Acute Kidney Injury Case Study: Nursing Assessment & Interventions
advertisement

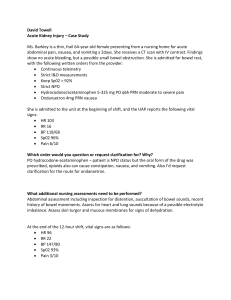
Acute Kidney Injury – Case Study Ms. Thomas is a thin, frail 64-year-old female presenting from a nursing home for acute abdominal pain, nausea, and vomiting x 2days. She receives a CT scan with IV contrast. Findings show no acute bleeding, but a possible small bowel obstruction. She is admitted for bowel rest, with the following written orders from the provider: • Continuous telemetry • Strict I&O measurements • Keep Sp02 > 92% • Strict NPO • Hydrocodone/acetaminophen 5-325 mg PO q6h PRN moderate to severe pain • Ondansetron 4mg PRN nausea She is admitted to the unit at the beginning of shift, and the UAP reports the following vital signs: • HR 103 • RR 16 • BP 118/68 • Sp02 96% • Pain 6/10 Which order would you question or request clarification for? Why? PO hydrocodone-acetaminophen – patient is NPO status but the oral form of the drug was prescribed, opioids also can cause constipation, nausea, and vomiting. Also I’d request clarification for the route for ondansetron. What additional nursing assessments need to be performed? Abdominal assessment including inspection for distention, auscultation of bowel sounds, recent history of bowel movements. Assess for heart and lung sounds because of a possible electrolyte imbalance. Assess skin turgor and mucous membranes for signs of dehydration. At the end of the 12-hour shift, vital signs are as follows: • HR 96 • RR 22 • BP 147/80 • Sp02 93% • Pain 3/10 The nurse recognizes that the patient has not voided all day and assists the patient to the bathroom. The patient voids 200 ml of dark, concentrated urine. What nursing action(s) should be implemented at this time? Who should this information be passed on to? Strict monitoring of intake and output should be passed onto the next nurse. What diagnostic tests would you expect the provider to order? Why? Bladder scan to see if Ms. Thomas is retaining any urine. A renal function panel to assess a possible decrease in kidney function. Provider orders a 500 mL bolus of Normal Saline (0.9%) IV over 1 hour and a renal function panel, which is drawn promptly by the nurse. After 6 hours, Ms. Thomas still has had no further urine output. A bladder scan shows approximately 60 ml of urine in the bladder. A head-to-toe assessment now reveals crackles in Ms. Thomas’ lungs and her Sp02 is 89%. The renal function panel has revealed: • BUN 56 mg/dL • Na 132 mg/dL • Cr 3.6 mg/dL • Ca 7.7 mg/dL • GFR 47 mL/min/m2 • Phos 4.8 mg/dL • K 5.5 mEq/L • Mg 1.4 mg/dL What nursing action(s) should be implemented at this time? Place patient on 1L O2 via nasal cannula to improve oxygen saturation, notify provider of increased BUN, Creatinine, and potassium and of decreased GFR and sodium. What orders should be anticipated from the provider? Diuretics to remove fluids from the lungs and IV infusion to correct dehydration What is going on physiologically with Ms. Thomas at this time? Explain what contributed to the development of this condition. Ms. Thomas developed an acute kidney injury from vomiting for two days causing dehydration with no immediate correction of fluid and electrolyte loss. The provider orders to give 1L bolus of Normal Saline (0.9%) over 1 hour, then 125 mL/hr of Normal Saline continuously. The provider also orders a one-time dose of 40 mg Furosemide IV push and to recheck the Renal Function Panel in 6 hours. Ms. Thomas diuresis approximately 600 mL in 2 hours and her lungs now sound clear to auscultation. Over the next two days, Ms. Thomas’ hourly urine output begins to improve and her BUN, creatinine, and GFR return to normal ranges. Her small bowel obstruction resolves on its own and she is able to begin taking PO food and fluids. What could have been done, if anything, to prevent acute kidney injury for Ms. Thomas? Ms. Thomas should have been given IV fluids upon admission to replenish her fluids and electrolytes that were lost upon two days of vomiting.