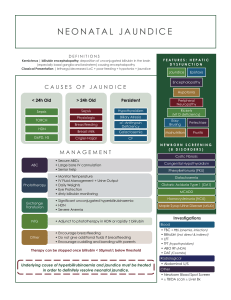
Let us first summarize what we talked about on Monday. Anybody in the group interested to the recap? In our previous session, we described jaundice as a yellowish coloring of the skin, sclerae, and mucous membrane brought on by an increase in the deposition of bilirubin and other yellow pigments. We have also listed some of the potential causes of jaundice, including hyperbilirubinemia, foods high in beta carotene like carrots, viral hepatitis, pre maturity, dehydration, biliary atresia, breastfeeding, genetic disorders and lastly liver diseases. We were also able to identify different anatomical structures that is related in the development of jaundice. Any one who can name some? So these are your spleen, liver, small intestine, large intestine, gall bladder, biliary tree that is composed of your (cystic duct, common bile duct, ampula of vater and common hepatic duct), we also have the skin, mucus membrane, sclera, brain, bone marrow and lastly the RBC’s. We also talked about the mechanism through which bilirubin is synthesized. So any one can have a quick discussion about it? 1. Hemoglobin from RBC --> unconj bilirubin (insoluble, binds to albumin) 2. Liver: bili conjugated with glucuronide by UDPGT, aka glucuronosyl transferase --> 3. Conjugated bili (water soluble) excreted into bile--> intestine 4. a) In adults, metabolized by the intestinal flora to urobilin --> stool 4. b) Newborn infant lacks GI flora to metabolize bile: Î2-glucuronidase in the meconium hydrolyzes the conjugated bilirubin back to its unconjugated form --> reabsorbed into blood, binds to albumin. Newborns absorb significant quantities of bilirubin through this process, known as enterohepatic circulation We were also able to classify the different causes of jaundice into pathologic and physiologic causes. So anyone can mention some pathologic and physiologic causes? That concludes the recap of the last session. Can we then move on to address our learning issues? Anyone who wants to answer our first learning issue. First in line is Kernicterus - bilirubin levels in the brain but first define what is kernicterus then give the mechanism. Kernicterus is the pathological term used to describe staining of the basal ganglia and cranial nerve nuclei by bilirubin. Kernicterus also describes the clinical condition that results from the toxic effects of high levels of unconjugated bilirubin Kernicterus, or bilirubin encephalopathy, is bilirubin-induced neurological damage, which is most commonly seen in infants. It occurs when the unconjugated bilirubin (indirect bilirubin) levels cross 25 mg/dL in the blood from any event leading to decreased elimination and increased production of bilirubin. The unconjugated bilirubin can cross the blood-brain barrier as it is lipid-soluble, unlike the water-soluble conjugated bilirubin. It gets deposited in the brain tissue, mainly the basal ganglia. Next is, Glucuronosyltransferase is same with glucuronyltransferase? Glucuronosyltransferase - Uridine diphosphate-glucuronyltransferase (UGT) is one kind of phase 2 enzyme, and genetic polymorphisms in the human UDP-glucuronosyltransferase-1A7 (UGTIA7) gene were detected. Glucuronyl transferase is a liver enzyme. It changes bilirubin into a form that can be removed from the body through the bile. It also changes some hormones, medicines, and toxins into non-harmful products. The skin can take on a yellow color (jaundice) if the body does not produce enough glucuronyl transferase. Then differentiate breastfeeding jaundice vs. breastmilk jaundice? 1. Breastfeeding jaundice aka "lack of breastmilk jaundice": - When does this occur? - Why does this occur? EARLY IN THE FIRST WEEK OF LIFE: milk supply is relatively or absolutely low --> limited enteral intake 2. --> decreased GI motility --> retention of meconium --> beta-glucuronidase in meconium deconjugates bilirubin and the unconjugated bilirubin is reabsorbed via the enterohepatic circulation, causing an elevation of serum levels. - Breast milk production typically increases greatly once "let-down" occurs. Occasionally, persistently low volume of breast milk can cause the neonate to become dehydrated and malnourished. Breastfeeding jaundice is often difficult to distinguish from physiologic jaundice. 2. Breast-milk jaundice: - When does this occur? How long can it persist? - Why does this happen? - How to tell apart from physiologic jaundice? - Begins in the first 4 to 7 days of life, may not peak until about 10 to 14 days. Can persist for up to 12 weeks, but total bilirubin concentration rarely, if ever, reaches concerning levels. - While the cause is not completely understood, one explanation is that beta-glucuronidase present in breast milk deconjugates bilirubin in the intestinal tract; the unconjugated bilirubin is then reabsorbed via enterohepatic circulation. The time course of breast-milk jaundice is quite different from that of physiologic jaundice. Then what are the different Genetic disorders that causes jaundice? And lastly how Cephalhematoma or bruises cause jaundice? A cephalohematoma (see photo) is a subperiosteal hemorrhage that is localized to the cranial bone that was traumatized during delivery. The swelling does not extend across a suture line. As the blood is reabsorbed from the cephalohematoma it will contribute to hyperbilirubinemia. - BRUISING on the head-or elsewhere on the body-from birth trauma or any other bleeding can also lead to increased bilirubin production because blood extravasated into tissues will be broken down and converted to bilirubin. So, is it all clear now? Any further information or explanation that we missed? If none let us proceed to our patient. So, anyone who can give the General information? So what is the chief complaint of our patient? How about the Gestational History of the mother Birth History Neonatal History Past Medical History Family History Socio economic So based on evidence from history what can we infer? Diagnostics: Serum bilirubin measurement • A visual estimate of bilirubin level is not a substitute for serum bilirubin levels as it can easily underestimate the true level of hyperbilirubinemia. Whenever there is concern about hyperbilirubinemia, a serum total bilirubin level should be obtained. Transcutaneous Bilirubin Measurement • Devices that measure transcutaneous bilirubin are effective tools for monitoring jaundice, although they cannot substitute for serum bilirubin levels. Newborn screening Etiology of hyperbilirubinemia: Age at which jaundice begins. Important why (2) Can help determine the risk for severe hyperbilirubinemia - Can direct you to specific causes of jaundice, especially hemolysis. Etiology of hyperbilirubinemia: Weight history. Important why? Inadequate weight gain indicates a potential insufficient fluid and calorie intake making a diagnosis of breastfeeding jaundice more likely. Etiology of hyperbilirubinemia: Feeding history Aids in distinguishing among possible causes of jaundice. Etiology of hyperbilirubinemia: Pregnancy history - Why is this important? 1. Maternal INFECTIONS may affect the fetus in utero --> congenital infection --> intrauterine growth restriction (IUGR). 2. The consequence may be a newborn who is born small for gestational age (SGA) with risk of direct hyperbilirubinemia. Etiology of hyperbilirubinemia: Signs of illness in the newborn - why important to ask about this? If jaundice only clinical finding, how likely is sepsis cause of hyperbili? Septic infants can have jaundice (with elevated total and direct bilirubin) as one sign of serious infection, along with other clinical manifestations, such as: Temperature instability, Respiratory distress, Apnea, Irritability, Lethargy, Poor tone, Vomiting, Poor feeding When jaundice is the only clinical finding, sepsis is highly unlikely as the cause of the increased bilirubin levels. Evaluation of neonatal hyperbilirubinemia - List 4 tests - When would you get them? 1. CBC and differential cell count 2. C-reactive protein 3. Blood cultures 4. Lumbar puncture with chemistry and cultures • If the jaundiced infant is ill or has other clinical signs suggesting possible infection. Jaundice as the only sign of sepsis would be rare. Evaluation of neonatal hyperbilirubinemia: Tests for congenital infections (TORCHS titers) • TORCHS titers test for congenital infections: Toxoplasmosis; Rubella; Cytomegalovirus; Herpes; and Syphilis. - Remember what the TORCH infections are? - When would you get titers for these?? Management of Jaundice in the Breastfed Infant - Should you stop breastfeeding since infants who are breastfed have higher incidence of hyperbili than formula fed babies? Obtain if the maternal history or infant's physical exam and clinical course suggested a congenital infection. • NO: stopping breastfeeding is NOT necessary in almost all cases, although some pediatricians will recommend temporary cessation of breastfeeding (for 24-48 hours) if breast milk jaundice causes extremely high bilirubin levels. American Academy of Pediatrics (AAP) discourages the interruption of breastfeeding by healthy term newborns with jaundice and encourages continued and frequent breastfeeding (at least 8 to 10 times every 24 hours).