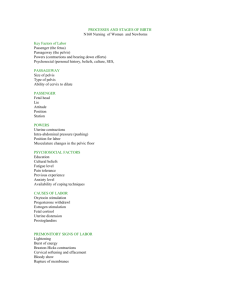
Health people, 2020 has 33 goals related to maternal, infant, and child health. Problems with the health care system - Structure of the Health care delivery system (fragmented and expensive) - Reducing medical errors - High cost of healthcare - Limited access to care - Health care reform Accountable care organizations - An ACO is a group of health care providers and health care agencies that are accountable for improving the health of populations while containing costs - Intended for Medicaid and Medicare services - Coordinate high-quality care, eliminate duplication of services and prevent medical errors Childbirth practices - Preconception care should begin before pregnancy - Hispanic and black receive significantly less prenatal care - Women who choose nurse-midwives seem to participate more actively in childbirth decisions, receive fewer interventions during labor and are less likely to give birth prematurely Gravidity and Parity - Gravida – a woman who is pregnant - Gravidity – pregnancy - Parity – the number of pregnancies in which the fetus has reached 20 weeks of gestation - Preterm – before 37 weeks - Early term – 37-38 weeks - Full-term – 39 weeks - GTPAL (gravity, term, preterm, abortions, living children) Cancer can be one cause of a false positive hCG pregnancy test Signs of pregnancy - Presumptive – subjective changes reported by the woman (amenorrhea, fatigue, breast changes) - Probable – Objective changes assessed by the examiner ( o Hegar sign – Compressibility and softening of the uterus, the cervix is still firm o Goodell sign – softening of the cervix o Chadwick – Violet blue vagina and cervix o Ballottement – tapping the cervix and feeling the fetus bounce back o pregnancy tests). Combined with presumptive signs, these strongly suggest pregnancy - Positive – Objective signs assessed by the examiner that can only be attributed to the presence of a fetus (hearing fetal heart tones, visualizing the fetus, palpating fetal movements) These are definitive signs of pregnancy Changes during pregnancy - HR increases 15-20 beats/min - Blood volume increases 1200-1500mL or 40-45% - Cardiac output increases 30-50% - State of chronic mild hyperventilation - Renal function is most efficient in the lateral recumbent position and least efficient in supine position Naegele’s Rule - Start with the first day of the last menstrual cycle - Add seven days then count forward 9 months - Or subtract three months and add seven days Nutritional requirements - First trimester – pretty much the same as non-pregnant - Second trimester – additional 340 calories - Third trimester – additional 452 calories - Increased need for iron, zinc, iodine (220), magnesium, vitamin C, and folate (600mg) Weight gain - With a normal BMI, women should gain 25-35 pounds during pregnancy (11.5-16kg) True Labor - Contractions regular - Pain felt in back radiating to the front - Cervical changes (most significant indication) - Fetus engages - Change of position doesn’t matter - Bloody show (cervix is changing) Normal fetal HR – 110-160 beats/min Stages of labor - First stage o Early or latent – 1-5 cm, contractions 5-30 minutes, takes about 6-8 hours Distraction Rest and relax Ambulation Slow-paced breathing o Active phase – 6-10 cm, contractions every 2-3 minutes, lasts 3-6 minutes Change positions frequently Empty bladder Hydrotherapy - Needs encouragement Don’t distract Second Stage o Pushing stage o Ferguson reflex (urge to push) - Third o Placenta o Usually takes 10-15 minutes o Given oxytocin to contract the uterus - Fourth o Recovery o 1-2 hours after delivery Stations - Ischial spines are 0 station - More positive = lower down - Negative = higher up Newborn Care assessment - Skin to skin/warmth - Quick assessment - APGAR scoring – activity muscle tone, pulse/heartbeat, grimace reflex irritability, appearance skin color, respirations. Normal 8-9 at 1-2 minutes Five Ps – Factors affecting the process of labor - Passenger: fetus and placenta o Size of the head o Fetal presentation Cephalic, breech, and shoulder LOA is the most preferred and optimal o Fetal lie o Fetal attitude General flexion – chin is flexed on the chest, thighs are flexed on the abdomen, legs are flexed at the knees. Arms are crossed over the thorax and the umbilical cord is between the arms and legs o Fetal position - Passageway: the birth canal - Powers: contractions and maternal voluntary pushing effort o Primary – involuntary contractions Responsible for the effacement and dilation of the cervix and decent of the fetus o Secondary powers – involuntary urge to push Contractions change and become expulsive Have no effect on cervical dilation Occur after the cervix is fully dilated and the baby is ready to be pushed out - Position of mother o Mother should be encouraged to find positions that are most comfortable for her - Psychological response Fetal Lie – relation of long axis of fetus to long axis of mother Fetal attitude – relation of the fetal body to each other – flexion of chin Fetal Position – right or left, presenting part, location in relation to maternal pelvis Signs preceding labor - Lightening – baby drops down into the pelvis, breathing becomes easier, causes pressure in pelvis - Bloody show – cervix begins to open up - Surge of energy - Backache - Return of urinary frequency - Braxton Hicks - Weight loss of .5-1.5kg - Cervical ripening - Possible rupture of membranes Mechanism of Labor - Engagement - BPD reaches pelvic inlet – head is said to be engaged - Descent - Flexion – chin is close to the chest - Internal rotation - Extension – head is delivered - Restitution and external rotation – turns to right or left to get shoulder out - Expulsion Maternal Physiologic Changes During Labor - CO increases 10-15% in first stage and 30-50% during second stage - HR increases slightly in first and second stages - Blood pressure increases during contractions and returns to baseline between contractions - WBC increases - Respiratory rate increases - Temp may be elevated - Proteinuria may occur - Gastric motility and absorption of solid food is decreased (nausea and vomiting may occur) - Blood glucose level decreases VEAL CHOP Variable Cord Compression – shaped like U or W Early Head compression – okay and good sign Accelerations Okay, good sign Late Placental insufficiency Amnioinfusion – used to treat variable decelerations and relieve intermittent umbilical cord compression Interventions for FHR patterns – POISON P - Position change – left side O- O2 – 10 L humidified I - Increase IV fluids – give bolus, usually LR S - Sterile vaginal exam O - Oxytocin off N - Notify the provider Amnioinfusion, tocolytics, fetal pulse oximetry, patient and family education, documentation Pain during labor and birth Neurologic origins - Visceral – Uterine ischemia and pressure - Somatic – Distention and traction on the peritoneum, pressure against the bladder and rectum, stretching and distention of the pelvic floor, lacerations of soft tissue Factors influencing pain response - Physiologic factors o Fatigue o Fetal size o The rapidity of fetal descent o Maternal position and mobility - Culture o May not show reaction to pain o May be stoic o May use indigenous remedies or other non-pharmacological means - Anxiety o Excessive anxiety and fear can magnify pain perception - Previous experience - Gate-Control Theory of Pain o Pain sensations travel along sensory nerve pathways to the brain, but only a limited number of sensations or messages can travel through these nerve pathways one time. Using distraction techniques reduces or blocks the capacity of nerve pathways to transmit pain Non-pharmacologic pain management - Counterpressure (useful on lower back when the fetus is in the posterior position) - Effleurage (light massage) - Walking - Rocking - Changing positions - Application of heat or cold - Transcutaneous electrical nerve stimulation - Acupressure - Water therapy (showers, baths) - Aromatherapy - Breathing techniques - Music - Imagery - Use of focal points - Childbirth education - Hypnosis - Biofeedback Pharmacological pain management - Nitrous oxide - Opioids o Meperidine, fentanyl, remifentanil, and nalbuphine - Nerve block analgesia and anesthesia o 20-30 minute electronic fetal monitoring strip is evaluated o Woman’s fluid balance is assessed, 500-1,000ml of LR or NS may be administered 15-30 minutes before induction of the anesthetic o After administering the anesthetic, maternal blood pressure, pulse and RR need to be assessed every 5-10 minutes o S/S of maternal hypotension with decreased placental perfusion Maternal hypotension (20% decrease from baseline) Fetal bradycardia Absent or minimal FHR variability o Interventions Turn onto lateral position, or place pillow or wedge under hip to displace uterus Maintain IV infusion Administer oxygen with nonrebreather mask 10-12L Elevate legs Notify provider Administer IV vasopressor (ephedrine or phenylephrine) Remain with the woman and monitor every 5 minutes until stable o Nursing considerations for epidurals Baseline vitals Have patient void Hydrate with 500-1000mL LR or NS O2 ready Position in side-lying or sitting on edge of bed Vital signs after procedure o Side effects of epidural Bladder distention Elevated temp Short or long term backache Disruption of labor Increased length of first and second stage of labor Increased use of oxytocin Increased use of instrumentation Increased incidence of C-section