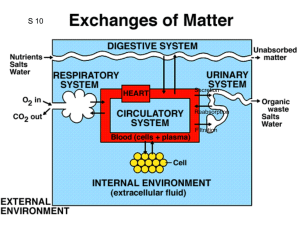
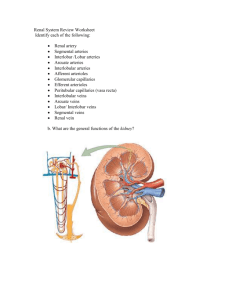
Chapter 19 Fluid, Electrolyte, and Acid-base Balance Percentages of Solutes in Body Fluids Solutes IC fluid Interstitial fluid Blood plasma K+ 75 3 3 Na+ 6 94 94 Ca++ 2 2 2 Proteins 27 traces 10 HCO3- 6 18 16 Chloride 2 77 69 Things to Know about Factors Affecting the Plasma Composition and Water Balance Solute and water content in plasma affected by movement of materials into and out of the body • Net gain of solutes and water due to the transport of molecules through the GI wall • Net loss of solutes and water due to the transport of molecules through the renal tubular walls Volume of plasma determined by its water content, affects directly MAP. Increased volume= increased MAP Plasma volume affects osmolarity (solute concentration). Increase of plasma water, decreases osmolarity. Decrease of plasma water, increases osmolarity Kidneys: control over the volume and composition of plasma by regulating solute and water composition • Principal cells: hormonal control of water and electrolyte balance • Intercalated cells: acid-base balance Material Exchanges Affecting Plasma Content Ingestion Lumen of digestive tract Excretion Feces Cells Absorption Secretion (Minimal) Extracellular connective tissue (including bone) Plasma and interstitial fluid (extracellular fluid) Filtration Secretion Reabsorption Lumen of renal tubules Other losses Excretion Sweating, hemorrhage, respiration Urine The Concept of Water Balance Output Input Input Output Output Input Increase No change Decrease Balance: Normovolemia = normal blood volume Positive balance: Hypervolemia = high blood volume due to positive water balance Negative balance: Hypovolemia = low blood volume due to negative water balance Continuous Fluid Movement In response of changes in relative osmolarityà Water moves by osmosis from hypotonic solution to hypertonic solution Fluid intake ànet movement of water from the blood plasma into the IC compartment Dehydrationà net movement of water from IC compartment into blood plasma Fluid Balance: Input + production = utilization + output Fluid Output (2500mL): Breathing, sweating, defecation, cutaneous transpiration (1000mL) Urination (1500mL) Fluid Intake (2500mL): Preformed water (2300 mL) Metabolic water (200mL) Factors Affecting Water Balance: Water intake + metabolically produced = water output + water used Cellular metabolism 0.3 L/day Ingestion 2.2 L/day Digestive tract Absorption Feces 2.2 L/day + 0.3 L/day = 2.5 L/day Filtration Total body water 42 L/day Secretion Excretion 0.1 L/day Water inputs = Secretion Renal tubules Reabsorption Other losses 0.9 L/day Insensible loss, sweating Excretion 1.5 L/day Urine Water outputs = 0.1 L/day + 0.9 L/day + 1.5 L/day = 2.5 L/day Fluid Output Obligatory • Expired air • Sweat • Cutaneous transpiration • Defecation • Minimum urine production • Abnormal: vomiting, blood loss Regulated • Hormonal stimulation of kidney Decreasing urine output: Aldosterone ADH Angiotensin II Increasing urine output: ANP Osmolarity and the Movement of Water Osmolarity of body fluids = 300 mOsm (300 milliosmoles of solute per liter of plasma) Under normal conditions: cell volumes don’t change and ICF and ECF are in osmotic equilibrium Water intoxication • Kidneys compensate for changes in osmolarity of extracellular fluid by regulating water reabsorption and adjusting the rate for water excretion • • Water reabsorption is a passive process, based on osmotic gradients. Coupled with electrolyte (Na+) reabsorption Water does not get secreted • • PCT: almost 70% of water is reabsorbed, unregulated DCT and collecting ducts: remaining water is reabsorbed, hormonal regulation Mechanism of Water Reabsorption in the Proximal Tubule Peritubular fluid Tubule epithelial cell Apical membrane Basolateral membrane Capillary endothelial cell Tubular fluid Plasma X Na+ Y X X Na+ K+ Na+ Y Y H2 O Permeating solute H2 O Permeating solute Steps for water and urea reabsorption: Solutes (Na+, X, Y) are actively reabsorbed, increasing the osmolarity of peritubular fluid and plasma. Creation of osmotic gradient Water is reabsorbed by osmosis, follows solute reabsorption Urea (permeating solute) is reabsorbed passively. Slide 1 Establishment of the Medullary Osmotic Gradient Osmotic pressure gradient: Responsible for water reabsorption by collecting ducts • near cortexà interstitial fluid osmolarity about 300 mOsm • near tips of medullary pyramidsà 1400 mOsm Due to countercurrent multiplier mechanism by loops of Henle and facilitated diffusion of urea (contributes about 40% to osmolarity of gradient) Vasa recta prevents the dissipation of osmotic gradient Medullary Osmotic Gradient Establishment of Medullary Osmotic Gradient by Countercurrent Multiplier Mechanism Vasa recta help to maintain the medullary osmotic gradient: The loss of water and gain of solutes that occurs as the descending limb goes toward the tip of the pyramid is counteracted by the gain in water and loss of solutes as the plasma ascends toward the cortex Water Reabsorption in DCT and Collecting Ducts • 20% water reabsorption by DCT and 10% in collecting ducts • Tubular fluid is hypo-osmolar compared to interstitial fluid • Epithelial cells are impermeable to water • Water channels/ aquaporins: type 3 in basolateral membrane and type 2 in apical surface activated by AntiDiuretic Hormone (ADH) • A. Water excreted in urine. High volume of low osmolarity urine • B. ADH presence. Water is reabsorbed. Urine isoosmotic to deep layer of medulla. Urine: small volume and high osmolarity Clinical Applications: Intravenous Solutions 0.9% saline solution • 0.9 g of NaCl to every 100 mL of sterile water 5% dextrose/ D5W • 5 g of dextrose to every 100L of sterile water • Standard for fluid replacement • Hypertonic solution to plasma when in holding bag but when infused à hypotonic • Similar osmolarity to plasma • Supplement for water and energy Sodium/Na+ • Principal cation of ECF in the form of NaCl and NaHCO3 • Exerts the greatest osmotic pressure in ECF that drives water reabsorption • 135-145 mEq/L • Daily requirement 1.5 to 2.3 g (0.5 – 20-25g) (3-7 g) • Determines blood plasma osmolarity and regulates fluid balance • Retention of Na+ and waterà increases BV and BP • Na+ reabsorption in proximal tubules unregulated • Na+ reabsorption in distal tubules regulated by ADH, aldosterone, and ANP • Na+ imbalance: hypernatremia and hyponatremia Mechanisms of Sodium Reabsorption in the Renal Tubule • Freely filtered • Control of Na+ levels is important in blood pressure and blood volume • Reabsorbed (70%) in proximal tubules, distal tubules, and collecting ducts • No secretion • Reabsorption regulated by aldosterone and ANP at principal cells of distal tubules and collecting ducts In PCT: • Na+/K+ pump on basolateral membrane drives active reabsorption • Na+ crosses apical surface: Na+/Glucose/ amino acids cotransport and Na+/H+ counter-transport In DCT: • Na+/K+ pump in basolateral surface • Na+/ Cl- and HCO3 cotransport and facilitated diffusion through Na+ channels Na+ Reabsorption in Renal Tubules Mechanisms of sodium reabsorption in the proximal and distal tubules Peritubular fluid Apical membrane Proximal tubule epithelial cell Capillary endothelial cell Basolateral membrane Tubular fluid Plasma X Na+ X Na+ Na+ H+ Cl– Sodium reabsorption in the proximal tubule Na+ K+ Mechanisms of sodium reabsorption in the proximal and distal tubules Distal tubule epithelial cell Cl– Na+ Na+ Na+ K+ Cl– K+ Cl– Na+ Sodium reabsorption in the distal tubule Cl– The Effects of Aldosterone Action: Increases sodium reabsorption and secretion of K+ • Acts on principal cells of distal tubules and collecting ducts – Increases number of Na+/K+ pumps on basolateral membrane and open Na+ and K+ channels on apical membrane • Stimuli for renin release – Decreased pressure in afferent arteriole – Renal sympathetic nerve activity – Decreases in Na+ and Cl– in distal tubule filtrate Effects of Aldosterone on Principal Cells of the Distal Tubules and Collecting Ducts Lumen of late distal tubule or collecting duct Basolateral membrane Peritubular fluid Peritubular capillary Principal cell Apical membrane Na+ Cytosolic receptor Aldosterone K+ K+ Na+ Na+ Tubular fluid K+ K+ K+ K+ K+ K+ Na+ Na+ Na+ Na+ Na+ Plasma Interactions Between Fluid and Electrolyte Balance • Physiological response to hemorrhage – Decrease in blood volume ® decrease in MAP – Neural control of heart and vasculature • Baroreceptor reflex – Hormonal control of blood volume: o Increase in solute reabsorption increases osmotic gradient for water reabsorption • ADH: increases the number of sodium channels in the apical membrane of principal cells • Angiotensin II increases ADH secretion • Renin-angiotensin-aldosterone system (RAAS) • Atrial natriuretic hormone: decreases ADH secretion Juxtaglomerular Apparatus JG / granular cells: enlarged smooth muscle cells in wall of arteriole, granules with renin. Mechanoreceptors (baroreceptors) Macula Densa: tall, closely-packed cells in DCT adjacent to the granular JG cells. Chemoreceptors (NaCl ). Sensor for tubuloglomerular feedback The Renin-Angiotensin-Aldosterone System (RAAS) Decrease in plasma Na+à fall in blood volumeàGranular/JG cells secrete reninà Angiotensinogen into angiotensin Ià Angiotensin-converting enzyme (ACE) converts into angiotensin IIà Stimulates aldosteroneà Promotes the reabsorption of Na+ and secretion of K+ àIncreases blood volume and raises blood pressure RAAS System Mechanisms by which Decreases in MAP Stimulate Renin Release MAP Afferent arteriole pressure Baroreceptor reflex Sympathetic activity GFR [Na+] and [Cl–] in distal tubules Macula densa Paracrine secretion Juxtaglomerular cells of afferent arteriole Renin release Initial stimulus Physiological response Result Slide 1 Mechanisms by which Angiotensin II Increases MAP Angiotensin II Systemic arterioles Vasoconstriction Adrenal cortex Posterior pituitary Hypothalamic neurons Aldosterone secretion ADH secretion Thirst stimulation Kidneys Sodium reabsorption in late distal tubules and collecting ducts Extracellular fluid osmolarity MAP Initial stimulus Physiological response Result Water reabsorption in late distal tubules and collecting ducts Plasma volume Slide 1 Control of Aldosterone Rise of K+ in plasma Depolarization of aldosterone– secreting cells Low Na+ in plasma Fall in blood volume àRenin – AngiotensinAldosterone system Atrial Natriuretic Peptide Secreted by atrial cells in response to distension of atrial wall o Increases GFR • Dilation of afferent arteriole • Constriction of efferent arteriole o Decreases Na+ reabsorption by closing Na+ channels in apical membrane o Inhibition of secretion of ADH, renin, and aldosterone o Endogenous diuretic Atrial Natriuretic Peptide Increased BV Decreased BP Stretch of atria ANP release Decreased BV Decreased reabsorption of Na+ and water Mechanisms by which Secretion of Atrial Natriuretic Peptide Increases Sodium Excretion in Response to Increased Plasma Volume Plasma volume Atria Atrial wall stretch ANP secretion Kidneys Afferent arteriole dilation Efferent arteriole constriction Na+ reabsorption Renin secretion Glomerular capillary pressure GFR Initial stimulus Physiological response Result Na+ excretion Aldosterone Slide 1 Potassium/K+ o Abundant in ICF o 3.5-5.0 mEq/L o Control of K+ levels is important in healthy skeletal and cardiac muscle activity o Hormonal regulation of K+ in blood plasma by aldosteroneà increases K+ secretion and excretion o K+ imbalance: the most lethal of electrolyte imbalancesà cardiac or respiratory arrest o Distribution: K+ shifts between ECF and ICF due to concentration in blood plasma, concentration of H+ in plasma, and insulin (decreases glucose and K+ in blood) Renal Handling of Potassium Ions • Glomerulus: freely filtered • Proximal tubules: reabsorbed • Distal tubules and collecting ducts: reabsorbed and secreted • K+ secretion in distal tubules and collecting ducts is regulated • Aldosterone regulates principal cells • As K+ increases in plasmaà stimulation of aldosterone release Potassium Reabsorption in Renal Tubules Apical membrane Basolateral membrane Proximal tubule epithelial cell Lumen of proximal tubule K+ Unknown mechanism ? K+ Na+ K+ K+ Tubular fluid Potassium reabsorption in the proximal tubule K+ Peritubular fluid K+ Secretion Secretion matches ingestion DCT and cortical collecting duct Types: o Aldosterone-dependent: ingestionà high K+ in bloodà aldosterone secretionà K+ secretion o Aldosterone-independent: rise (fall) in blood K+ à insertion (removal) of K+ channels in collecting duct Potassium Secretion in Renal Tubules Apical membrane Basolateral membrane Principal cell Lumen of late distal tubule or collecting duct K+ Na+ K+ Tubular fluid Peritubular fluid Potassium secretion in the principal cells of the late distal tubule and collecting duct Calcium Balance • Hypercalcemia: high plasma calcium • Hypocalcemia: low plasma calcium Critical function: – Exocytosis – Secretion – Muscle contraction – Increases contractility of cardiac and smooth muscle Routes of Calcium Exchange Bone Calcification (calcitonin) Ingestion Digestive tract Absorption (1,25-(OH2)D3) Resorption (PTH, 1,25-(OH2)D3) Plasma [Ca2+] Filtration Reabsorption (PTH stimulates, calcitonin inhibits) Kidneys Renal Handling of Calcium Blood calcium – Bound to carrier proteins – Free in plasma – Ca2+ + protein Ca-protein – Free calcium: freely filtered at glomerulus – 99% of filtered calcium is reabsorbed: • 70% is reabsorbed in PCT • 19–20% is reabsorbed in thick ascending limbs of the loops of Henle. Regulated • 9–10% is reabsorbed in DCT. Regulated Hormonal Control of Plasma Calcium Concentrations: Parathyroid Hormone (PTH) • Stimulus: decreased Ca2+ in plasma • Actions – Increases Ca2+ reabsorption by kidneys – Stimulates activation of 1,25dihydroxycholecalciferol in kidneys – Stimulates reabsorption of bone – Stimulates small increase in calcium absorption – Overall effect: increased blood calcium Role of Parathyroid Hormone in Calcium Balance Slide 1 [Ca2+] in plasma Parathyroid glands PTH secretion Negative feedback [PTH] in plasma Kidneys Phosphate reabsorption Ca2+ reabsorption Calcium excretion in urine Bone 1,25-(OH2)D3 activation Ca2+ resorption [1,25-(OH2)D3] in plasma Negative feedback Kidneys Gastrointestinal tract Ca2+ absorption Initial stimulus Physiological response Result [Ca2+] in plasma Hormonal Control of Plasma Calcium Concentrations: Calcitonin –Secreted from C cells of thyroid gland –Release triggered by high plasma [Ca2+] –Actions at target cells • Increases bone formation • Decreases calcium reabsorption by kidneys Acid-Base (pH) Balance Requires the regulation of H+ concentration in body fluids in order to maintain arterial blood pH= 7.35-7.45 pH < 7.35 = acidosis pH > 7.45 = alkalosis H+ concentration altered by: 1. Chemical buffers 2. Respiratory rate 3. Input and output of acids and bases Compensation for Acid-Base Disturbances • Henderson-Hasselbalch equation pH = 6.1 + log [HCO3–] [CO2] • For pH = 7.4, [HCO3–]/[CO2] = 20:1 • Acidosis: [HCO3–]/[CO2] < 20:1 • Alkalosis: [HCO3–]/[CO2] > 20:1 • Kidneys regulate HCO3– • Lungs regulate CO2 Inputs and Outputs of Acids to the Blood Input Diet Metabolism Output Proteins Fats CO2 Lactic acid Keto acids H+ Kidneys CO2 Lungs Blood [H+] pH Balance in the Body © 2016 Pearson Education, Inc. Acid-Base Disturbances Respiratory Disturbances Carbon dioxide is a source of acid CO2 + H2Oà H2CO3 àHCO3– + H+ Normal PCO2 arterial blood = 40 mm Hg Sources of CO2: metabolism Output of CO2 through respiratory system Hypoventilationà Increased plasma [CO2] ® Respiratory acidosis Hyperventilationà Decreased plasma [CO2] ® Respiratory alkalosis Metabolic Disturbances o Metabolic Alkalosis ü Increased pH Excessive vomiting Consumption of alkaline products (baking soda) Alterations in renal function (increased H+ secretion/ HCO3- reabsorption) o Metabolic Acidosis üDecreased pH High-protein diet High-fat diet Heavy exercise Severe diarrhea (loss of bicarbonate) Renal dysfunction (decreased H+ secretion/ HCO3 reabsorption) Complications with A-B Disturbances Acidosis Alkalosis Denatures proteins Decreases excitability of neurons: confusion, coma, and death Increases excitability of neuron Retention of K+ K+ depletion Cardiac arrhythmias Vasodilation Generation of APs in sensory and motor neurons Defense Mechanisms Against AcidBase Disturbances Renal compensation Buffering of hydrogen ions Respiratory compensation: corrects 75% of A-B disturbances Adjustments to pH Changes 1. Buffering H+ ions: the quickest defense ECF buffer: HCO3ICF buffers: phosphate (HPO42– + H+ àH2PO4–) and proteins 2. Respiratory compensation: within minutes pH decreasesà hyperventilationà decrease of pCO2àremoval of H+àpH increases pH increasesà hypoventilationà increase of pCO2à addition of H+à pH decreases The Mechanism by which Decreases in Plasma pH Increase Ventilation Plasma pH ( acidity) Peripheral chemoreceptors Detect and respond Ventilation Plasma PCO2 Plasma pH Initial stimulus Physiological response Result Negative feedback Adjustments to pH Changes 3. Renal Compensation: hours to days. Regulates hydrogen ions and bicarbonate in urine – Proximal tubule • Bicarbonate reabsorption coupled to hydrogen secretion – Distal tubule and collecting duct • Secretion of hydrogen coupled to synthesis of new bicarbonate ions Low pH (high H+ concentration)à increased reabsorption of HCO3 and secretion of H+à pH increases High pH (low H+ concentration)àdecreased HCO3 reabsorption and secretion of H+à pH decreases Bicarbonate Reabsorption and Hydrogen Ion Secretion in the PCT Proximal tubule epithelial cell H+ H+ H+ + HCO3– (secreted) (filtered) H2CO3 H2O + CO2 Tubular fluid K+ Na+ H+ CO2 + H2O H2CO3 CA CA HCO3– Na+ Na+ HCO3– Cl– HCO3– Peritubular fluid Bicarbonate synthesis and hydrogen ion secretion by intercalated cells of the distal tubule and collecting duct. Intercalated cell Tubular fluid Peritubular fluid H+ H+ H+ + HPO42– H2PO4 – H+ H+ K+ CO2 + H2O Cl– H2CO3 CA HCO3– Cl– HCO3– Adjustments to pH Changes • Glutamine in renal compensation –Severe acidosis Glutamine metabolism produces new bicarbonate and secretes hydrogen in the form of ammonium Bicarbonate production and hydrogen secretion by glutamine metabolism in the proximal tubule. Peritubular fluid Tubular fluid NH4+ Na+ NH3 + H+ NH4+ K+ Glutamine HCO3– H+ Na+ Cl– Na+ Na+ HCO3– HCO3– Acidification of the Urine Compensation for Acid-Base Disturbances • Respiratory alkalosis – Cause: hyperventilation – Decreased CO2 ® decreased H+ – Compensation: renal • Decreased H+ secretion • Decreased HCO3– reabsorption • Respiratory acidosis – Cause: hypoventilation – Increased CO2 ® increased H+ – Compensation: renal • Increased H+ secretion • Increased HCO3– reabsorption Compensation for Acid-Base Disturbances • Metabolic acidosis – Cause: increased H+ independent of CO2 – Compensation: respiratory and renal (unless renal problem) – Respiratory compensation • Increased ventilation ® decreased CO2 – Renal compensation • Increased H+ secretion • Increased HCO3– reabsorption • Increased synthesis of new bicarbonate Compensation for Acid-Base Disturbances • Metabolic alkalosis – Cause: decreased H+ independent of CO2 (increased HCO3-) – Compensation: respiratory and renal (unless renal problem) – Respiratory compensation • Decreased ventilation ® increased CO2 – Renal compensation • Decreased H+ secretion • Decreased HCO3– reabsorption • Decreased synthesis of new bicarbonate Summary of acid-base disturbances and compensation Slide 1 Arterial pH pH < 7.35 OR pH > 7.45 Acidosis [HCO3–] < 24 mM Metabolic acidosis Respiratory compensation PCO2 < 40 mm Hg OR Alkalosis PCO2 > 40 mm Hg [HCO3–] > 24 mM Respiratory acidosis Metabolic alkalosis Renal compensation [HCO3–] > 24 mM Respiratory compensation PCO2 > 40 mm Hg OR PCO2 < 40 mm Hg Respiratory alkalosis Renal compensation [HCO3–] < 24 mM Relationship between Na+, K+, and H+ • Reabsorption of Na+ stimulates the secretion of K+ and H+ • Low pH stimulates the secretion of H+ and inhibits the secretion of K+; acidosis can lead to hyperkalemia • Hyperkalemia stimulates the secretion of K+ and inhibits secretion of H+; can lead to acidosis • High pH stimulates the secretion and excretion of more K+ Reabsorption of Na+ and Secretion of K+, and H+ Blood Volume Reflex Low BV Baroreceptors and stretch receptors Posterior pituitary: ADH Increased BV Decreased water secretion Collecting ducts: increased water reabsorption Blood Osmolarity Low water intake Elevation of osmolarity Osmoreceptors in liver and hypothalamus Increased water reabsorption and constriction of arteriolesà fluid reabsorption Increased secretion of ADH Increased thirst and fluid intake Decreased water excretion Use of Diuretics • BP control and treatment of edema • Increase urine volume, decreasing blood volume and interstitial fluid volume