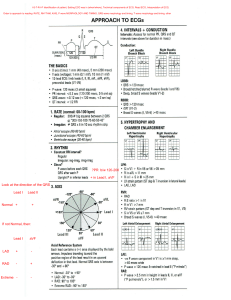
BASIC ECG, CARDIAC ARRYTHMIAS Ranulfo Javelosa, Jr., M.D. November 09, 2010 LEGEND Normal text : lecture ppt, 2011B trans, Guyton and ECG Made Easy Italicized: AUDIO INTRODUCTION Augustus Waller – introduced the concept that the heart has electrical potential The ECG provides information for: Rhythm Rate Enlargement Injury/infarction REVIEW Phase 0 is the upstroke of the action potential (depolarization) If upstroke is due only to ICa, it will be slow If the upstroke is due to both ICa and INa, it will be fast. Corresponds to the onset of QRS Factors that decrease the slope of phase 0 by impairing the influx of Na+ (e.g., hyperkalemia, or drugs such as flecainide) tend to increase QRS duration Phase 1 The rapid repolarization component of the action potential (when it exists) due to almost total inactivation of INa or ICa, and may also + depend on the activation of a minor K current not listed previously, called Ito (for transient outward current). Phase 2 plateau phase of the action potential, which is prominent in ventricular muscle 2+ + depends on the continued entry of Ca or Na ions through their major channels, and on a minor membrane current due to the Na-Ca exchanger corresponds to the isoelectric ST segment conditions that prolong phase 2 (use of amiodarone, hypocalcemia) increase the QT interval shortening of this phase, as by digitalis administration or hypercalcemia, abbreviates the ST segment Phase 3 repolarization component of the action potential It depends on IK Corresponds to the inscription of the T wave Phase 4 constitutes the electrical diastolic phase of the action potential In SA and AV nodal cells, changes in IK, ICa, and If produce pacemaker activity during phase 4 Purkinje fibers also exhibit pacemaker activity, but use only I f Atrial and ventricular muscle have no time-dependent currents during phase 4 Transmembrane potential (Ventricular Muscle). (What goes in, what goes out of membrane potential) Underlying cardiac potentials are 4 major time-dependent and voltage-gated membrane currents: + 1. The Na current (INa) is responsible for the rapid depolarizing phase of the action potential in atrial and ventricular muscle and in Purkinje fibers. It is also the largest current in the heart. 2. The Ca2+ current (ICa) is responsible for the rapid depolarizing phase of the action potential in the SA node and AV node; it also triggers contraction in all cardiomyocytes. It passes primarily through L-type Ca2+ channels. + 3. The K current (IK) is responsible for the repolarizing phase of the action potential in all cardiomyocytes. 4. The "pacemaker current" (If) is responsible, in part, for pacemaker activity in SA nodal cells, AV nodal cells, and Purkinje fibers. It is mediated by a nonselective cation channel. Sinoatrial (SA) node / Sinus node Located in the R atrium Primary pacemaker Cells fire spontaneously; i.e., they exhibit automaticity Atrioventricular (AV) node Located near the atrioventricular groove and the tricuspid valve Secondary pacemaker Purkinje fibers For rapid conduction of action potentials Tertiary pacemaker Any pathologies in the tricuspid, R atrium, septum, would affect this part of the conducting system TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 1 of 16 The bundle branches would be running along the surface of the interventricular septum. Therefore, congenital heart diseases like VSD, ASD, could affect this flow of electricity. When AV valves (tricuspid and mitral) close, you have the S1, and this is at the same time as QRS also. Rapid ejection phase and then the depolarization. The T wave, you have the repeat of the cycle during diastole. Atrial excitation – p-wave Atrial systole at the beginning of the Q Ventricular excitation – QRS Ventricular systole after T wave Ventricular diastole – U wave Step I. Rapid filling of ventricles Ventricular pressure drops below atrial pressure AV valves are open, semilunar valves are closed Rapid ventricular filling occurs 70-90% of the ventricles fill with blood CARDIAC CYCLE Aortic valve closure Aortic valve opening ↑ in ventricular pressure Step II. Atrial systole P wave occurs Atrial contraction – lateral 1/3 of diastole Pushed 10-30% more blood into ventricle *timing of complexes to the clinical events (heart sounds) S4 – atrial contraction after p-wave P-wave – atrial depolarization After atrial excitation, atrial contraction follows After ventricular excitation ventricular contraction tricuspid and mitral valve closure S1 S2 and S3 comes after the p-wave P to beginning of R-wave – diastole QRST – systole Step III. Isovolumetric contraction QRS just occurred Contraction of the ventricles causes ventricular pressure to rise above atrial pressure AV valves close Ventricular pressure is still less than aortic pressure Semilunar valves are closed Volume of blood in the ventricle is EDV Step IV. Ejection Contraction of the ventricles causes ventricular pressure to rise above aortic pressure, Semilunar valves open Ventricular pressure is greater than atrial pressure AV valves are still closed Volume of blood ejected by the ventricles: stroke volume (SV) TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 2 of 16 of that lead, and a negative deflection if the wave spreads toward the negative pole. If the mean orientation of the depolarization vector is at right angels to a given lead axis, a biphasic (equally positive & negative) deflection will be recorded Step V. T-wave occurs Ventricular pressure drops below aortic pressure Back pressure causes semilunar valves to close Step VI. Isovolumetric relaxation AV valves are still closed Semilunar valves are still closed Volume of blood in ventricles: ESV Ventricular pressure drops P Q R Limb Leads Record potentials transmitted onto the frontal plane 3 standard “bipolar” leads (I, II, III) and 3 augmented “unipolar” leads (aVR, aVL, aVF) S T U ECG ECG Leads Configured so that a positive (upright) deflection is recorded in a lead if a wave of depolarization spreads toward the positive pole TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 3 of 16 Atrial repolarization is usually too low in amplitude to be detected, but it may become apparent in such conditions as acute pericarditis or atrial infarction PR interval – should not be >1 big square From the start of the P to the start of the Q or R wave Prolongation is used in assessing AV blocks or conduction defects Normally 120-200msec Measures the time bet. atrial and ventricular depolarization, w/c includes the physiologic delay imposed by stimulation of cells in the AV junction area. Chest / Precordial Leads (6) Surround the heart to pick up activity of different chambers Record potentials transmitted onto the horizontal plane V1 – 4th ICS, R parasternal border Near to R ventricle th V2 – 4 ICS, L parasternal border V3 – b/w V2 & V4 Closest to L ventricle th V4 – 5 ICS, LMCL th V5 – 5 ICS, LAAL Nearest the septum V6 – 5th ICS, LMAL Inferior leads (for inferior wall infarction): II, III, aVF Lateral leads (lateral wall problems): I, aVL, V5, V6 Anterior leads (ant. wall infarction): V1 to V4 V1 and V2 – for RV hypertrophy, infarction V5 and V6 – for LV infarction, enlargement, hypertrophy QRS interval – should not be >3 small squares (~2.5small squares) Normally 100-110 ms or less Prolongation could mean a delay of propagation of impulse in the ventricles Reflects the duration of ventricular depolarization QT interval Includes both ventricular depolarization & repolarization times and varies inversely with the heart rate R-R interval – interbeat interval SEQUENCE OF ECG INTERPRETATION THE NORMAL ECG Paper speed: 25mm/sec Vertical Axis 1 small square = 1mm (0.1mV) 1 large square = 5mm (0.5mV) 2 large squares = 1mV Horizontal Axis 1 small square = 0.04sec 1 large square = 0.2sec 2 large squares = 1sec ECG Waveforms & Intervals P wave = atrial depolarization Normal atrial depolarization vector is oriented downward & toward the subject’s left, reflecting the spread of depolarization from the sinus node Since this vector points toward the positive pole of lead II & toward the negative pole of lead aVR, the normal P wave will be positive in lead II & negative in lead aVR. QRS complex = ventricular depolarization Normal ventricular depolarization proceeds as a rapid, continuous spread of activation wavefronts ST-T-U complex (ST segment, T wave, and U wave) = ventricular repolarization 1. 2. 3. 4. 5. 6. 7. Rate Rhythm Axis Hypertrophy Infarction Injury Ischemia Interpretation Sequence Check the patient details—is the ECG correctly labelled? o Are the electrodes correctly placed? o Interchanged electrodes reversed polarity What is the rate? Is this sinus rhythm? If not, what is going on? What is the mean frontal plane QRS axis? (You may wish at this stage to glance at the P and T wave axes, too.) Are the P waves normal (Good places to look at are II and V1) What is the PR interval? Are the QRS complexes normal? Specifically, are there: o Significant Q waves o Voltage criteria for LV hypertrophy o Predominant R waves in V1 o Widened QRS complexes Are the ST segments normal, depressed, or elevated? Quantify the abnormalities. Are the T waves normal? What is the QT interval? Are there abnormal U waves? TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 4 of 16 Step 1: RATE Identify an R wave that falls on the marker of a ‘big block’ Each large square (5mm) represents 0.2 seconds, so there are five large squares per second, and 300 per minute. Count the number of the big blocks to the next R wave 300 ÷ # of big squares 1500 ÷ # of small squares Relationship Between the Number of Large Squares Covered by the R-R Interval and the Heart Rate R-R Interval (Large Squares) Heart Rate (beats/minute) 1 300 2 150 3 100 4 75 5 60 6 50 What is the Rate? 18 small squares: 1500/18 = 83bpm The normal pacemaker is the SA node; the signal then propagates through the AV node, and activates the ventricles. When the heart follows this pathway at a normal rate and in this sequence, the rhythm is called a "normal sinus rhythm." SA Node: 60-100bpm AV Node: 40-60bpm Ventricular: no p-wave, <40bpm Normal Sinus Rhythm Sinus rhythm: when depolarization begins in the sinoatrial (SA) node Normal Sinus Rhythm elements: R-R measurement Should be the same P-P measurement P-P to R-R measurement Should have a constant PR interval QRS interval should be <0.12s P should always be followed by QRS P wave should be identical, upright, uniform and occurring regularly P always followed by a QRS 3 big squares: 300/3 = ~100bpm 4 big squares: 300/4 = ~75bpm 19 small squares: 1500/19 = 79bpm Junctional Rhythm originate at AV node with retrograde and anterograde direction Normal/narrow QRS P-wave may be absent or may show after QRS HR is slow (40-60bpm) can be due to β-blocker, digitalis toxicity, myocarditis, dengue fever, R Coronary branch occlusion Step 2: RHYTHM Sinus? Junctional (AV node)? Ventricular? Pacemaker? Atrial fibrillation? Ventricular Fibrillation? TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 5 of 16 7 big squares: 300/7 = 42bpm Nodal Escape: if region around the AV node takes over as the focus of depolarization Rate is 100/minute No P waves in junctional beats (indicates either no atrial contraction or P wave lost in QRS complex) Normal QRS complexes Ventricular Rhythm originate from purkinje fibers Wide QRS Impulse originates from one side of the ventricle causing prolonged/delayed activation of the ventricles No P-wave HR is slower (40-60bpm) Ventricular Escape most commonly seen when conduction between the atria and ventricles is interrupted by a complete heart block After three sinus beats, the SA node fails to discharge. No atrial or nodal escape occurs. After a pause, there is a single wide and abnormal QRS complex with an abnormal T wave 8 small squares: 1500/8= 188bpm Pacemaker Rhythm Impulses originate at transvenous pacemaker Wide QRS Pacemaker spikes Ventricular rhythm with faster HR No p-wave 8.5 big squares: 300/8.5 = 35bpm 8.5 big squares HR: 150bpm (for figure below) MI, metamphetamine, drugs Patient can collapse Can be tolerated in younger individuals If with pulse and normal BP, give anti-arrhytmics If no pulse is detected, start CPR and defibrillate Spike R S T Ventricular Tachycardia No P waves Regular QRS complexes, rate 200/minute Broad QRS complexes, duration 240 milliseconds with a very abnormal shape No identifiable T waves Atrial Fibrillation (AF) ECG has many but not identical P waves RR interval is not constant TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 6 of 16 Usually 5-10 P: 1 QRS Irregularly irregular rhythm HR variable Causes: drugs, alcohol, ischemia, metabolic disturbances, heart failure, dilatation, HTN Aka “Holiday Heart Syndrome” Step 3: QRS AXIS The subtotal of the direction of the electrical activity of the heart; normally, downward and to the left Frontal QRS Axis Course vs. Fine Fibrillation Baseline coarsely or finely irregular; P waves are absent. Ventricular (QRS) irregular, slow or rapid Atrial Flutter 4P : 1 QRS Saw-toothed configuration of the p-waves Regular RR intervals TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 7 of 16 Wolff-Parkinson-White syndrome – right-sided accessory pathway Tricuspid atresia Ostium primum - OSD Northwest territory – both lead I and aVF (-) Causes: Emphysema Hyperkalemia Lead transposition Artificial cardiac pacing Ventricular tacchycardia Normal Using leads I and aVF, the axis can be calculated to within one of the four quadrants at a glance. Shortcut: 1. You normally look at leads I and aVF. 2. Hold the results of lead I of the ECG with your left hand and that of the aVF with your right. 3. With the index finger and middle finger of each hand, follow the deflection of the waves (upward = +, downward = -) found in the corresponding leads. 4. If both point upward, then it is normal. If both point downward, then it is NW axis deviated. 5. If one is positive and the other is negative, then the opposite of the hand holding the negative is the side where the deviation is (in short, the one holding the upward deflection is the side of the deviation) Right Axis Deviation Another way (for the mathematically gifted): 1. Plot the heights of the deflection of waves - + + 2. Get the vector - + + 3. Report in degrees of deviation Left Axis Deviation The QRS Axis Normal Axis – both I and aVF (+) Right axis deviation – lead I (-) and aVF (+) Causes: Normal finding in children and tall thin adults Right ventricular hypertrophy Chronic lung disease even without pulmonary HTN Anterolateral myocardial infarction Left posterior hemiblock Pulmonary embolism Wolff-Parkinson-White syndrome – left-sided accessory pathway Atrial septal defect Ventricular septal defect Left axis deviation – lead I (+) and aVF (-) Causes: Left ventricular hypertrophy Inferior myocardial infarction Artificial cardiac pacing Emphysema Hyperkalemia TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 8 of 16 Step 4: P-R INTERVALS FOR AV BLOCK A-V Block First-Degree AV conduction lengthened May be seen in normal individuals Usually caused by drugs such as -blockers (metoprolol, atenolol, propanolol), Ca2+ channel blockers (verapamil, diltiazem) that can prolong the AV conduction Associated with the ff: coronary artery disease acute rheumatic carditis Beta blockers digitalis cardiomyopathy normal sinus rhythm prolonged PR interval (>1 big square or 0.2s) o delay from SA node firing and spread of impulses to AV node Mobitz type I (Wenckebach) P-R intervals become progressively longer until one P wave is totally blocked and produces no QRS. After a pause, during which the AV node recovers, this cycle is repeated. Rate: depends on rate of underlying rhythm Rhythm: irregular P waves: normal (upright and uniform) PR interval: progressively longer until one P wave is blocked and a QRS is dropped QRS: normal (0.06-0.10 sec) A-V Block Second Degree sudden dropped QRS absence of QRS after 1 P-wave Mobitz type II no gradual prolongation (PR-PR-PR-dropped QRS) more dangerous and indicates excessive damage to AV node AV Block Third Degree When there is complete dissociation between P wave and QRS (Atrioventricular dissociation) QRS occurs independently whenever it wants to Atrial rate and ventricular rate are not the same Indication for pacemaker TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 9 of 16 Hyperkalemia Hypothyroidism Hypermagnesemia Adrenal insufficiency Drug-related Beta blockers Adenosine Ca channel blockers Anti-arrythmics (class I & III) Digitalis Lithium Infectious Endocarditis Tuberculosis Lyme disease Diphtheria Chagas disease Toxoplasmosis Syphilis Dengue fever Heritable/congenital Congenital heart disease Maternal SLE Kearns-Sayre syndrome Emery-Dreiffus MD Myotonic dystrophy Progressive familial heart block Inflammatory SLE MCTD Rheumatoid arthritis Scleroderma Infiltrative Amyloidosis Hemochromatosis Sarcoidosis Coronary artery disease Acute MI (esp. inferior wall MI or R Coronary a. involvement) Neoplastic/traumatic Lymphoma Radiation Mesothelioma Catheter ablation Melanoma Degenerative Lev disease Lenegre disease Step 5: ECTOPIC BEATS Atrial vs. Ventricular Ectopy Causes of AV blocks Autonomic Carotid sinus hypersensitivity Metabolic/endocrine TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 10 of 16 Step 6: CHAMBER ENLARGEMENT Premature Atrial Contraction (PAC) Originates from the atria; an independent focus decided to fire a few msec ahead of the expected beat and override or insert into the sequence of the P-wave firing Not coming from the SA node The following QRS is narrow With P-wave Left Atrial Enlargement P wave duration equal or more than 0.12 sec. Notched, slurred P wave in lead I and II (P mitrale). Biphasic P wave in lead V1 with a wide, deep and negative terminal component. Premature Ventricular Contraction (PVC) No P wave Wide QRS With gap Right Atrial Enlargement P wave duration equal or less than 0.11 sec. Tall, peaked, narrow T wave equal or more than 2.5 mm in amplitude in lead II,III or aVF (P pulmonale). Mean P wave axis shifted to the right (more than +70 degrees). TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 11 of 16 Ventricular Hypertrophy Sinus tachycardia, Left Axis deviation, LVH, No PR prolongation, No AV blocks (pic below) Left Ventricular Hypertrophy "Voltage criteria": R or S wave in limb lead equal or more than 20mm S wave in V1, V2 or V3 equal or more than 30mm R wave in V4, V5 or V6 equal or more than 30mm. Depressed ST segment with inverted T waves in lateral leads (strain pattern; more reliable in the absence of digitalis therapy. Left axis of -30 degree or more. QRS duration equal or more than 0.09 sec. Time of onset of the intrinsicoid deflection (time from the beginning of the QRS to the peak of the R wave) equal or more than 0.05 sec in lead V5 or V6. Tall Rs in V5 and V6 Deep S in V1 and V2 Right Ventricular Hypertrophy Tall R waves over the right precordium and deep S waves over the left precordium ( R:S ratio in lead V1 > 1.0) Normal QRS duration (if no bundle branch block) Right axis deviation. ST-T "strain" pattern over the right precordium. Late intrinsicoid deflection in lead V1 or V2. Tall Rs in V1 and V2 Deep S in V5 and V6 TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 12 of 16 Below: normal sinus rhythm (NSR), HR = 88, RA deviation (RAD), R atrial enlargement (RAE), RVH Step 7: QRS DURATION NSR, 80bpm, RAD, PR interval normal, RAE, RVH Sinus tachycardia, RAD, LAE, RVH Left Bundle Branch Block QRS duration equal or more than 0.12 sec. Broad , notched or slurred R wave in lateral leads(I, aVL , V5,V6) QS or rS pattern in the anterior precordium. Secondary ST-T wave changes (ST and T wave vectors are opposite to the terminal QRS vectors). Late intrinsicoid deflection in lead V5 and V6. Wide QRS due to prolonged ventricular depolarization (>0.12; N: 0.08-0.1) V5 and V6 – wide, notched R wave V1 and V2 – deep S wave With P-wave o If w/o P-wave – sinus tachycardia TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 13 of 16 Right Bundle Branch Block QRS duration equal or more than 0.12 sec. Large R' wave in lead V1 (rsR'). Deep terminal S wave in lead V6. Normal septal Q wave. Inverted T wave in lead V1 (secondary T wave changes). Late intinsicoid deflection in lead V1 and V2. Step 8: ST SEGMENT ABNORMALITIES ECG Changes in Acute Ischemia, Injury and Infarction. Typically, three phenomena may occur on the ECG that are characteristic of the evolution of a myocardial infarction (MI): T wave inversion, indicating ischemia. S-T segment elevation, indicating injury and the acuteness of myocardial infarction (MI). The presence of an abnormal Q wave, indicating tissue death (necrosis). The above abnormalities are usually seen in the ECG leads representing the area of damage. TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 14 of 16 Leads I, V5, V6 and AVL ST elevation in I, V5-V6, AVL: acute lateral wall infarction Localization of Infarction Rare V1: tall R Localization of MI through ECG Anterior wall Anteroseptal Inferior Right ventricular Posterior Wall Leads I, V2, V3, V4 V1-V4: Q-wave and ST elevation (Anterior Wall infarction); T inversion (Anterior wall ischemia) V1-V6 involement: extensive anterior extending to the lateral wall V1 through V6 V1 through V3 II, III, aVF V4R, V3R V7 through V9 V1 through V3 ( ST depression) Anterior wall Anteroseptal Inferior Right ventricular Posterior wall Anterior wall infarct (V1-V4) Leads V2, V3 and AVF TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 15 of 16 Inferior Wall infarct (V2, V3, AVF) Questions The ECG rhythm is called: a. Sinus bradycardia changing to ventricular tachycardia b. Junctional rhythm with a run of ventricular tachycardia c. Sinus rhythm terminating in ventricular fibrillation d. Sinus bradycardia changing to junctional tachycardia This ECG rhythm is called: a. Sinus arrhythmias b. Atrial fibrillation with ectopic atrial beats c. Sinus tachycardia with ventricular couplets d. Sinus rhythm, with ectopic atrial beats *** Hello 2012! Hello 2nd sem! As usual, hi sa mga Alphan brods and sisses ko—Taktak, Kenji, Tel, Rors, Charm, Tristan and especially sa mga batchmates ko na sina Faith, Jes, Vin, and Mel. Also, sa mga brods and sisses ko from 2013 and 2014, who’ll read this soon. Hi rin sa PPG...so dilemma parin naten kung saan tayo kakain. Lapit na Christmas! Hi sa mga Med, Pedia, Surge, Psych (and ComMed?) groupmates ko—tsismisan ulet lalo na si ‘Dencyo’ hahaha! Happy aral! I hope this helps (though this looks like a photo album. Sorry!) –hayzle GRABE! Good luck sa topic na ito! Isapuso natin ang pag-aaral nito. Magagamit natin ito next year. Goodluck 2012! There are only two questions that human beings have ever fought over, all through history: “How much do you love me?” and “Who’s in charge?” ~Liz Gilbert in E.P.L. Abby *hello to all the hardworking members of 2012 trans4med!! especially to those i worked with in this trans: hayz, abby, and to our leader, senator peaches *hugs to ms cathy, jo, darling vin, grandmere joie, twin monique, therapeutic friend joey-gurl, riese-pieces, my inaanak and tweetmate charmy, melissa marie, sexy jessa, tellyteltel, faith, POLARIS...and a special greeting to my mommy cyll who will be This ECG rhythm is called: a. Sinus rhythm with multifocal premature ventricular complexes (PVCs) b. Sinus bradycardia with ventricular paced beats c. Sinus rhythm with paced ventricular beats d. Junctional rhythm with unifocal PVCs This ECG rhythm is called: a. Junctional rhythm with a premature atrial complex (PAC) b. Sinus bradycardia with a premature atrial complex (PAC) c. Sinus arrhythmia d. Sinus arrhythmia with a PVC getting married next month *to my enchantmates: miriam, queen seon-dok, GA, fake, diyes, ampatuan, los ohos, really?, brake fluid, claire dela fuente, senator, train, elbow, and yamashita: only 5 meetings to go! we made it!! *2012B, please support the vote for your Lantern Queen and escort project by our class officers! Lantern Queen 2010 will be on December 14, UERM Gym, 6pm-10pm * Regina Iustitiae Sorority, Ateneo Law, in cooperation with Phi Alpha Sigma Sorority and Alpha Sigma Phi Fraternity, are proud to present to you vERdict, the first and biggest medical-law school batch on December 11, 2010 (let's unwind after exams!), 8pm, Ascend Bar, The Fort. Tickets are priced at P250, inclusive of drinks *Medicine 2012, we only have four short months to go before we become JIs...let's do this! --ANAtomy amphitheater (inspired by daisy duck ) OMARISM (because you know this was coming...) Alomar: “nung narinig ko na ang lec ay EKG for dummies, i almost left!" This ECG rhythm is called: a. Sinus tachycardia with a PVC b. Atrial fibrillation with rapid ventricular response c. Sinus tachycardia with a PAC d. Sinus arryhtmia with a PVC OMAR: I’m no escort. I’m either the host or the star. Armand has been bugging me about wanting to be an escort again, he claims he is the key to another victory. DELOICIOUS: Ngeeeee... Can you believe this guy? Hahaha! wala na Omar. You have escaped you're rightful throne as the escort of the lantern queen for 2 years! pinoproject mo lang sa ibang lalake kaya kmi nlang ni Glen last 2 years. Pero ngayon, there is no escape my friend CARLOTACIOUS: Sabi ni Omar he is either the host or the star. Pero diba it's not a star. IT'S OMAR! :) kaya yun na ang theme the Lantern natin. Hahaha DELOICIOUS: Tama carlo. At ung mas ok pa. Dba c lanter queen magddescribe ng lantern? eh, what's more, C escort is the lantern!!! wahahahahaha! It's not a star, it's freakin OMAR!!! TRANSCRIBED BY: Hayzle Mallari, Abby Maralit, Ana Aurelia Santos, Carlo Benjamin Tañada Page 16 of 16