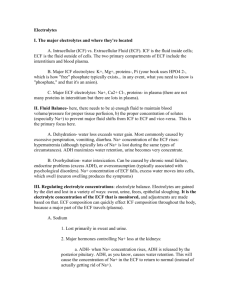
Body Fluids, Electrolytes, & pH Balance: Lecture Notes
advertisement

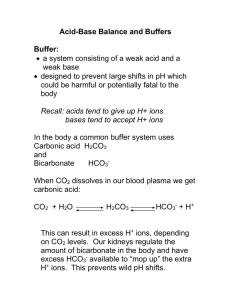
PART 1 Body Fluids – water accounts for nearly the entire volume of body fluids. Normal amount of water in human body ▪ Adult female = 55%, male = 60% ▪ More adipose, less water Distribution Of Water • • Intracellular fluid (ICF) – Inside cells (25 L), 2/3 of body fluids, 40% body weight Extracellular fluid (ECF) – Outside cells (15 L), Interstitial (tissue) fluid, plasma, lymph, etc. Plasma • • • Link between intra and extracellular environments Water is continually exchanged through capillary walls and plasma membranes by Osmosis Water is universal solvent for 2 types of solutes: o Electrolytes – Chemicals that dissociate into free ions (charged) e.g., Na+ (cations), Cl- (anions) o Non-electrolytes – Chemical bonds prevent dissociation, no charge (glucose, lipids, creatinine, urea etc) Electrolyte Pattern Distinct • • • ECF – Na+ (sodium) – main cation (dominant electrolyte to plasma osmolarity) ICF – K+ (potassium) – main cation (dominant electrolyte to intracellular osmolarity) Na+ – K+ pump – maintains these concentrations using active transport (ATP, thus oxygen required) Electrolytes • • Despite these electrolyte differences the osmolarity of ECF and ICF is the same Therefore, so is water concentration Water Balance • • Water intake (2.5 L) = water output (2.5 L) Sources for water intake: Foods and fluids, Metabolic processes (200 mL) Dehydration • • Thirst is driving force – osmoreceptors in hypothalamus detect increase in blood osmolarity (↓saliva) > dry mouth, increase thirst Requires action of angiotensin II and antidiuretic hormone (ADH) to accentuate thirst and reduce urinary loss of water Sources For Water Output - Faeces Expired air from lungs Cutaneous transpiration Sweat Urine production - Kidneys major regulators of body fluid composition Tubular reabsorption of water and electrolytes regulated by hormones – ADH, Aldosterone, Angiotensin, ANP PART 2 Acid-Base Balance of Blood, pH • • • Relative concentration of hydrogen ions [H+] Blood pH = 7.35 to 7.45 (enzymes are pH sensitive) H+ originates from metabolism (lactic acid, carbonic acid) and ingested nutrients (fatty acids, amino acids) pH Maintained by: 1. Buffers 2. Lungs (CO2 and H2O) 3. Kidneys (H+ and H2CO3-) Buffers (Handbag) – chemicals that can regulate pH • • Prevent dramatic changes in [H+] o Act instantaneously o Bind to H+ when pH drops H+ + B- = HB o Release H+ when pH rises HB = H+ + BComposed of a weak acid (H+ donor) and a weak base (H+ acceptor) Major Chemical Buffers 1. Protein buffer system (ICF) • Amino acids can act as weak acid or base o release H+ (acid group) or bind to H+ (amine group) o R group most buffering 2. Bicarbonate buffer system (ECF: plasma) • Mix of carbonic acid H2CO3 (acid=H+ donor) and bicarbonate HCO3- (base=H+ acceptor) • Carbonic acid concentration is regulated by respiration (CO2 and H2O) • Bicarbonate ion concentration is regulated by kidneys (H+ and HCO3-) • Bicarbonate is how we transport CO2 around body • We use this equation to buffer our blood 3. Phosphate buffer system (CSF and urine) Chemical Buffer Systems – can tie up excess acids or bases but only LUNGS and KIDNEYS can eliminate them from body Reversible Chemical Reactions • Symbolized with double-headed arrows CO2 + H2O ↔ H2CO3 ↔ H + + HCO3 - (H+ donor) (H+ acceptor) • Law of mass action determines direction o proceeds from side with greater quantity to less Equilibrium exists reactions when ratio of reactants to products is stable (equal) • DEMONSTRATION Respiratory Mechanisms • • • In healthy people, CO2 is expelled from lungs at same rate it is produced at tissues Thus, H+ does not accumulate and has no effect on blood pH However, if there is a pH change, Chemoreceptor’s in medulla oblongata (brain), adjust your breathing to restore homeostasis within minutes • • With deeper and more rapid breathing MORE CO2 and H+ is expelled, pH rises (alkaline) With shallow and slower breathing LESS CO2 and H+ is expelled, pH decreases (acid) Renal Mechanisms • • • Kidneys ultimate pH regulatory organs o Remove all METABOLIC acids (non-CO2) o Sole regulators of alkaline substances (HCO3-) Tubular secretion or reabsorption of bicarbonate ions (HCO3-), or generate new bicarbonate ions if necessary Takes hours to days to restore pH When blood pH rises (alkaline) • • Hydrogen ions retained by tubular reabsorption Bicarbonate ions excreted (tubular secretion) When blood pH falls (acid) • • • Hydrogen ions excreted, or neutralised by HCO3Bicarbonate ions reabsorbed Thus, urine pH varies (4.5 to 8.0) Compensatory Mechanisms – lungs and kidneys work together to correct pH imbalances