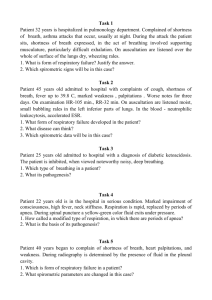
IN-CLASS/ONLINE CASE STUDY Chronic Obstructive Pulmonary Disease with Exacerbation Patient Profile D.B. is a 63-year-old electrician who came to the emergency department complaining of shortness of breath, morning cough, and swelling in his lower extremities. Subjective Data • Has smoked one pack of cigarettes daily for over 30 years • Has difficulty breathing when he walks • Has been sleeping in a recliner to make it easier to breathe • His shoes are tight at the end of the day Objective Data Physical Examination • Blood pressure 125/90, pulse 90, temperature 98.4° F, respirations 32 • Increased anterior-posterior diameter • Breath sounds diminished with prolonged expiration • 2+ peripheral edema bilateral lower extremities • Thin with muscle wasting • Respirations labored Diagnostic Studies • Arterial blood gases: pH 7.32, SaO2 86%, PaCO2 55 mm Hg, PaO2 70 mm Hg • Chest x-ray shows hyperinflation of lungs • FEV1 65% Discussion Questions 1. What in D.B.’s history is commonly associated with pulmonary problems? D.B has had a history of smoking for 30 years; the patient is experiencing shortness of breath, and labored breathing, has to sleep in a recliner to breathe better, has an increase in anteriorposterior diameter, and has diminished breath sounds with prolonged expiration. 2. Interpret D.B.’s arterial blood gases. pH is 7.32 is acidic, and PaCO2 is 55 mm hg indicating respiratory acidosis. Patient has respiratory acidosis. 3. 4. What is a likely medical diagnosis for D.B.? The patient has Chronic obstructive productive disorder. What assessment data and diagnostic study results led you to this diagnosis? The patient is experiencing COPD symptoms such as morning cough, shortness of breath, barrel chest, diminished breath sounds with prolonged expiration; the patient has a smoking history of 30 years. Chest X-rays show hyperinflation of the lungs, ABG shows respiratory acidosis in which the lungs are having trouble removing carbon dioxide, and FEV1 is 65% which is a percentage that indicates COPD. 5. What complication associated with this diagnosis does D.B. also have? What clinical manifestation led you to that and what is the cause of it? I believe D.B. could have a complication such as emphysema, and the reason I am making this diagnosis is due to the clinical manifestations such as labored breathing, shortness of breath, bilateral 2+ edema, elevated heart rate, and not being able to perfectly breathe appropriately laying down. This is caused due to inadequate gas exchange leading to excessive amounts o f carbon dioxide in the lungs. 6. What are the priority nursing diagnoses for D.B. at this time? The priority intervention is the risk of impaired gas exchange. 7. What interventions are indicated for D.B. and what outcome is expected for each intervention? Interventions that need to be done are to put the patient on a 2L nasal cannula to increase SatO2 levels and identify any potential irritants in the environment. Ensure D.B. get the annual flu vaccine to reduce the risk of infection in the lungs. 8. As part of patient teaching, is it “too late” to encourage D.B. to stop smoking? Why? Even though the patient has developed irreversible lung damage, the patient should still consider stopping smoking as this can help prevent further damage in the lungs. This includes destruction in the alveoli even further and making the patient's breathing even worse due to the inability of the lungs to exchange carbon dioxide. 9. What other teaching needs would you review with D.B. while he is hospitalized? It is important to teach patients about smoking cessation to prevent any further respiratory damage. The use of corticosteroids can also help with breathing. Having the patient perform exercises such as a spirometer to help to reduce CO2 in the body and how well the lungs are performing to reduce respiratory acidosis. Exercising 30 minutes a day can also help her improve breathing by the use of pursed lip breathing to reduce respirations.