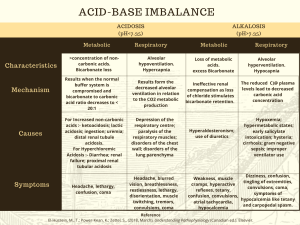
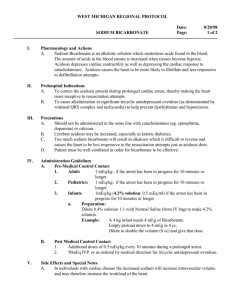
Anaesth Crit Care Pain Med 37 (2018) 495–497 Editorial Treatment of acute acidaemia in the seriously ill patient: Should base be given? A R T I C L E I N F O Keywords: Sodium bicarbonate Severe acidaemia Metabolic acidosis Respiratory acidosis NHE1 Acute severe acidaemia, defined as a plasma pH of 7.20 [1] or 7.15 [2] that is present for minutes to a few days, is associated with decreased hemodynamic function, increased cardiac arrhythmogenicity, increased tissue inflammation, and increased mortality [3]. The critical factors producing the cellular dysfunction with acute acidaemia is a decrement in intracellular pH (pHi) and interstitial pH (pHe) rather than systemic plasma pH alone. Therefore, improving the pH of all three compartments should be a major goal of therapy [4]. The most effective strategy for treatment of acute acidaemia is elimination of the underlying cause such as administration of crystalloid to improve blood pressure and hemodynamic function or treatment of infection in patients with sepsis. However, if this is not possible, or the clinician desires to speed the recovery of acidbase balance, administration of base, primarily in the form of sodium bicarbonate, is often recommended [5]. There remains great controversy about the value of the administration of sodium bicarbonate in acute severe acidaemia [5]. In order for the clinician to make an informed decision about the use of bicarbonate in the treatment of acute severe acidaemia, he/she must understand the rationale for its use, its perceived benefits and limitations, and any alternative therapy available. 1. Causes of severe acidaemia Assuming an appropriate respiratory response, severe acidaemia will be observed when serum [HCO3-] falls below 10 mEq/L. However, many patients with severe acidaemia do not have metabolic acidosis alone, but rather have mixed metabolic and respiratory acidosis [6]. Since the generation and retention of carbon dioxide after bicarbonate administration is a major concern (see below), any impairment in the elimination of carbon dioxide will affect the clinician’s prescription for base administration. Thus, documenting whether metabolic acidosis with appropriate respiratory compensation or a mixed metabolic and respiratory disturbance is present is a critical step in determining whether and how much sodium bicarbonate should be administered. The major metabolic causes of severe acidaemia are lactic acidosis and ketoacidosis; whereas, other high anion gap acidosis such as toxic alcohol poisoning or Tylenol poisoning are uncommon [7]. The non-anion gap metabolic acidosis associated with aggressive administration of chloride-containing solution is frequent, but is generally mild to moderate in degree [8]. Therefore, the overwhelming majority of the information about the use of bicarbonate in the treatment of severe acidaemia has been obtained from studies of lactic acidosis and ketoacidosis. Thus, I will restrict my comments only to the use of bicarbonate in the treatment of these acid-base disorders. 2. Impact of base administration on mortality and haemodynamics In both prospective and retrospective studies in children and adults, bicarbonate did not reduce morbidity or mortality of diabetic ketoacidosis [9]. Similarly, in several of the studies of lactic acidosis in adults published in English, bicarbonate did not reduce mortality [1,6,10]. On the other hand, in a single study published in the Chinese literature, administration of sufficient bicarbonate to raise blood pH to 7.25 as associated with less mortality when the goal of therapy was blood pH of 7.15 [11]. In the recent large multi study of Jaber et al. [1], although sodium bicarbonate did not reduce the composite of mortality at day 30 and at least one organ failure at day 7 (primary outcome), it did reduce the primary outcome when given to a subset of patients with acute kidney injury network scores of 2–3 who were being dialysed (70% vs. 82%). The reason for the benefit of bicarbonate in the treatment of metabolic acidosis associated with severe AKI is unclear. In patients who were dialysed, it might be explained by the ability of dialysis to aid in the control of volume, serum osmolality, and ionized calcium during treatment, factors that might affect the response to sodium bicarbonate therapy. In patients who were not dialysed the reasons behind the benefits of bicarbonate are less clear. Be that as it may, this intriguing finding merits further investigation, and if confirmed would support the use of sodium bicarbonate under these circumstances. Not only did bicarbonate administration not reduce mortality in most of the reported studies, it did not improve hemodynamic function in patients with diverse causes of lactic acidosis more than an equivalent quantity of sodium chloride assessed both at https://doi.org/10.1016/j.accpm.2018.11.005 2352-5568/Published by Elsevier Masson SAS on behalf of Société française d’anesthésie et de réanimation (Sfar). 496 Editorial / Anaesth Crit Care Pain Med 37 (2018) 495–497 30 minutes [12] or 60 minutes postinfusion [13]. Similar studies of diabetic ketoacidosis have not been performed, although a single observational study revealed that spontaneous correction of diabetic ketoacidosis in patients was not associated with any improvement in cardiac contractility [14]. effects of sodium bicarbonate. Indeed, the improvement in cardiac contractility when a selective NHE1 inhibitor is given along with bicarbonate is not different than when the NHE1 inhibitor is given alone [22]. 6. Conclusions and future directions 3. Adverse effects of bicarbonate administration Adverse effects of bicarbonate administration include volume overload, metabolic alkalosis, and cerebral oedema in children with DKA [7]. However, the most important adverse effects reported include: a pH-dependent decrease in the level of ionized calcium [12]; and intracellular acidification of various tissues due to accumulation of carbon dioxide [15]. The inevitability of the latter complication has been questioned, as in some studies infusion of bicarbonate to an acidemic animal or human failed to reduce pHi or even raised it [16]. Unfortunately, the explanation for the discrepant effects were not clear. However, it is postulated that acidification of tissues is more common when large quantities of bicarbonate are administered at a rapid rate. To monitor the presence and the magnitude of this complication, assessment of acid-base parameters in central venous blood is useful [17]. Patients with lactic acidosis can have hypocalcaemia prior to bicarbonate therapy and the hypocalcaemia can be exacerbated with bicarbonate treatment, particularly if alkalemia develops [12]. In this regard, twenty-five percent of patients receiving bicarbonate for the treatment of acute acidaemia in the study of Jaber et al. [1] developed hypocalcaemia. The potential success of the prevention of hypocalcaemia and tissue accumulation of carbon dioxide following bicarbonate infusion to allow the positive effects of bicarbonate therapy to be expressed was shown by studies of rats with acute lactic acidosis in which both alterations were prevented: this resulted in improved cardiac contractility and vascular responsiveness to catecholamines [18]. In summary, bicarbonate administration to non-dialysis patients with lactic acidosis or diabetic ketoacidosis does not reduce mortality or improve cardiovascular function. As noted, this might be attributed to tissue accumulation of carbon dioxide and hypocalcaemia during treatment. Therefore, their minimization or prevention might allow more of the positive effects of bicarbonate administration to be expressed. 4. Additional bases for treatment of acute acidaemia Other bases that were designed to avoid tissue accumulation of carbon dioxide with their administration have been studied. THAM (tris-buffer) raised plasma [HCO3-] and pH in patients with lactic acidosis and was not associated with carbon dioxide retention in patients with combined metabolic and respiratory acidosis [19]. Also, carbicarb1 a 1:1 mixture of sodium bicarbonate and disodium carbonate improved acid-base parameters and cardiac function in animal studies, but not in studies of humans [20]. Both agents are presently not being manufactured. 5. Other mechanisms of cellular injury as targets for treatment Activation of the myocardial sodium hydrogen exchanger NHE1 with lactic acidosis causes, accumulation of detrimental quantities of sodium and calcium, cellular injury, impaired haemodynamics, and increased mortality in animal models, which can be prevented by treatment with selective NHE1 inhibitors [21]. Administration of sodium bicarbonate can exacerbate this process by reducing the proton gradient against which the sodium-hydrogen exchanger must pump: a potential additional reason to explain the injurious Bicarbonate administration to patients with lactic acidosis and ketoacidosis does not improve haemodynamics or reduce mortality in the majority of clinical and experimental studies. As noted, this failure could be due to hypocalcaemia and accumulation of carbon dioxide with bicarbonate administration and studies in humans to determine whether their prevention is beneficial is warranted. Also, the recognition of the potential role of activation of the myocardial NHE1 and its enhancement by bicarbonate administration in depressing haemodynamics suggests administration of NHE1 inhibitors might further enhance beneficial effects of bicarbonate or other bases. The acidaemia in seriously ill patients is of major concern to the clinician. Developing effective methods of treatment is of critical importance. Although as presently prescribed, bicarbonate might not be beneficial, examination of putative measures to improve its effectiveness or the use of other bases is clearly indicated. Disclosure of interest The author declares that he has no competing interest. Acknowledgements Dr Kraut has a pending patent for treatment of acute metabolic acidosis. References [1] Jaber S, Paugam C, Fulier E, Lefrant JY, Lasocki S, Lescot T. Sodium bicarbonate therapy for patients with severe metabolic acidaemia acidosis in the intensive care unit. Lancet 2018;392:31–40. [2] Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 2013;39(2):165–228. [3] Kraut JA, Madias NE. Lactic acidosis. Engl N J Med 2014;371(24):2309–19. [4] Kraut JA, Madias NE. Lactic Acidosis: current treatments and future directions. Am J Kidney Dis 2016;68(3):473–82. [5] Kraut JA, Kurtz I. Use of base in the treatment of acute severe organic acidosis by nephrologists and critical care physicians: results of an online survey. Clin Exp Nephrol 2006;10(2):111–7. [6] Jung B, Rimmele T, Le GC, et al. Severe metabolic or mixed acidaemia on intensive care unit admission: incidence, prognosis and administration of buffer therapy. A prospective, multiple-center study. Crit Care 2011;15(5): R238. [7] Kraut JA, Madias NE. Metabolic acidosis: pathophysiology, diagnosis and management. Nat Rev Nephrol 2010;6(5):274–85. [8] Gunnerson KJ, Saul M, He S, Kellum J. Lactate versus non-lactate metabolic acidosis:a retrospective outcome evaluation of critically ill patients. Crit Care Med 2006;10(1):R22–32. [9] Kraut JA, Kurtz I. Use of base in the treatment of severe acidemic states. Am J Kidney Dis 2001;38(4):703–27. [10] Fang ZX, Li YF, Zhou XQ, et al. Effects of resuscitation with crystalloid fluids on cardiac function in patients with severe sepsis. BMC Infect Dis 2008;8:50. [11] Chen X, Ye JL, Zhu ZY. The use of sodium bicarbonate in stages the treating hypoperfusion induced lactic acidaemia in septic shock. Chinese Crit Care Med 2013;25(1):24–7. [12] Cooper DJ, Walley KR, Wiggs BR, Russell JA. Bicarbonate does not improve hemodynamics in critically ill patients who have lactic acidosis. Ann Intern Med 1990;112(7):492–8. [13] Mathieu D, Neviere R, Billard V, Fleyfel M, Wattel F. Effects of bicarbonate therapy on hemodynamics and tissue oxygenation in patients with lactic acidosis:a prospective, controlled clinical study. Crit Care Med 1991;19(11): 1352–6. [14] Maury E, Vassal T, Offenstadt G. Cardiac contractility during severe ketoacidosis. N Engl Med 1999;341(25):1938. [15] Levraut J, Labib Y, Chave S, et al. Effect of sodium bicarbonate on intracellular pH under different buffering conditions. Kidney Int 1996;49(5):1262–7. Editorial / Anaesth Crit Care Pain Med 37 (2018) 495–497 [16] Nielsen HB, Hein L, Svendsen LB, Secher NH, Quistorff B. Bicarbonate attenuates intracellular acidosis. Acta Anaesthesiol Scand 2002;46(5):579–84. [17] Adrogue HJ, Rashad MN, Gorin AB, et al. Assessing acid-base status in circulatory failure differences between arterial and central venous blood. N Engl J Med 1989;320(20):1312–6. [18] Kimmoun A, Ducrocq N, Sennoun N, et al. Efficient extra- and intracellular alkalinization improves cardiovascular functions in severe lactic acidosis induced by hemorrhagic shock. Anesthesiology 2014;120(4):926–34. [19] Kallet RH, Jasmer RM, Luce JM, Lin LH, Marks JD. The treatment of acidosis in acute lung injury with tris-hydroxymethyl aminomethane (THAM). Am J Resp Crit Care Med 2000;161(4):1149–53. [20] Leung JM, Landow L, Franks M, et al. Safety and efficacy of intravenous Carbicarb in patients undergoing surgery: comparison with sodium bicarbonate in the treatment of metabolic acidosis. Crit Care Med 1994;22(10):1540–9. [21] Wu D, Kraut JA. Role of NHE1 in the cellular dysfunction of acute metabolic acidosis. Am J Nephrol 2014;40(1):36–42. [22] Wu DY, Kraut JA, Abraham WM. Administration of a NHE1 inhibitor but not sodium bicarbonate improves cardiovascular function and reduces generation 497 of proinflammatory cytokines in piglets with asphyxia-induced cardiac arrest. Pediatr Res 2014;76(2):118–26. Jeffrey A. Kraut MD * Medical and Research Services VHAGLA Healthcare System, UCLA Membrane Biology Laboratory, and Division of Nephrology VHAGLA Healthcare System and David Geffen School of Medicine, Los Angeles, CA, USA *Correspondence. Division of Nephrology, VHAGLA Healthcare System, 11301 Wilshire Boulevard, Los Angeles CA 90073, USA E-mail address: jkraut@ucla.edu