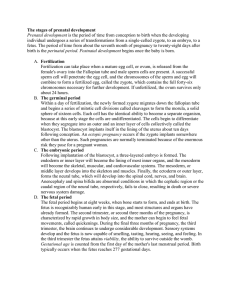
ANTENATAL CARE Case Scenario Farah 22 years old lady came to MCH center, accompanied with her mother in law, complains from nausea, fatigue, and missed period. LMP 15/7/2021 Antenatal period: Time of physical and psychological preparation for birth and parenthood. (time between conception and the onset of labour ). Antenatal care: Care provided to improve the health of the pregnant woman and her baby by monitoring the progress of the pregnancy and detecting and managing any problems. Pregnancy span 9 month ,but health care provider use concept of lunar month, which last 280 days, or 40weeks . First trimester last from 1 to 13 weeks . Second trimester last from 14 to 26 weeks. Third trimester from week 27 through 40. The purpose of antenatal care are to: Establish baseline of present health. determine the gestational age of fetus. Monitor fetal development. Identify women at risk for complication. Minimize the risk of possible complication by anticipating and preventing problem before they occur. Provide time for education about pregnancy, lactation and newborn care Diagnosis of Pregnancy Pregnancy may be assumed based on the presence of certain signs and symptoms: Presumptive signs are subjective and recorded under the history of present illness Probable and positive signs of pregnancy are objective and recorded as physical assessment findings Urine pregnancy test: Reacts with human chorionic gonadotropin (hCG), Performed on first voided urine sample of the day; positive approximately 4 weeks following the first day of the last menstrual period Serum pregnancy test: Useful in monitoring expected pattern of progression of hCG; detects hCG as early as 9 days post-conception Ultrasound: Confirms presence of gestational sac, and fetal, cardiac activity, Validates location of pregnancy (intrauterine versus ectopic) Estimate Date of Delivery Establishing an accurate date of delivery is important to: Determine timing of antenatal screening Monitor growth of the fetus Scrutinize timing of delivery ■ Common abbreviations denoting delivery date are: EDD. ………estimated date of delivery EDC. ……… estimated date of confinement EDB. ……… estimated date of birth Naegele’s Rule Formula used to estimate date of delivery Count back 3 months and add 7 days to the last menstrual period (LMP) reported by the patient Example: The patient states that her LMP was April 20th. 20+7/4-3 27/1 The baby is estimated to be due on January 27th of the following year Trimesters of Pregnancy Normally, pregnancy continues for 40 weeks or 280 days 1st trimester: conception until 12 weeks’ gestation 2nd trimester: 13 weeks until 27 weeks’ gestation 3rd trimester: 28 weeks until 40 weeks’ gestation Schedule of Prenatal Visits (low-risk pregnancy) Monthly until 28 weeks’ gestation Biweekly from 28 weeks until 36 weeks Weekly from 36 weeks until delivery Nursing Care with First Prenatal Visit Determine EDD based on LMP. Document current gestational عمر الجنينage. Document baseline vital signs Document height, weight, and body mass index (BMI) Obtain urine specimen and test for presence of: Glucose Negative/Trace Protein Negative/Trace Auscultate fetal heart tones. Fundal height is an indication of uterine size; periodic measurements of the fundal height should correlate strongly with fetal growth. Uterine size increases in pregnancy in a predictable pattern and is measured to gauge fetal growth. Fundal height that is lagging or greater than expected should be further investigated The relationship of the fundus (top part) of the uterus to specific maternal abdominal landmarks is used throughout pregnancy as a gauge to assess fetal growth. The fundal height measurement correlates to the weeks of gestation from approximately 22 to 34 weeks of gestation McDonald’s method Most often, the fundal height is measured with a tape measure. This method is usually initiated at around 22 weeks of gestation. The end of the measuring tape with the zero mark is held on the superior border of the symphysis pubis. Using the abdominal midline as guide, the tape is stretched over the contour of the abdomen to the top of the fundus The measurement (in centimeters) is recorded and equals the weeks of gestation ±2 wks Physical examination: General examination: It should be started at the moment of the pregnant woman walked into the examination room. Perform vital Signs as a baseline. Report any signs of illness health. * Examine the height * Examine the weight * The approximate weight gain during pregnancy is ( 16% - 25% ) from the pre-pregnancy weight. Diagnostic test Blood test : We must detecting the presence of human chorionic gonadotropin ( HCG). It appear in serum as early as 24 to 48 after implantation. Complete blood count. We must check for hemoglobin concentration ,WBC,RBC. Blood typing (include Rh typing). Maternal serum for alpha-fetoprotien this level will be elevated if a neural tube or abdominal defect is present in fetus, low level may be associated with down syndrome and other chromosomal abnormalities. (done in 16-18 week). An indirect coombs test (determination if Rh antibody are present in Rh negative women) Antibody titer for rubella. TORCH. Urinanalysis: Is performed to test for proteinuria, glycosuria and offer screening for asymptomatic bacteriuria (ASB). Glucose challenges is usually done between 24-28 weeks of gestation. Other test : Aminocentesis procedure used to obtain amniotic fluid for analysis may be needed to evaluate the fetus for genetic disorder. Ultrasound It can be used for the following purposes: To diagnose pregnancy as early as 6 weeks gestation. To confirm the presence, size, and location of the placenta and amniotic fluid . To detect any abnormality in the fetus, placenta, amniotic fluid . To establish the presentation and position of the fetus . To predict maturity by measuring of the biparital diameter. Assessment of fetal growth and development: Assess fundal height is used as indicator of fetal growth. From approximately gestational weeks 18-32 ,the height in the fundus in centimeters is approximately the same as the # of week of gestation (± 2GW). Fetal movement ( quickening start 16-20 weeks) To assess the movement ask the mother to lie in a left recumbent position after a meal and record how many movement it should be 4 fetal movement/hr), nurse should instruct the mother to immediately report any change in fetal movement. Fetal heart rate FHR range from 120 to 160b/m . Ultrasound also provide information about wellbeing of the fetus. Abdominal exam (Leopold maneuver) Leopold maneuvers: a four-part clinical assessment method, to determine the lie, presentation, and position of the fetus It is necessary to place a small pillow or wedge under her right or left hip to displace the weight of the fetus off the major abdominal blood vessels. A sustained supine position can interfere with gas exchange between the woman and fetus. An empty bladder is a prerequisite for abdominal assessment. First Maneuver Determine the height the uterine fundus. Determine what fetal part is in the uterine fundus. Will usually indicate the fetal part situated in the fundus; usually a fetal head; infrequently a fetal breech. Nurse faces woman's head Place hands on either side of the fundal area so that the fingers of both hands almost touch each other. Can be palpated above the symphysis pubis between 12 weeks gestation. Reach the level of the umbilicus at about 20 to 22 weeks and reach the xiphoid process at 36 weeks. When the baby engages into the pelvis between 38 and 40 weeks of gestation, the fundal height drops slightly. Press gently and firmly with finger pads. A somewhat hard and roundish shape, which when moved back and forth between the finger pads, also moves the entire fetus usually indicates a fetal breech, A very hard round well defined shape which can be moved back and forth (balloted) usually indicates a fetal head. First Maneuver: Palpation of the Uterine Fundus Second Maneuver(latral palpation) Determines back of fetus along the sides of maternal abdomen) Palpate fetus between two hands Assess on which side is the fetal back or spine and which side has small parts or extremities. Hands should alternately apply pressure against the opposite hand. Third Maneuver pelvic palpation of the uterus - assess the presenting part). Provides information about the presenting part: breech or head(cephalic ). Examiner faces woman's feet Place hands on either side of the lower abdomen with finger pads at the lower uterine pole and thumbs directed toward the umbilicus. Carefully move fingers of each hand towards each other in a downward and inward manner using gentle pressure. Fourth Maneuver (pawlik manouver) Face the woman's head and spread your hand widely apart Grasp the uterine contents just above the symphysis pubis (firmly but gently) Hold presenting part between index finger and thumb Assess for cephalic versus Breech Presentation This maneuver determine if the presenting part is engaged or not Nutrition Inquire about dietary practices Gather 24-hour diet recall Suggest an addition of 300 healthy calories per day Encourage daily prenatal vitamin with 400 micg folic acid Suggest 6–8 glasses of water daily Encourage to follow food pyramid in daily choices Exercise Physical activity in pregnancy is recommended unless contraindicated by medical complications Avoid sports with potential for abdominal trauma or falls Avoid overheating and supine positioning ■ STOP exercise if experiencing Vaginal bleeding Cramping Leaking of amniotic fluid Decreased fetal movement Dizziness Headache Chest pain Calf pain Dyspnea Sexuality in Pregnancy Sex not restricted in pregnancy unless risk factors exist for bleeding or preterm labor Discuss expected changes in sexuality Change in libido Body image changes Braxton-Hicks contractions with orgasm. Education in the Second and Third Trimester ■ Teach patient to count fetal movement and report change in fetal movement pattern. ■ Discuss fetal growth and development. ■ Discuss symptoms of preterm labor. ■ Encourage childbirth preparation class ■ Discuss options for pain control in labor ■ Cesarean preparation class, if indicated ■ Epidural anesthesia class, if indicated ■ Explore preparing for the newborn Danger signs during pregnancy