then sudden hot weather - Clothing: pruritus AFTER taking clothing off (picture), - o wool clothing Emotional stress: can result from the disease or itself an exacerbating factor to more flare ups. Pathogenesis Complex interaction of skin barrier, genetic, environmental, pharmacologic, and immunologic factors. Type I (IgE-mediated) hypersensitivity reaction occurring as a result of the release of vasoactive substances from both mast cells and basophils that have been sensitized by the interaction of the inflammation in AD shows a biphasic pattern of T-cell activation. Clinical Manifestation: (Character of the skin) - Dry skin - Pruritus – - Itch scratch cycle – vicious - Acute (less than 6 months) – erythematous patches, papules, plaques o (picture) 2-12, 2-13, o o o consequent rubbing leads to increased inflammation and lichenification (picture) and to further itching and scratching leading to chronic AD. - Chronic (more than 6 months, YEARS) o Picture (2-14, 2-17 Distribution: (2-16, 2-17A B) o Flexures o front and side of the neck o forehead o face o wrists o dorsum of feet and hands Diagnosis - Medical History and clinical findings Laboratory Examinations - Bacterial Culture - Viral Culture - Blood Studies - Dermatopathology Course and Prognosis - In many patients, the disease persists for 15–20 years, but is less severe. Thirty to fifty percent of patients develop asthma and/or hay fever. Management - Baseline therapy of dryness with emollients - Picture of management - Contact Dermatitis Irritant Contact Dermatitis VS Allergic Contact Dermatitis Irritant – caused by chemical irritant Allergic – caused by an allergen – delayed and with immunologic reaction. Epidemiology: - Can happen to anyone and at any age. Predisposing Factors: - Atopic Dermatitis - Fare Skin - Cold weather - Humid weather - Occlusion - Mechanical Irritation Irritants or Allergens: - Abrasives, cleaning agents, - oxidizing agents; reducing agents, - plants and animal enzymes, secretions; - desiccant powders, dust, soils; - excessive exposure to water. Clinical Manifestation: (Character of the skin) IRRITANT CONTACT - Burning, stinging – can occur within seconds (immediate-type stinging), or can be delayed up to >24 hrs. - Erythema or vesiculation (picture) - Sharply demarcated and superficial edema - LESIONS DO NOT SPREAD BEYOND SITE OF CONTACT. ALLERGIC CONTACT - Less likely to be itchy - Itch scratch cycle – vicious - Acute (less than 6 months) – erythematous patches, papules, plaques o (picture) 2-12, 2-13, Diagnosis - Medical History and clinical findings Laboratory Examinations - Bacterial Culture - Viral Culture - Blood Studies - Dermatopathology Course and Prognosis - In many patients, the disease persists for 15–20 years, but is less severe. Thirty to fifty percent of patients develop asthma and/or hay fever. Management - Baseline therapy of dryness with emollients - Picture of management