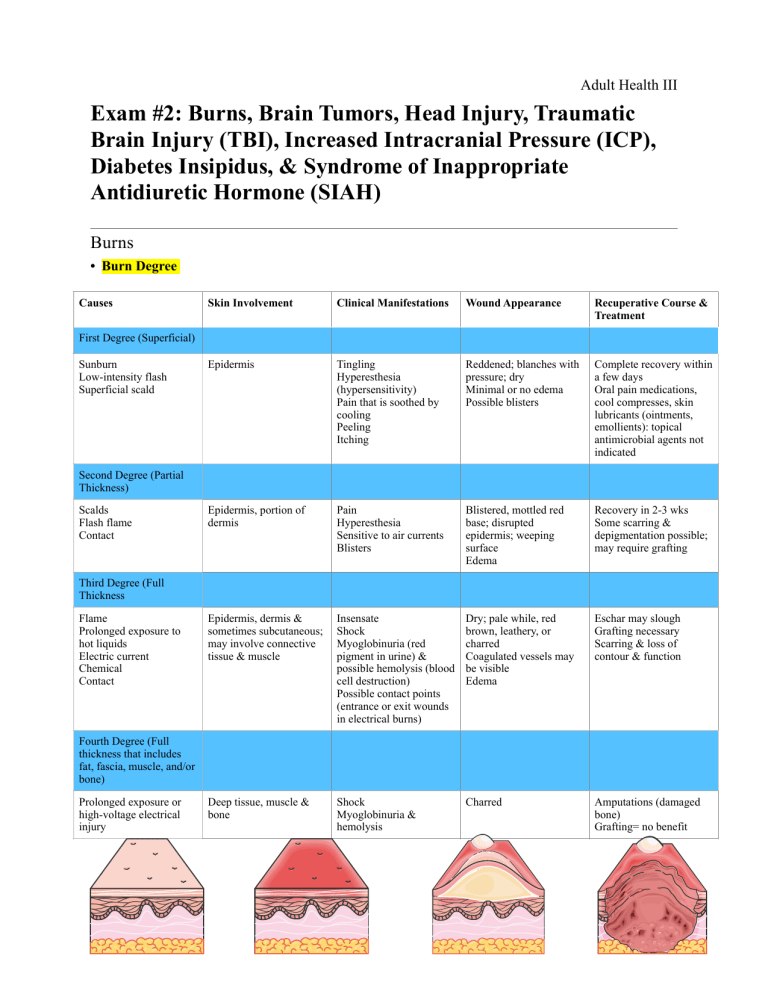
Adult Health III Exam #2: Burns, Brain Tumors, Head Injury, Traumatic Brain Injury (TBI), Increased Intracranial Pressure (ICP), Diabetes Insipidus, & Syndrome of Inappropriate Antidiuretic Hormone (SIAH) Burns • Burn Degree Causes Skin Involvement Clinical Manifestations Wound Appearance Recuperative Course & Treatment Epidermis Tingling Hyperesthesia (hypersensitivity) Pain that is soothed by cooling Peeling Itching Reddened; blanches with pressure; dry Minimal or no edema Possible blisters Complete recovery within a few days Oral pain medications, cool compresses, skin lubricants (ointments, emollients): topical antimicrobial agents not indicated Epidermis, portion of dermis Pain Hyperesthesia Sensitive to air currents Blisters Blistered, mottled red base; disrupted epidermis; weeping surface Edema Recovery in 2-3 wks Some scarring & depigmentation possible; may require grafting Epidermis, dermis & sometimes subcutaneous; may involve connective tissue & muscle Insensate Shock Myoglobinuria (red pigment in urine) & possible hemolysis (blood cell destruction) Possible contact points (entrance or exit wounds in electrical burns) Dry; pale while, red brown, leathery, or charred Coagulated vessels may be visible Edema Eschar may slough Grafting necessary Scarring & loss of contour & function Deep tissue, muscle & bone Shock Myoglobinuria & hemolysis Charred Amputations (damaged bone) Grafting= no benefit First Degree (Superficial) Sunburn Low-intensity flash Superficial scald Second Degree (Partial Thickness) Scalds Flash flame Contact Third Degree (Full Thickness Flame Prolonged exposure to hot liquids Electric current Chemical Contact Fourth Degree (Full thickness that includes fat, fascia, muscle, and/or bone) Prolonged exposure or high-voltage electrical injury 1 of 12 Adult Health III • Types of Burns • Chemical- toxic substance on skin • Inhalation injury increases • #1 priority: remove chemical from skin (copious water irrigation) • Thermal- heat • Ex: fire, boiling water, stove, curling iron, steam • Depends on time that contact occurred • Electrical • Iceberg effect- cannot see the damage to bone & muscle under skin • Can cause damage to: heart muscle (cardiac death can occur due to ventricular tachycardia & dysrhythmias), bone fractures (assess cervical spine), acute tubular necrosis (occurs when myoglobin & hemoglobin clogs the kidneys causing acute kidney injury or kidney failure) • Nursing interventions: there is an open & exit wound, refrain from touching due to electricity, attach to EKG (be cautious!) • Inhalation- airway concern • A visible sign is soot (smoke from fire) in the airway leading to respiratory arrest • Diagnosis: bronchoscopy • S&S: dyspnea, respiratory distress, facial burns, swelling of oropharynx, & nasopharynx, singed nose hairs, flaring nostrils, hoarse voice, tachycardia, agitation, anxiety, bloody sputum, tachypnea • Nursing interventions: EMT will bring pt on O2, when arrive to hospital pt will be intubated • Rule of Nines Parkland Formula: ‣Volume of Lactated Ringers solution equation: ‣ 4 mL x BSA (%) x weight (kg) ‣ Give half of the solution for the first 8 hrs ‣ Give the other half of the solution for the next 16 hrs Example: 1. Calculate the fluid restriction for a patient who weighs 70 kg and has a 50% total body surface area burned. 4 x 50% x 70 kg = 14,000 mL in 24 hrs 14,000 mL/2 = 7,000 for 1st 8 hrs & 2nd 16 hrs 2. How many mL per hour will they receive? 7,000 mL/8 hrs= 875 mL/hr 7,000 mL/16 hrs= 437 mL/hr 3. How many mL will the patient receive on the 4th hour? 875 mL/hr x 4 hr = 3,500 mL 4. How many mL will the patient receive on the 14th hour? For the 1st 8 hrs, pt is receiving 7,000 mL 7,000 mL + 437 mL/hr (6 more hrs)= 9,622 mL ★ Divide % by 2 if half of body part was burned • Complications • Cardiovascular • Hypovolemic shock (hypotension, tachycardia, decreased cardiac output, & dysrhythmias) due to plasma volume loss & results in decreased perfusion, O2 delivery to organs & tissues 2 of 12 Adult Health III • • • • • • • • Causes electrolyte abnormalities: hyponatremia, hyopkalemia, hypochloremia, hypomagnesemia • Diagnosis: BMP (basic metabolic panel) Fluid imbalance • Edema forms rapidly after a burn injury • Treatment for edema: • Elevation of extremity • In severe cases of edema: • Cutting the eschar (dead tissue) via escharotomy (surgical incision through eschar) to relieve pressure • Decompression of edema formation via fasciotomy (surgical incision through fascia to relieve constricted muscle) to restore tissue perfusion • How do to you know it was successful?: palpate pulses, capillary refill, assess skin color Respiratory • Upper airway burns vs. lower airway burns • Upper airway injury (above the glottis) • Results in obstruction • Severe upper airway edema from direct thermal injury or secondary edema from face & neck burns • Protective intubation may be used to maintain patency of airway • Lower airway burns (below the glottis) • Inhalation of incomplete combustion or noxious gases is the source of death at the scene of a fire leading to bronchoconstriction (may administer bronchodilators) • Pulmonary edema occurs EMERGENCY: Carbon monoxide poisoning- carbon monoxide combines with hemoglobin • and displaces oxygen resulting in tissue hypoxia (CO is colorless, odorless, & tasteless) • Diagnosis: Carboxyhemoglobin > 15% • S&S: SOB, headache, vertigo, confusion, mucous membrane irritation, bradycardia, hypotension, change in LOC, bright cherry color to skin or lips • Treatment includes: 100% oxygen on non-rebreather to displace the CO molecules bound to hemoglobin Gastrointestinal • Impaired motility & absorption, vasoconstriction, loss of mucosal barrier function with bacterial translocation, increased pH • 3 of the most common GI alterations: paralytic ileus, Curling’s ulcer (gastric erosion), & translocation of bacteria • Pt with larger burns are at increased risk for life-threatening abdominal compartment syndrome • Leads to abdominal organ ischemia • Nursing interventions: NO elevation of extremities if compartment syndrome, inform physician immediately! Renal • Renal function altered as a result of decreased blood volume post-burn injury • Acute tubular necrosis (acute kidney injury)- occurs when myoglobin & hemoglobin clogs the kidneys causing acute kidney injury or kidney failure • Vasoconstriction Altered thermoregulation • Hypothermia in early hrs after injury due to TBSA (% burned) involved, the IV resuscitation fluids administered, & exposure to air (pt may be shivering) Immunodepression • Skin is the largest barrier to infection & lots on inflammation • Decreased WBCs Hypermetabolism (increases risk for infection & slowing healing time) • Nutrition should be provided ASAP (this helps decrease catabolism), pt may need an NG tube 3 of 12 Adult Health III • Carbohydrates= most important energy source for pts who were severely burned • When oral route is used, high-calorie meals, high protein, low fat & supplements are given (milkshake, pasta with cheese, etc.) • TPN is also an option • Thrombocytopenia may occur • Wound Debridement • What is it?: Removal of dead or devitalized tissue • The goals: • Prepare for grafting and wound healing (medicate pt with morphine before debridement) • Removal of bacteria, foreign bodies • 4 types of debridement: 1. Natural debridement- the dead tissue separates from the dead tissue spontaneously 2. Mechanical debridement- removal of dead tissue with tools • Wet-to-dry dressings are not advised for burn because it can remove epithelial cells along with dead tissue 3. Chemical debridement- topical agents help to remove dead tissue 4. Surgical debridement • Pt is at increased risk for bleeding • Wound Grafting • Who is a good candidate?: Pt w/ deep partial or full thickness burns • Autografts- covering burn wounds with pt’s own skin • Homografts/allograft- pieces of skin obtained from recently deceased or living humans other than the patient • Xenografts/heterografts- skin taken from animals (usually pigs) • These are usually not good options because body may reject the graft • Care of the graft site: • Protect & immobilize for 3-7 days • Occlusive dressings encased in bulky gauze are common to immobilize graft & support the humid environment • First dressing change occurs in 3-5 days after sx • Pt should be positioned frequently to avoid pressure on the graft • Nursing Interventions for Burns Immediate Primary Survey of Patient • Initial treatment (field)- EMS: Assess ABCDEs (pg. 1873): 1. Remove pt from the source of injury & stop burning process while preventing injury to ‣ This occurs in initial treatment (field)-EMS rescue ‣ A: Airway with consideration given to protecting 2. Assess for ABCDEs while establishing airway, the cervical spine supplying O2 (100% O2 on non-rebreather if CO ‣ B: Breathing or gas exchange poisoning is suspected) ‣ C: Circulatory & cardiac status 3. Covering wound with a sterile dry cloth/clean ‣ D: Disability including neurological deficit’s blanket to conserve body heat ‣ E: Examine or expose while maintaining a warm 4. Inserting at least one large bore IV catheter for environment fluids (16-18 gauge) inserted ‣ Seconding survey focuses on: • Emergent/resuscitative phase (lasts 24-48 hrs): ‣ Obtaining a hx • Fluid replacement (give fluid resuscitation ‣ Completion of the total body systems assessment when TBSA (% of body that is burned) is > ‣ Initial fluid resuscitation 20% ‣ Provision of psychosocial support of the • Lactated ringers (LR) administered per order conscious pt to prevent hypovolemia shock & provide electrolytes • Daily weights & labs in the resuscitation period to monitor fluid status 4 of 12 Adult Health III • Strict monitoring of I&Os • How do you assess the efficacy of fluid replacement? • BP is increasing, HR is decreasing, cap refill is < 3 seconds, pulses present, electrolytes are WNL (BMP), urine output of 60 mL/hr, MAP > 65 mmHg • Pulmonary complications • Maintain patent airway Overview of Phases in Burn Management: • Administer O2 as needed • Encourage the pt to cough to remove secretions ‣ Emergent (onset of burn injury) • Intubation needs to be done for inhalation & ‣ Primary survey: ABCDEs burns to the chest, neck & face! ‣ Risk for: hypovolemic shock, respiratory • Cardiovascular distress, compartment syndrome • BMP (basic metabolic panel) ‣ Focus on: wound assessment • BP cuff on unaffected extremity ‣ Acute (capillary permeability stabilized) • If burns everywhere, place a clean dressing ‣ Focus on: preventing infection, alleviating before applying the BP cuff pain, ensuring proper nutrition, & wound • Assess peripheral pulses via Doppler or palpation care • Elevation of burned extremities above the level ‣ Rehabilitative (burn healed, pt able to of the heart if edema occurring function again) • GU ‣ Focus on: emotional support, ADLs, PT, • Insert urinary catheter OT, dietician, RT, cosmetic correction • > 60 mL/hr is required (urine output is most non-invasive assessment for cardiac output & tissue perfusion) • Acute/intermediation phase: • Wound care & closure • Gentle cleaning with mild soap, water & a washcloth • Hair should be clipped or trimmed short • Assess for skin breakdown, redness, & infection • Assess for hypothermia, water should be warm when cleaning pt • After topical ointment applied, the wound is covered in several layers of dry dressings with lighter dressing over joints for mobility • Burns to the face may be left open to air once cleaned • Occlusive dressings, bulky gauze, & a topical antimicrobial agent may be used over areas with new skin grafts to protect the new graft • Preventing infection • Keep area clean & dry • Assess for drainage, redness, etc. • Visitors cannot bring fresh flowers, plants, & fruits • Nutritional management • Family members should be encouraged to bring nutritious & favorite foods • High-calorie nutritional supplements, vitamins, & mineral supplements • If caloric goals cannot be met by oral feeding, a feeding tube (dobbhof or NG tube) may be inserted or IV TPN • Pain management • Frequent pain assessment & administer morphine if ordered PRN • Oral antipyretic agents (helps with itching), frequent lubrication with water or silica-based lotion • If patient is itchy, they should “pat, don’t scratch” • Rehabilitation phase: • Major goals • Increased mobility & participation in ADLs • Adaptation & adjustment to alterations in body image, self-concept & lifestyle • Increased understanding & knowledge of injury, treatment, & follow-up care • Absence of complications 5 of 12 Adult Health III • Functional & cosmetic reconstruction • Nursing interventions • Assess fatigue & pain intolerance related to activities • Schedule rest periods & uninterrupted sleep • Pt should be addressing basic concerns/psychosocial counseling: Will I be disfigured or disabled? How long will I be in the hospital? How can I pay for my care? • Encourage independence • Compression therapy • Consult PT & OT to prevent disabilities (i.e. neuropathic & nerve entrapment, contractures, complex pain) • Medications for Burns ★ Usually administered in 1st & 2nd degree burns Neurology • Brain Tumors • What is it?: Tumor occupies space within the skull resulting in inflammation & compression • S&S: (#1 symptoms) headache, N/V, visual changes, personality changes, change in LOC, hydrocephalus, altered pituitary function, seizures, aphasia • Diagnosis: MRI (gold standard) • Treatment: sx (removal of tumor), radiation, chemotherapy, pharmacological • Craniotomy- the bone flap is returned to its previous location • Craniectomy- the bone flap is not returned • Nursing Interventions for Brain Tumors • Elevate HOB • Assess pain & treat pain • Seizure precautions • Assess gag reflex & ability to swallow Damages to Parts of the Brain (pg. 2033): ‣ Occipital lobe: visual agnosia ‣ Temporal lobe: auditory agnosia ‣ Frontal lobe: learning capacity, memory, or other intellectual functions (leading to limited attention span, difficulties in comprehension, forgetfulness, & lack of motivation) ‣ Motor neurons: hemiparesis, hemiplegia, & a change in reflexes 6 of 12 Adult Health III • In pts with diminished gag response: • Educate pt to direct food & fluids toward unaffected side, having the pt sit upright to eat, offering semisoft diet, & having suction ready • Monitor for ICP • Adequate nutrition • Assess neuro, vitals signs • Encourage independence, reduce anxiety • Head Injury • What is it?: An injury that is the result of an external force that interferes with daily life and prompts treatment • Causes: falls, MVA, assaults • S&S: headache, N/V, visual disturbances, confusion, pupil abnormalities, seizures, abnormal posturing, unsteady gait • EMERGENCY: CSF (cerebral spinal fluid) leak from ears (CSF otorrhea) & nose (CSF rhinorrhea) • CSF is clear/colorless, halos (seen on bedding or gauze; there will be blood in the middle & it will be clear outside) • CSF tests + for glucose when tested using a strip test • Report to PHCP! A meningeal infection can occur if organisms gain access to the fluid via the nose, ear, or sinus! • Diagnosis: CT scan (skull fracture), MRI (brain injury) • Any pt with a head injury is presumed to have a cervical spine injury until proven otherwise • Stabilize spine with a cervical collar until X-ray states otherwise • Primary injury • What is it?: Injury from direct contact to the head/brain causing extra cranial injuries (e.g. contusions, lacerations, external hematomas, concussions, diffuse axonal injury (DAI)) • Secondary injury • What is it?: After the initial injury occurs there is a decreased glucose, O2, & nutrients • Common causes: cerebral edema, hypotension, respiratory depression that may lead to hypoxemia & electrolyte imbalances • Types of injuries/fractures: • Scalp injuries (generally minor injury) • May result in abrasion (brush wound), contusion, laceration, or subgaleal hematoma A large avulsion (tearing away)= life threatening • • Nursing interventions: • Irrigate before it is sutured to prevent infection • Skull fractures- a break in the skull caused by forceful trauma • Basilar skull fractures (priority brain injury if presented in ER) • Battle signs- an area of ecchymosis (bruising will be seen over the mastoid (bone behind ear)) • Raccoon eyes- bruising around eyes • CSF rhinorrhea & CSF otorrhea present (you will see halos) • Do not place an NG tube if CSF rhinorrhea is present! (consider OG tube instead) • Loss of cranial nerve 1 (olfactory) function • Nursing interventions for CSF leak: elevate HOB • Traumatic Brain Injury (TBI) • 5 Types of Brain Injuries: 1. Contusion- brain is bruised & damaged • S&S: loss of LOC, stupor, confusion, headache, pt is aroused with effort but slips back into unconsciousness 2. Types intracranial hemorrhage: 7 of 12 Adult Health III • Hematomas- collection of blood in the brain 1. Epidural hematoma (above the dura) (EXTEME EMERGENCY REQUIRES SX) • S&S: loss of LOC, respiratory arrest, followed by a lucid interval in which the pt is awake & conversant then leads to coma • Treatment: making opening through skull to decrease ICP, remove the clot, & control the bleeding 2. Subdural hematoma (below the dura) • Most common cause is trauma or a rupture of an aneurysm a. Acute SDH • Usually caused by a fall • S&S: changes in LOC, pupillary signs, hemiparesis (one-sided weakness), hypertension, bradycardia, bradypnea, coma • Treatment: immediate craniotomy b. Chronic SDH • Usually develops from minor injuries & is seen mostly in older adults • S&S: intermittent severe headache, alternating focal neurotic signs, personality changes, mental deterioration, focal seizure • Treatment: surgical evaluation for evacuation of the clot 3. Intracerebral hemorrhage & hematoma- blood vessel ruptures within the brain • S&S: headache, neurological deficits • Causes: hypertension, rupture of aneurysm, intracranial tumors, bleeding disorders, complications of anticoagulant therapy • Treatment: craniotomy • Nursing interventions: control ICP, administration of fluids, electrolytes & antihypertensive meds 4. Concussion- temporary loss of neurologic function with no structural damage to the brain • Usually resolves by itself in 1-3 weeks, pt should rest! • These S&S are red flags indicating the need for further intervention: decrease in LOC, worsening headache, dizziness, seizures, abnormal pupil response, vomiting, irritability, slurred speech, numbness or weakness in the arms or legs • Chronic traumatic encephalopathy- repeated concussive incidents (occurs most often in pts who participate in football & boxing) • S&S: personality changes, memory impairment, speech & gait disturbances • Nursing intervention: pt CAN go to sleep, monitor closely for change in LOC (educate pt & family members, pt can go home), tell family to wake up pt every 2 hrs 5. Diffuse Axonal Injury (DAI)- widespread shearing & rotational forces that produce damage throughout the brain • S&S: immediate coma, decorticate & decerebrate posturing, global cerebral edema • Diagnosis: CT & MRI scan • Nursing Interventions for TBI • Administer medications: 8 of 12 Adult Health III • NSAIDS (ex: acetaminophen) for pain • Opioids are not good pain relievers because it may cause drowsiness in a pt with a head injury therefore making it difficult to know whether the pt is tired from the opioid or the head injury • Hypertonic fluids (3% NaCl, 5% NaCl) • Uses: Helps draw fluids in the intravascular space, which helps decrease swelling in brain • Pentobarbital (sedative) • Uses: decreases metabolic demands • Anticonvulsants (prevent seizures) • Elevate HOB 30 degrees or higher (keep head neutral!) • Cluster care/avoid noxious stimuli (e.g. hyperventilating, suctioning pt, blowing nose, coughing, sneezing) • Maintain normal body temp • Monitor respiratory status & maintain patent airway • Monitor neuro status • Seizure precautions (padded bed rails, loosen tight clothes, turn to side, remove jewelry, have suctioning ready) • Monitor for CSF & test for glucose (place a 2x2 gauze underneath nose to observe CSF but DO NOT CLOG NOSE!) • Inform pt & family about the possible behavior changes that may occur • Increased Intracranial Pressure (pg. 2050) ( MEDICAL EMERGENCY ) • As the damaged brain swells with edema or as blood collects within the brain, an increase in ICP occurs • Causes: head injury, bleeding in brain, tumors, infections, stroke • Prevention: stop secondary injury & maintain cerebral oxygenation • ICP normal levels: 0-15 mmHg (if ICP increases & does not decrease, notify physician) • If reading is 0 check the equipment & report to physician • S&S: (#1 symptom) change in LOC, agitation, slowing of speech, delay in response to verbal suggestions, confusion, increasing drowsiness, restless, • Getting worse when pt is is coma, decortication (pt flexes 1 or both arms on the chest & may extend legs stiffly), decerebration (client stiffly extends 1 or both arms & possibly the legs), or flaccidity • Sudden vomiting (emesis) without nausea & sudden change in LOC= REPORT TO HCP! • Late deadly signs: Cheyne-stokes respirations (rhythmic respirations, with periods of apnea), nuchal rigidity (pt cannot flex chin toward chest), Babinski reflex (toes fan out when stimulated), seizures, coma • Complications: diabetes insipidus, syndrome of inappropriate antidiuretic hormone, brain stem herniation • EMERGENCY: Brain herniation- downward movement of brain tissue due to cerebral edema • S&S: fixed and/or dilated pupils (late sign), decreased LOC, abnormal respirations, abnormal posturing, hyperthermia • Cushing’s triad (late sign)- systolic hypertension/wide pulse pressure (i.e. BP: 180/75), bradycardia, irregular breathing (bradypnea) • This occurs when brain herniation is about to occur • Monroe-Kellie hypothesis/doctrine 9 of 12 Adult Health III • What is it?: Due to limited space for expansion within the skill, an increase in any one of the components causes a change in the volume of the others (e.g. displacing or GCS Score: shifting CSF, increasing the absorption or diminishing the production of CSF, or decreasing cerebral blood volume) ‣ What is being assessed?: Eye opening, • Diagnosis: CT & MRI verbal response, motor response • Treatment: craniotomy (removal of bone flap that is later ‣ 15= highest/bestest score returned), ventriculostomy (drain fluids from ventricle of ‣ 8= intubate brain into a collecting device) ‣ 3= lowest score • Nursing interventions: ‣ REPORT decreasing GCS score! • Neuro assessments q 15 min • Administer mannitol IV to reduce cerebral edema • SE: edema (drains fluid from brain to peripheral areas), HF, fluid overload, bibasilar crackles, pulmonary edema, increased BP • Administer hypertonic solutions (3% NaCl, 5% NaCl) • Monitor for seizures & place pt on seizure precautions (can give seizure medications) • Cluster care/avoid noxious stimuli (e.g. hyperventilating, suctioning pt, blowing nose, coughing, sneezing) • Inform pt to not blow their nose if drainage occurs (place a 2x2 gauze underneath nose to observe CSF but DO NOT CLOG NOSE!) • Give sedation as ordered to prevent agitation (benzodiazepine) • Neck should be parallel/neutral with body (use pillows) to allow extra fluid to drain properly • Limit fluid intake, monitor strict I&Os • Elevate HOB (30 degrees or more) • Monitor electrolyes, VS • Administer TPN IF hypoactive bowels • Give food IF they can eat & bowel sounds present Diabetes Insipidus (DI) vs. Syndrome of Inappropriate Antidiuretic Hormone (SIAH) • Diabetes Insipidus (DI) “Dried inside” • What is it?: Hyposecretion of ADH by posterior pituitary; in renal DI, posterior pituitary is producing ADH but the kidneys do not respond • Causes: damage to brain (tumors, trauma, sx, ICP) • S&S: diuresis or polyuria (HIGH urine output), polydipsia (thirsty) [pt drinks a TON of cold water], dehydrated (dry mucosa, decreased skin turgor, & cracked skin), hypotension, tachycardia, seizures, coma • Labs you will see in DI: • Hypernatremia (Na+ in pt: > 145+) (Normal Na+: 135-145 mEq/L) • Low specific gravity (Specific gravity in pt: < 1.005) (Normal specific gravity: 1.005-1.030) • Hyperosmolaity • Diagnostics: Fluid deprivation test, BMP, urine osmolarities, specific gravity • Fluid deprivation test (withhold fluids for 8-12 hrs) • Pt will continue to have high UO regardless of holding fluids & weight will continue to decrease • Inability to increase specific gravity/osmolality = DI confirmed • Medications to treat DI: • Desmopressin (DDAVP) (sub-q, IV, intranasally, or PO) & Vasopressin • Uses: Decreases UO, increases BP • CAUTION W/ CAD PT! • SE: headaches (CAUTION, #1 priority), hyponatremia which can lead to seizures & death!!, confusion, agitation, water intoxication/fluid overload (too much fluids), SOB 10 of 12 Adult Health III • If DI is caused by a renal issue: administer thiazide diuretics, stop Na+ intake, & administer prostaglandin inhibitors • Nursing interventions: • Close monitoring of I&Os, daily weight, urine & BMP (electrolyte levels), neurological status • Pt needs to drink 2-20 L of fluid daily, IV isotonic fluids, monitor for dehydration • Limit Na+ intake • Syndrome of Inappropriate Antidiuretic Hormone (SIAH) “Soaked inside” • What is it?: Excessive secretion of ADH from the posterior pituitary gland • Generally self-limiting & treatment is focused on eliminating underlying cause • Causes: damage to brain (trauma, sx), sepsis, infections of brain (meningitis), pneumonia, lung cancer • S&S: low urine output, sticky & thick urine, hypertension, tachycardia (seizures, headaches, confusion (due to hyponatremia)), cerebral edema (may also cause seizures), weight gain, edema, change in LOC/mental status changes, N/V • Labs you will see in SI: • Dilutional hyponatremia (Na+ in pt: < 135) (Normal Na+: 135-145) • High specific gravity/osmolarity (Specific gravity in pt: > 1.030+) (Normal specific gravity: 1.005-1.030) • Hypoosmolaity • Diagnostics: labs (BMP), specific gravity, osmolarities • Medications to treat SI: • Severe cases: careful IV administration of 3% hypertonic saline (NaCl (3%)) (the only exception to fluids) when S&S of hyponatremia occurs • Thiazide diuretics to reduce hypervolemia & level Na+ • Chlorpropamide • Democlocycline • Nursing interventions: • Close monitoring of I&Os, daily weight, urine & BMP (electrolyte levels), neurological status • Elevate HOB < 10 degrees (helps venous return) • Monitor a change in neuro status • Monitor for ICP • Seizure precautions (padded bed rails, loosen tight clothes, turn to side, remove jewelry, have suctioning ready) • Limit all fluids < 800 mL per day! (IV & PO) 11 of 12 Adult Health III YOU NEED TO KNOW THIS!! 12 of 12