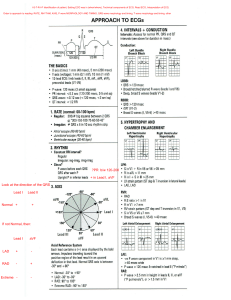
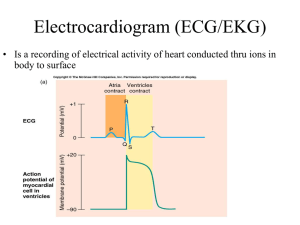
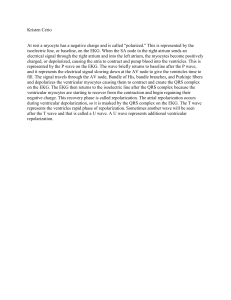
LECTURE 2 à ECG INTERPRETATION CHAPTER 38 Electrical Conduction System Ø Mechanical follows electrical Ø SA node = no stimulus to depolarize o Non-functional SA node (60-100bpm) = AV node (40-60bpm) is a back-up for HR regulation o AV node isn’t working = pacemaker cells in ventricles =purkinjie fibers, back up back-up generators (20-40bpm) à they need pacemaker Phases of the Action Potential Ø Action potential of a cardiac cell consists of five phases Ø Reflects rapid sequence of voltage changes across cell membrane during electrical cardiac cycle Ø Na in, K out (upon stimulus), -90 = resting; stimulus; -90 à +20 Ø 0-1 = depolarization Ø 2-3= repolarization à sodium out potassium in (Na/K pump using energy) + Ca activation Ø 3 = Na/K pump & everything back to normal Ø -70 = threshold for another AP, -70 - -90 = strong stimulus can trigger another depolarization Waveforms Ø A waveform or deflection is movement away from the baseline in either a positive (upward) or negative (downward) direction Ø A waveform that is partly positive and partly negative is biphasic Ø A waveform or deflection that rests on the baseline is isoelectric (flat) Rule of Electrical Flow The ECG Ø When the electrical current travels perpendicular to the lead, the waveform can go in both directions. (Biphasic) Leads Ø Think of the positive electrode as an eye ® The position of the positive electrode on the body determines the portion of the heart “seen” by each lead à electrical activity of heart (if it’s coming towards (via elec. Path) + = positive) Lead I Ø Records the difference in electrical potential between the left arm (+) and right arm (–) electrodes Ø Views the lateral wall of the left ventricle Lead II Ø Records the difference in electrical potential between the left leg (+) and right arm (–) electrodes Ø Views the inferior surface of the left ventricle à follows most natural pathway of heart Electrode Placement for Monitoring Lead II Lead III Ø Records the difference in electrical potential between the left leg (+) and left arm (–) electrodes Ø Views the inferior surface of the left ventricle 1 Summary of Standard Limb Leads Lead Positive Electrode Negative Electrode Heart Surface Viewed Lead I Left arm Right arm Lateral Lead II Left leg Right arm Inferior Lead III Left leg Left arm Inferior Rhythm Interpretation Voltage Ø Voltage is a KEY point in diagnostic ECGs ® 12 lead ECG Ø Voltage is UNIMPORTANT in rhythm recognition ® 3 or 5 lead ECG What do we need to know with interpreting an ECG? 1. What is the rhythm? 2. What is the rate? 3. What is the PR interval? 4. What is the QRS? 5. What is the QT? 6. Interpret the strip………. P Wave à atrial contraction; QRS = depolarization; impulse through ventricles (atria repolarize during QRS, so small we don’t see it) Q Wave à first neg. deflection R Wave à first pos. S Wave à - after R wave à different configurations, QRS measuring = first time leaves baseline to the time it returns to baseline, different patterns, but still QRS, not considered abnormal, timing is key (normal times per wave section) T Wave à REPOLARIZATION Various QRS Configurations J-Point Ø J point - end of QRS complex & beginning of ST segment ST Segment ECG WAVES Ø P wave: the sequential activation (depolarization) of the right and left atria Ø QRS complex: right and left ventricular depolarization (normally the ventricles are activated simultaneously) Ø ST segment Ø T wave: ventricular repolarization ECG INTERVALS Ø PR interval (0.12-0.20s): time interval from onset of atrial depolarization (P wave) to onset of ventricular depolarization (QRS complex) à slowing down of SA to AV node (AV node slows down the impulse, when it starts in the ventricles Ø QRS (< 0.12s) duration: duration of ventricular muscle depolarization, leaving baseline and coming back Ø QT interval (< 0.40s)l: duration of ventricular depolarization and repolarization Ø PP interval: duration of atrial cycle (an indicator or atrial rate) Ø RR interval: duration of ventricular cardiac cycle (an indicator of ventricular rate) Electrical Activity in the Heart 2 Rhythm Interpretation à Regular or Irregular ECG Measurements: The Rate Calculating Heart Rate “Counting Method” Calculating Heart Rate “6 second” Rule Calculating Heart Rate “300 Method” Calculating Heart Rate Irregular Rhythm: measure the fastest and the shortest (count little boxes between R-R and calculate rate by divide 1500/#small boxes which gives you the rate); do this twice with the fastest and shortest interval What is the heart rate? 300 / 6 = 50 bpm Method: measure PR, QRS, QT, Reg/Irregular & HR 3 Measuring QRS Complex Measuring Intervals Measuring ECG Rhythm Strip Rhythm Interpretation Normal Values Ø Normal ranges ® Rhythm: Regular ® Rate: 60-100 ® PR: 0.12 to .20 ® QRS: 0.06-0.12 ® QR: < 0.40 ® QT interval = repolarization (prolonged due to meds, lyte imbalances) Normal Sinus Rhythm Ø Sinus node initiates regular impulses at a normal rate. Each impulse is conducted normally to the ventricles Ø Regularity: Regular Ø Rate: 60–100 beats per minute Ø P Wave: Normal and upright; one P wave in front of every QRS complex Ø PRI: .12–.20 seconds and constant Ø QRS: Less than .12 seconds Sinus Bradycardia Ø Sinus node initiates regular impulses at a slow rate. Each impulse is conducted normally to the ventricles o Athletes, during sleep, increased vagal tone, the valsava maneouvre, hypothermia o Disease states: hypothyroidism, high ICP o S/S: pale cool skin, hypotension, weakness, angina, dizziness, syncope, disorientation, SOB Ø Regularity: Regular Ø Rate: Less than 60 beats per minute Ø P Wave: Normal and upright; one P wave in front of every QRS complex Ø PRI: .12–.20 seconds and constant Ø QRS: Less than .12 seconds; Tx anticholinergics, pacemakers 4 Sinus Tachycardia Ø Regularity: Regular Ø Rate: Greater than 100 beats per minute (usually 100–160 beats per minute) Ø P Wave: Normal and upright; one P wave in front of every QRS complex Ø PRI: .12–.20 seconds and constant Ø QRS: Less than .12 seconds Ø SOB, heart is not filling (cyanotic), chest discomfort (no coronary artery filling time à slow it down, innervate parasymp. Nervous system by bearing down (hold breath, vagal maneuvers if symptomatic) Sinus Arrhythmia Ø Sinus node fires faster during inspiration and slower during expiration, creating an irregular rhythm. Rate is usually normal, Conduction to ventricles is normal o Fever, pain, hypotension, hypovolemia, anemia, hypoxia, hypoglycemia, ischemia, HR, hyperthyroidism, anxiety o Epinephrine, anticholinergics, caffeine, pseudoephedrine o S/S: dizziness, dyspnea, hypotension, increased HR Ø Regularity: Irregular Ø Rate: 60–100 beats per minute (usually) Ø P Wave: Normal and upright; one P wave in front of every QRS complex Ø PRI: .12–.20 seconds and constant Ø QRS: Less than .12 seconds Atrial Fibrillation Ø Many irritable sites within atria fire repetitively, causing ineffective atria l depolarization. AV node blocks most impulses, so ventricular rate is usually slower than atrial; atria does not contract, -25% preload o Underlying heart disease, CAD, HF, pericarditis o Lower CO, no time to fully pump, at risk for thrombi from blood stasis o Tx. B blockers and blood thinners (static blood = clot) § Heparin/coumadin/ digoxin o Atrial contraction = 25% CO (atrial kick) this is lost Ø Regularity: Grossly irregular Ø Rate: Atrial greater than 350 beats per minute; ventricular rate varies greatly Ø P Wave: No discernible P waves; atrial activity is referred to as fibrillatory waves (f waves) (no coordination through atria, multiple irritable focus) Ø PRI: Unable to measure Ø QRS: Less than .12 seconds Idioventricular Rhythm (unknown cause) Ø Regularity: Usually regular (it can be unreliable since it is such a low site) Ø Rate: 20-40 beats per minute; can drop below 20 beats per minute Ø P Wave: None Ø PRI: None Ø QRS: Wide and bizarre; .12 seconds or greater ® Irritable focus at ventricles, QRS takes longer, originating in ventricles instead of atria ® Pacemaker (temp one transcutaneous, mins-hours before OG pacemaker) ® Could be a dying heart Premature Ventricular Contractions Ø An irritable focus within the ventricles fires prematurely to initiate a single ectopic complex Ø Distorts QRS, associated with caffeine, alcohol, nicotine, E, lyte imbalances; usu benign Multifocal PVCs Ø PVCs that are initiated from different foci appear in different shapes from each other o vs. unifocal PVC’s look the same and most likely coming from the same irritable focus 5 Ventricular Tachycardia Ø A single irritable focus within the ventricles fires very rapidly, thus overriding higher sites for control of the heart, 3+ PVCs o Sustained = 30s+, not sustained= <30s Ø Regularity: Usually regular; can be slightly irregular Ø Rate: Usually 150-250 beats/min; less than 150 is called slow VT; over 250 is called Ventricular Flutter Ø P Wave: Not preceded by P waves; dissociated P waves may be seen Ø PRI: None Ø QRS: Wide and bizarre; .12 sec. or greater Ø Tx IV amiodarone if hemodynamic instability Ø VT + no pulse = life threatening, treat like V Fib à Code, CPR; defib + Epi/ Amiodarone Ventricular Fibrillation Ø Multiple foci in the ventricles become irritable and generate uncoordinated, chaotic impulses that cause the heart to fibrillate rather than contract Ø Rate, regularity p wave, PRI, QRS = chaotic with no discernible wavs/complexes Ø Quivering ventricles, no effective contracitons, no CO Ø Occurs in acute MI and myocardial ischemia, CAD, cardiomyopathy Ø CAB (circ, airway, breathing), no pulse = CPR; ACLS, defib Asystole à There is no electrical pacemaker to initiate electrical flow. The heart has lost its electrical activity; check patient, see if lead popped off; children go into asystole more often than adults (usu cause, OD, hyperthermia, tamponade, etc Tx à high quality CPR with ACLS measures (IV/IO access; epinephrine 1mg every 3-5mins, advanced airway, capnography) 12 Lead ECG Ø When someone has chest discomfort they would be having a cardiac event, there are three criteria to determine this ® Hx of cardiac pain (Angina vs. cardiac pain) ® 12 Lead ECG (changes) ® The cardiac markers (rising enzymes) Ø 2/3 = highly suspicious of cardiac issue Ø Rhythm strip does not diagnose, just the rhythm (electrical pathway) Ø 12 lead allows us to diagnose à 12 leads looking at the heart , there are also 3 leads, and 5 leads ® Looking at impulses from 12 different areas Ø Across the bottom (v bottom) is the rhythm interpretation; lead 2, a running strip Leads on R + L arms and legs (limbs) Precordial Leads à looking at left ventricle Lead Groups à V leads = chest leads, surround heart 6 Inferior Wall Ø II, III, aVF; Left Leg; inferior surface (R corn. Art) Inferior MI à highlighted segment is pointing out the inferior surface of the L ventricle Lateral Wall Ø I and aV; Left Arm; Lateral surface of L ventricle Ø V5 and V6; Left lateral chest à both looking at lateral wall, circumflex coronary artery feeds that area Ø I, aVL, V5, V6 Lateral MI à 1, AVL, V5, V6 Anterior Wall Ø V3, V4, Left anterior chest o Left anterior descending coronary artery Anterior MI à V1, V2, V3, V4; septal area, anteroseptal area, big muscular area in L ventricle Septal Wall Ø V1, V2, Along sternal borders, also anterior area 7 AMI Localization AMI Recognition Coronary Arteries & the 12 Lead ECG à understand what blood vessels feed what area, different tx according to which artery and where ST Segment Ø The portion of the ECG tracing between the QRS complex and T wave Ø Represents the early part of repolarization of the right and left ventricles Ø The point where the QRS complex and ST segment meet = “J point” or junction Ø The PR segment used as a baseline from which to evaluate the degree of displacement of the ST segment from the isoelectric line (elevation or depression) Ø ST segment (representing the very early part of repolarization of ventricles is considered: ® Elevated (B) if the segment is deviated above the baseline of the PR segment ® Depressed © if the segment deviates below it ® Above/below à ischemia / lack of perfusion, electrical impulse takes longer/must go a different way AMI Recognition Ø Know what to look for ® ST elevation o > 2mm elevation (two boxes) ® Two contiguous leads (in two/three) Ø Know where you are looking ® You will soon have this memorized Analyzing the 12 lead ECG Ø Look for elevation/depression Ø Group them interior, anterior, lateral Ø Elevation/depression in 2/3 boxes per grouping? 8 The Three I’s Ø Ischemia ® lack of oxygenation ® ST depression or T inversion Ø Injury ® prolonged ischemia ® ST elevation Ø Infarct ® death of tissue ® may or may not show in Q wave ® Q wave ~ 25% size of R wave or S wave (2-3 boxes) Ischemia Ø T wave inversion, ST segment depression Ø Acute injury: ST segment elevation (ischemia) Ø Dead tissue: Q wave Evolving MI and Hallmarks of AMI • • • T wave inversion, ST segment depression Acute injury: ST segment elevation Dead tissue: Q wave (big Q) à Myocardial ischemia -à call it by most significant finding (Q wave) à Open blood vessels to injury/ischemia area to mitigate damage à old MI = q waves, evolution of MI, infarcted tissue is not viable à not seen on rhythm strip, only on 12 lead (has to be in 2/3 leads in that area of heart) EKG Changes: Ischemia → Acute Injury→ Infarction 1. 2. 3. 4. Flipped T waves (takes a year for a flipped t wave to go back to normal) Elevation Q waves Deep Q waves Evolution of Transmural Infarction 9 Look for Grouped Patterns (Footprints) Ø ST Depressions = Ischemia Ø ST Elevations = injury Ø Q Waves & T Wave Inversion = Infarction A Normal 12 Lead ECG (normal) Analyzing a 12 Lead ECG à practice Lateral (Circ.) Inferior (R corn) Anterior (L Descending) 10 11 12